Abstract
Background
Multidisciplinary tumor board (MDT) discussion is standard practice in the management of Upper Gastrointestinal (UGI) cancers. However, poor adherence to MDT recommendations may account for the lack of improved oncological outcomes with MDTs. We aim to quantify adherence rates and compare outcomes between adherent and non-adherent patients.
Methods
We included all patients with potentially curable primary UGI carcinomas who were discussed at UGI MDT from 2017 to 2018. MDT recommendations were compared to actual treatment received. Oncological and survival outcomes were compared between both groups.
Results
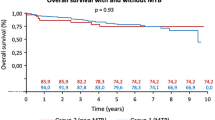
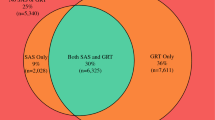
Amongst 153 patients, 64 (41.8%) were non-adherent to MDT recommendations. Reasons for non-adherence were patient refusal (50.0%), treatment-related complications (31.3%), disease factors (17.2%) and clinician decision (1.56%). Univariate analysis showed that non-adherent patients were older (71.6 vs 65.2 years, p < 0.001), with higher clinical stage at point of diagnosis (p = 0.028), pathological stage after resection (p < 0.001) and were more likely to be recommended for multimodal therapy. No significant factors were associated with non-adherence at multivariate analysis. Non-adherent patients had worse median overall survival (19.5 months) compared to adherent patients (not reached at follow-up) with both unmatched and propensity-score matched analysis. Patients who received only part of the intended adjuvant chemotherapy course had worse median overall survival and disease-free survival compared to patients who completed or did not initiate adjuvant chemotherapy.
Conclusions
Non-adherence to MDT recommendations was associated with advanced age and tumor stage, and potentially contributes to the worse oncological outcomes in a group of patients already predisposed to poor outcomes.




Similar content being viewed by others
Data Availability
The datasets generated during and/or analysed during the current study are not publicly available due to institutional guidelines regarding the secure storage of deidentified datasets but are available from the corresponding author on reasonable request.
References
Freeman RK, Ascioti AJ, Dake M, Mahidhara RS. The effects of a multidisciplinary care conference on the quality and cost of care for lung cancer patients. Ann Thorac Surg. 2015;100(5):1834–8; discussion 1838. https://doi.org/10.1016/j.athoracsur.2015.05.056. Epub 2015 Aug 12. PMID: 26276054.
Liu JC, Kaplon A, Blackman E, Miyamoto C, Savior D, Ragin C. The impact of the multidisciplinary tumor board on head and neck cancer outcomes. Laryngoscope. 2020;130(4):946–950. https://doi.org/10.1002/lary.28066. Epub 2019 May 16. PMID: 31095740; PMCID: PMC7868105.
Levine RA, Chawla B, Bergeron S, Wasvary H. Multidisciplinary management of colorectal cancer enhances access to multimodal therapy and compliance with National Comprehensive Cancer Network (NCCN) guidelines. Int J Colorectal Dis. 2012;27(11):1531–8. https://doi.org/10.1007/s00384-012-1501-z (Epub 2012 May 30 PMID: 22645076).
Onukwugha E, Petrelli NJ, Castro KM, Gardner JF, Jayasekera J, Goloubeva O, Tan MT, McNamara EJ, Zaren HA, Asfeldt T, Bearden JD III, Salner AL, Krasna MJ, Das IP, Clauser SB. ReCAP: Impact of multidisciplinary care on processes of cancer care: a multi-institutional study. J Oncol Pract. 2016;12(2):155–6; e157–68. https://doi.org/10.1200/JOP.2015.004200. Epub 2015 Oct 13. PMID: 26464497; PMCID: PMC4960465.
Boxer MM, Duggan KJ, Descallar J, Vinod SK. Do patients discussed at a lung cancer multidisciplinary team meeting receive guideline-recommended treatment? Asia Pac J Clin Oncol. 2016;12(1):52–60. https://doi.org/10.1111/ajco.12421. Epub 2015 Oct 19 PMID: 26481765.
Denton E, Conron M. Improving outcomes in lung cancer: the value of the multidisciplinary health care team. J Multidiscip Healthc. 2016;30(9):137–44. https://doi.org/10.2147/JMDH.S76762. PMID: 27099511; PMCID: PMC4820200.
Wang YH, Kung PT, Tsai WC, Tai CJ, Liu SA, Tsai MH. Effects of multidisciplinary care on the survival of patients with oral cavity cancer in Taiwan. Oral Oncol. 2012;48(9):803–10. https://doi.org/10.1016/j.oraloncology.2012.03.023. Epub 2012 Apr 23 PMID: 22534006.
Friedland PL, Bozic B, Dewar J, Kuan R, Meyer C, Phillips M. Impact of multidisciplinary team management in head and neck cancer patients. Br J Cancer. 2011;104(8):1246–8. https://doi.org/10.1038/bjc.2011.92. Epub 2011 Mar 29. PMID: 21448166; PMCID: PMC3078600.
Rangabashyam MS, Lee SY, Tan SY, Mueller S, Sultana R, Ho J, Skanthakumar T, Tan NC, Tan HK, Soo KC, Iyer NG. Adherence of head and neck squamous cell carcinoma patients to tumor board recommendations. Cancer Med. 2020;9(14):5124–5133. https://doi.org/10.1002/cam4.3097. Epub 2020 May 30. PMID: 32472749; PMCID: PMC7367636.
Yang X, Huang J, Zhu X, Shen K, Zhu J, Chen X. Compliance with multidisciplinary team recommendations and disease outcomes in early breast cancer patients: an analysis of 4501 consecutive patients. Breast. 2020;52:135–145. https://doi.org/10.1016/j.breast.2020.05.008. Epub 2020 May 28. PMID: 32512360; PMCID: PMC7375553.
Samarasinghe A, Chan A, Hastrich D, Martin R, Gan A, Abdulaziz F, Latham M, Zissiadis Y, Taylor M, Willsher P. Compliance with multidisciplinary team meeting management recommendations. Asia Pac J Clin Oncol. 2019;15(6):337–42. https://doi.org/10.1111/ajco.13240. Epub 2019 Sep 10 PMID: 31507069.
Gashin L, Tapper E, Babalola A, Lai KC, Miksad R, Malik R, Cohen E. Determinants and outcomes of adherence to recommendations from a multidisciplinary tumour conference for hepatocellular carcinoma. HPB (Oxford). 2014;16(11):1009–15. https://doi.org/10.1111/hpb.12280. Epub 2014 May 28. PMID: 24888730; PMCID: PMC4487752.
Kikuchi L, Chagas AL, Alencar RSSM, Tani C, Diniz MA, D’Albuquerque LAC, Carrilho FJ. Adherence to BCLC recommendations for the treatment of hepatocellular carcinoma: impact on survival according to stage. Clinics (Sao Paulo). 2017;72(8):454–60. https://doi.org/10.6061/clinics/2017(08)01.PMID:28954003;PMCID:PMC5577619.
Pillay B, Wootten AC, Crowe H, Corcoran N, Tran B, Bowden P, Crowe J, Costello AJ. The impact of multidisciplinary team meetings on patient assessment, management and outcomes in oncology settings: a systematic review of the literature. Cancer Treat Rev. 2016;42:56–72. https://doi.org/10.1016/j.ctrv.2015.11.007. Epub 2015 Nov 24 PMID: 26643552.
Croke JM, El-Sayed S. Multidisciplinary management of cancer patients: chasing a shadow or real value? An overview of the literature. Curr Oncol. 2012;19(4):e232–8. https://doi.org/10.3747/co.19.944.PMID:22876151;PMCID:PMC3410834.
Bauer K, Schroeder M, Porzsolt F, Henne-Bruns D. Comparison of international guidelines on the accompanying therapy for advanced gastric cancer: reasons for the differences. J Gastric Cancer. 2015;15(1):10–8. https://doi.org/10.5230/jgc.2015.15.1.10. Epub 2015 Mar 31. PMID: 25861518; PMCID: PMC4389092.
Freeman RK, Van Woerkom JM, Vyverberg A, Ascioti AJ. The effect of a multidisciplinary thoracic malignancy conference on the treatment of patients with esophageal cancer. Ann Thorac Surg. 2011;92(4):1239–42; discussion 1243. https://doi.org/10.1016/j.athoracsur.2011.05.057. Epub 2011 Aug 25. PMID: 21867990.
Bouvier AM, Créhange G, Azélie C, Cheynel N, Jouve JL, Bedenne L, Faivre J, Lepage C, Maingon P. Adjuvant treatments for gastric cancer: from practice guidelines to clinical practice. Dig Liver Dis. 2014;46(1):72–5. https://doi.org/10.1016/j.dld.2013.07.003. Epub 2013 Aug 23 PMID: 23978456.
Schmidt HM, Roberts JM, Bodnar AM, Kunz S, Kirtland SH, Koehler RP, Hubka M, Low DE. Thoracic multidisciplinary tumor board routinely impacts therapeutic plans in patients with lung and esophageal cancer: a prospective cohort study. Ann Thorac Surg. 2015;99(5):1719–24. https://doi.org/10.1016/j.athoracsur.2014.11.019. Epub 2015 Feb 10 PMID: 25678503.
Chen Y, Xiang J, Liu D, Xiao J, Xiong F, Wei K, Liu A, Chen S, Zhu Y, Meng X, Peng J. Multidisciplinary team consultation for resectable gastric cancer: a propensity score matching analysis. J Cancer. 2021;12(7):1907–14. https://doi.org/10.7150/jca.53365. PMID: 33753988; PMCID: PMC7974536.
English R, Metcalfe C, Day J, Rayter Z, Blazeby JM, breast cancer multi-disciplinary team. A prospective analysis of implementation of multi-disciplinary team decisions in breast cancer. Breast J. 2012;18(5):459–63. https://doi.org/10.1111/j.1524-4741.2012.01270.x. Epub 2012 Jul 10. PMID: 22776015.
Rajan S, Foreman J, Wallis MG, Caldas C, Britton P. Multidisciplinary decisions in breast cancer: does the patient receive what the team has recommended? Br J Cancer. 2013;108(12):2442–7. https://doi.org/10.1038/bjc.2013.267. Epub 2013 Jun 4. PMID: 23736032; PMCID: PMC3694248.
Ameratunga M, Miller D, Ng W, Wada M, Gonzalvo A, Cher L, Gan HK. A single-institution prospective evaluation of a neuro-oncology multidisciplinary team meeting. J Clin Neurosci. 2018;56:127–30. https://doi.org/10.1016/j.jocn.2018.06.032. Epub 2018 Jun 29 PMID: 30318071.
Chang YL, Lee SC, Liao CT, Wang CH, Lin YF, Chen SC. Factors impacting on discordance with treatment plan in head and neck cancer patients: a retrospective, population-based cohort study. Support Care Cancer. 2020;28(2):951–8. https://doi.org/10.1007/s00520-019-04904-z. Epub 2019 Jun 8 PMID: 31177393.
BrintzenhofeSzoc K, Krok-Schoen JL, Canin B, Parker I, MacKenzie AR, Koll T, Vankina R, Hsu CD, Jang B, Pan K, Lund JL, Starbuck E, Shahrokni A. The underreporting of phase III chemo-therapeutic clinical trial data of older patients with cancer: a systematic review. J Geriatr Oncol. 2020;11(3):369–379. https://doi.org/10.1016/j.jgo.2019.12.007. Epub 2020 Jan 10. PMID: 31932259; PMCID: PMC7412117.
Mohile SG, Mohamed MR, Xu H, Culakova E, Loh KP, Magnuson A, Flannery MA, Obrecht S, Gilmore N, Ramsdale E, Dunne RF, Wildes T, Plumb S, Patil A, Wells M, Lowenstein L, Janelsins M, Mustian K, Hopkins JO, Berenberg J, Anthony N, Dale W. Evaluation of geriatric assessment and management on the toxic effects of cancer treatment (GAP70+): a cluster-randomised study. Lancet. 2021;398(10314):1894–1904. https://doi.org/10.1016/S0140-6736(21)01789-X. Epub 2021 Nov 3. PMID: 34741815; PMCID: PMC8647163.
Parsons M, Lloyd S, Johnson S, et al. Refusal of local therapy in esophageal cancer and impact on overall survival. Ann Surg Oncol. 2021;28(2):663–75. https://doi.org/10.1245/s10434-020-08761-7.
Chew KS, Tan TW, Ooi YT. Influence of Chinese cultural health beliefs among Malaysian Chinese in a suburban population: a survey. Singapore Med J. 2011;52(4):252–6 (PMID: 21552785).
Chen HC, Allan H, Lu ZY. The social construction of cancer chemotherapy toxicity: the case of Taiwan. Cancer Nurs. 2013;36(4):E61–7. https://doi.org/10.1097/NCC.0b013e31826a7235. PMID: 23047801.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Joel Jia Yi Soon and Yue Zhao. The first draft of the manuscript was written by Joel Jia Yi Soon and all authors commented on previous versions of the manuscript. Nicholas Brian Shannon performed further data analysis and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This is an observational study. The SingHealth Centralised Institutional Review Board has confirmed that no ethical approval is required.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Soon, J.J.Y., Zhao, Y., Shannon, N.B. et al. Adherence to Multidisciplinary Tumor Board Recommendations in Patients With Curable Esophageal and Gastric Cancers. J Gastrointest Canc 54, 614–622 (2023). https://doi.org/10.1007/s12029-022-00847-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-022-00847-7