Abstract
Purpose
Aspirin reduces the incidence of various gastrointestinal (GI) malignancies. This meta-analysis assessed the efficacy and safety of regular aspirin use on the incidence of hepatocellular carcinoma (HCC) in patients with chronic liver disease.
Methods
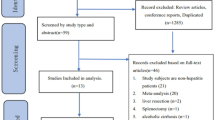
Electronic reference databases were searched for studies in patients with chronic liver disease exposed to aspirin. The primary outcome was the incidence of HCC in regular aspirin users compared to non-users. The secondary outcome was the incidence of major GI bleeding events in both groups. The propensity score (PS) and non-PS-adjusted pooled hazard ratio (HR) were calculated using random-effects models.
Results
Six observational studies with 71,211 subjects were included. The median duration of follow-up ranged from 2.7 to 7.9 years. Four studies included patients with viral hepatitis; five studies used aspirin 100 mg/day. All six studies reported the non-PS-matched HR, and there was a 54% reduction in the incidence of HCC among regular aspirin users [HR (95% CI): 0.46(0.31–0.67), p < 0.001]. Four studies reported on the PS-matched HR; this showed a 46% reduced incidence of HCC in those using aspirin [HR (95% CI): 0.54(0.38–0.79), p < 0.001]. Subgroup analysis on studies restricted to viral hepatitis (n = 4) showed a 28% reduction in HCC incidence in aspirin users [HR (95% CI): 0.72(0.64–0.80), p < 0.001]. Four studies reported the incidence of major GI bleeds, there was no significant difference between the two groups [HR (95% CI: 1.00(0.69–1.45), p = 0.90]. All outcome analysis, except the subgroup analysis, had significant inter-study heterogeneity.
Conclusion
Regular aspirin use in chronic liver disease is associated with reduced incidence of HCC without increasing the risk of major GI bleeding.



Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132:2557–76. https://doi.org/10.1053/j.gastro.2007.04.061.
Singal AG, Lampertico P, Nahon P. Epidemiology and surveillance for hepatocellular carcinoma: New trends. J Hepatol. 2020;72:250–61. https://doi.org/10.1016/j.jhep.2019.08.025.
Petrick JL, McGlynn KA. The changing epidemiology of primary liver cancer. Curr Epidemiol Rep. 2019;6:104–11. https://doi.org/10.1007/s40471-019-00188-3.
Flossmann E, Rothwell PM, British Doctors Aspirin Trial and the UK-TIA Aspirin Trial. Effect of aspirin on long-term risk of colorectal cancer: consistent evidence from randomised and observational studies. Lancet. 2007;369:1603–13. https://doi.org/10.1016/S0140-6736(07)60747-8
Bosetti C, Santucci C, Gallus S, Martinetti M, La Vecchia C. Aspirin and the risk of colorectal and other digestive tract cancers: an updated meta-analysis through 2019. Ann Oncol. 2020;31:558–68. https://doi.org/10.1016/j.annonc.2020.02.012.
Yoshida S, Ikenaga N, Liu SB, Peng Z-W, Chung J, Sverdlov DY, et al. Extrahepatic platelet-derived growth factor-β, delivered by platelets, promotes activation of hepatic stellate cells and biliary fibrosis in mice. Gastroenterology. 2014;147:1378–92. https://doi.org/10.1053/j.gastro.2014.08.038.
Malehmir M, Pfister D, Gallage S, Szydlowska M, Inverso D, Kotsiliti E, et al. Platelet GPIbα is a mediator and potential interventional target for NASH and subsequent liver cancer. Nat Med. 2019;25:641–55. https://doi.org/10.1038/s41591-019-0379-5.
Lee T-Y, Hsu Y-C, Tseng H-C, Lin J-T, Wu M-S, Wu C-Y. Association of daily aspirin therapy with hepatocellular carcinoma risk in patients with chronic hepatitis C virus infection. Clin Gastroenterol Hepatol. 2020;18:2784-2792.e7. https://doi.org/10.1016/j.cgh.2020.04.036.
Lee T-Y, Hsu Y-C, Tseng H-C, Yu S-H, Lin J-T, Wu M-S, et al. Association of daily aspirin therapy with risk of hepatocellular carcinoma in patients with chronic hepatitis B. JAMA Intern Med. 2019;179:633–40. https://doi.org/10.1001/jamainternmed.2018.8342.
Lee M, Chung GE, Lee J-H, Oh S, Nam JY, Chang Y, et al. Antiplatelet therapy and the risk of hepatocellular carcinoma in chronic hepatitis B patients on antiviral treatment. Hepatology. 2017;66:1556–69. https://doi.org/10.1002/hep.29318.
Simon TG, Duberg A-S, Aleman S, Chung RT, Chan AT, Ludvigsson JF. Association of aspirin with hepatocellular carcinoma and liver-related mortality. N Engl J Med. 2020;382:1018–28. https://doi.org/10.1056/NEJMoa1912035.
Shin S, Lee SH, Lee M, Kim JH, Lee W, Lee HW, et al. Aspirin and the risk of hepatocellular carcinoma development in patients with alcoholic cirrhosis. Medicine (Baltimore). 2020;99:e19008. https://doi.org/10.1097/MD.0000000000019008.
Booth A, Clarke M, Dooley G, Ghersi D, Moher D, Petticrew M, et al. The nuts and bolts of PROSPERO: an international prospective register of systematic reviews. Syst Rev. 2012;1:2. https://doi.org/10.1186/2046-4053-1-2.
Brooke BS, Schwartz TA, Pawlik TM. MOOSE reporting guidelines for meta-analyses of observational studies. JAMA Surg. 2021;156:787–8. https://doi.org/10.1001/jamasurg.2021.0522.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000.
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2013. http://www.R-project.org/.
Du Z-Q, Zhao J-Z, Dong J, Bi J-B, Ren Y-F, Zhang J, et al. Effect of low-dose aspirin administration on long-term survival of cirrhotic patients after splenectomy: A retrospective single-center study. World J Gastroenterol. 2019;25:3798–807. https://doi.org/10.3748/wjg.v25.i28.3798.
Pang Q, Jin H, Qu K, Man Z, Wang Y, Yang S, et al. The effects of nonsteroidal anti-inflammatory drugs in the incident and recurrent risk of hepatocellular carcinoma: a meta-analysis. Onco Targets Ther. 2017;10:4645–56. https://doi.org/10.2147/OTT.S143154.
Qiao Y, Yang T, Gan Y, Li W, Wang C, Gong Y, et al. Associations between aspirin use and the risk of cancers: a meta-analysis of observational studies. BMC Cancer. 2018;18:288. https://doi.org/10.1186/s12885-018-4156-5.
Wang S, Yu Y, Ryan PM, Dang M, Clark C, Kontogiannis V, et al. Association of aspirin therapy with risk of hepatocellular carcinoma: A systematic review and dose-response analysis of cohort studies with 2.5 million participants. Pharmacol Res. 2020;151:104585. https://doi.org/10.1016/j.phrs.2019.104585
Simon TG, Ma Y, Ludvigsson JF, Chong DQ, Giovannucci EL, Fuchs CS, et al. Association between aspirin use and risk of hepatocellular carcinoma. JAMA Oncol. 2018;4:1683–90. https://doi.org/10.1001/jamaoncol.2018.4154.
Hwang IC, Chang J, Kim K, Park SM. Aspirin use and risk of hepatocellular carcinoma in a national cohort study of korean adults. Sci Rep. 2018;8:4968. https://doi.org/10.1038/s41598-018-23343-0.
Petrick JL, Sahasrabuddhe VV, Chan AT, Alavanja MC, Beane-Freeman LE, Buring JE, et al. NSAID use and risk of hepatocellular carcinoma and intrahepatic cholangiocarcinoma: the liver cancer pooling project. Cancer Prev Res (Phila Pa). 2015;8:1156–62. https://doi.org/10.1158/1940-6207.CAPR-15-0126.
Tsoi KK, Ho JM, Chan FC, Sung JJ. Long-term use of low-dose aspirin for cancer prevention: A 10-year population cohort study in Hong Kong. Int J Cancer. 2019;145:267–73. https://doi.org/10.1002/ijc.32083.
Tanwar S, Rhodes F, Srivastava A, Trembling PM, Rosenberg WM. Inflammation and fibrosis in chronic liver diseases including non-alcoholic fatty liver disease and hepatitis C. World J Gastroenterol. 2020;26:109–33. https://doi.org/10.3748/wjg.v26.i2.109.
Ogunwobi OO, Liu C. Hepatocyte growth factor upregulation promotes carcinogenesis and epithelial-mesenchymal transition in hepatocellular carcinoma via Akt and COX-2 pathways. Clin Exp Metastasis. 2011;28:721–31. https://doi.org/10.1007/s10585-011-9404-x.
Koga H, Sakisaka S, Ohishi M, Kawaguchi T, Taniguchi E, Sasatomi K, et al. Expression of cyclooxygenase-2 in human hepatocellular carcinoma: relevance to tumor dedifferentiation. Hepatology. 1999;29:688–96. https://doi.org/10.1002/hep.510290355.
He J, Gerstenlauer M, Chan LK, Leithäuser F, Yeh MM, Wirth T, et al. Block of NF-kB signaling accelerates MYC-driven hepatocellular carcinogenesis and modifies the tumor phenotype towards combined hepatocellular cholangiocarcinoma. Cancer Lett. 2019;458:113–22. https://doi.org/10.1016/j.canlet.2019.05.023.
Arsura M, Cavin LG. Nuclear factor-kappaB and liver carcinogenesis. Cancer Lett. 2005;229:157–69. https://doi.org/10.1016/j.canlet.2005.07.008.
Wang SS, Chen YH, Chen N, Wang LJ, Chen DX, Weng HL, et al. Hydrogen sulfide promotes autophagy of hepatocellular carcinoma cells through the PI3K/Akt/mTOR signaling pathway. Cell Death Dis. 2017;8:e2688. https://doi.org/10.1038/cddis.2017.18.
Bhat M, Sonenberg N, Gores GJ. The mTOR pathway in hepatic malignancies. Hepatology. 2013;58:810–8. https://doi.org/10.1002/hep.26323.
Huang Z, Fang W, Liu W, Wang L, Liu B, Liu S, et al. Aspirin induces Beclin-1-dependent autophagy of human hepatocellular carcinoma cell. Eur J Pharmacol. 2018;823:58–64. https://doi.org/10.1016/j.ejphar.2018.01.031.
Mandrekar P, Szabo G. Signalling pathways in alcohol-induced liver inflammation. J Hepatol. 2009;50:1258–66. https://doi.org/10.1016/j.jhep.2009.03.007.
Witters P, Freson K, Verslype C, Peerlinck K, Hoylaerts M, Nevens F, et al. Review article: blood platelet number and function in chronic liver disease and cirrhosis. Aliment Pharmacol Ther. 2008;27:1017–29. https://doi.org/10.1111/j.1365-2036.2008.03674.x.
Muciño-Bermejo J, Carrillo-Esper R, Uribe M, Méndez-Sánchez N. Coagulation abnormalities in the cirrhotic patient. Ann Hepatol. 2013;12:713–24. https://doi.org/10.1016/S1665-2681(19)31312-2.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Systematic review and data collection were performed by Jin Lin Tan and Sandeep Sidhu-Brar with supervision by Mohamed Asif Chinnaratha. The first draft of the manuscript was written by Jin Lin Tan, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This is a systematic review and meta-analysis of observational study. Ethical approval is not required.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tan, J.L., Sidhu-Brar, S., Woodman, R. et al. Regular Aspirin Use Is Associated with a Reduced Risk of Hepatocellular Carcinoma (HCC) in Chronic Liver Disease: a Systematic Review and Meta-analysis. J Gastrointest Canc 54, 325–331 (2023). https://doi.org/10.1007/s12029-022-00842-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-022-00842-y