Abstract
Background
The aim of this study is to analyze the role of neutrophil–lymphocyte ratio (NLR) and its variation pre- and postoperatively (delta NLR) in the overall survival after pancreatectomy for pancreatic ductal adenocarcinoma (PDAC) at a single center and to identify factors associated with overall survival.
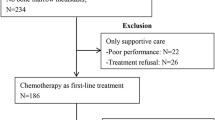
Methods
A retrospective study of consecutive patients undergoing pancreatectomy due to PDAC or undifferentiated carcinoma from January 2010 to January 2020 was performed. Association between the evaluated factors and overall survival was analyzed using a log-rank test and Cox proportional hazard regression model.
Results
Overall, 242 patients underwent pancreatectomy for PDAC or undifferentiated carcinoma. OS was 22.8 months (95% confidence interval (CI): 19.5–29), and survival rates at 1, 3, and 5 years were 72%, 32.5%, and 20.8%, respectively. NLR and delta NLR were not significantly associated with survival (hazard ratio (HR) = 1.14, 95%CI: 0.77–1.68, p = 0.5). Lymph node ratio was significantly associated (HR = 1.66, 95%CI: 1.21–2.26, p = 0.001) in the bivariate analysis. In multivariable analysis, the only factors that were significantly associated with survival were perineural invasion (HR = 1.94, 95%CI: 1.21–3.14, p = 0.006), surgical margin (HR = 1.83, 95%CI: 1.10–3.02, p = 0.019), tumor size (HR = 1.01, 95%CI: 1.003–1.027, p = 0.16), postoperative CA 19–9 level (HR = 1.001, p < 0.001), and completion of adjuvant treatment (HR = 0.53, 95%CI: 0.35–0.8, p = 0.002).
Conclusion
Neutrophil–lymphocyte ratio and delta NLR were not associated with the overall survival in this cohort. Risk factors such as perineural invasion, surgical margins, CA19-9 level, and tumor size showed worse survival in this study, whereas completing adjuvant treatment was a protective factor.


Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. PMID: 30207593.
Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the united states. Cancer Res. 2014;74(11):2913–21. PMID: 24840647.
Oettle H, Neuhaus P, Hochhaus A, Hartmann JT, Gellert K, Ridwelski K, et al. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: the CONKO-001 randomized trial. JAMA - J Am Med Assoc. 2013;310(14):1473–81. PMID: 24104372.
Neoptolemos JP, Kleeff J, Michl P, Costello E, Greenhalf W, Palmer DH. Therapeutic developments in pancreatic cancer: current and future perspectives. Nat Rev Gastroenterol Hepatol. 2018;15(6):333–48. PMID: 29717230.
Klaiber U, Hackert T, Neoptolemos JP. Adjuvant treatment for pancreatic cancer. Transl Gastroenterol Hepatol. 2019;4(April). PMID: 31143848.
Conroy T, Hammel P, Hebbar M, Ben Abdelghani M, Wei AC, Raoul J-L, et al. FOLFIRINOX or gemcitabine as adjuvant therapy for pancreatic cancer. N Engl J Med. 2018;379:2395–406. PMID: 30575490.
Strobel O, Lorenz P, Hinz U, Gaida M, Konig AK, Hank T, et al. Actual five-year survival after upfront resection for pancreatic ductal adenocarcinoma. Ann Surg. 2020. PMID: 32649469. https://doi.org/10.1097/SLA.0000000000004147.
Liebl F, Demir IE, Mayer K, Schuster T, D’Haese J, Becker K, et al. The impact of neural invasion severity in gastrointestinal malignancies: a clinicopathological study. Ann Surg. 2014;260(5):900–8. PMID: 25379860.
Luchini C, Veronese N, Nottegar A, Riva G, Pilati C, Mafficini A, et al. Perineural invasion is a strong prognostic moderator in ampulla of vater carcinoma: a meta-analysis. Pancreas. 2019;48(1):70–6. PMID: 30451797.
Gasparini G, Pellegatta M, Crippa S, Schiavo Lena M, Belfiori G, et al. Nerves and pancreatic cancer: new insights into a dangerous relationship. Cancers (Basel). 2019;11(7):1–24. PMID: 31248001.
Faulkner S, Jobling P, March B, Jiang CC, Hondermarck H. Tumor neurobiology and the war of nerves in cancer. Cancer Discov. 2019;9(6):702–10. PMID: 30944117.
Roxburgh CSD, McMillan DC. Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Futur Oncol. 2010;6(1):149–63. PMID: 20021215.
Luo G, Guo M, Liu Z, Xiao Z, Jin K, Long J, et al. Blood neutrophil–lymphocyte ratio predicts survival in patients with advanced pancreatic cancer treated with chemotherapy. Ann Surg Oncol. 2015;22(2):670–6. PMID: 25155401.
Zhou Y, Wei Q, Fan J, Cheng S, Ding W, Hua Z. Prognostic role of the neutrophil-to-lymphocyte ratio in pancreatic cancer: a meta-analysis containing 8252 patients. Clin Chim Acta. 2018;479(January):181–9. PMID: 29407690.
Malleo G, Maggino L, Capelli P, Gulino F, Segattini S, Scarpa A, et al. Reappraisal of nodal staging and study of lymph node station involvement in pancreaticoduodenectomy with the standard international study group of pancreatic surgery definition of lymphadenectomy for cancer. J Am Coll Surg. 2015;221(2):367-379.e4. PMID: 26081176.
You MS, Lee SH, Cho YH, Shin BS, Paik WH, Riu JK, et al. Lymph node ratio as valuable predictor in pancreatic cancer treated with R0 resection and adjuvant treatment. BMC Cancer. 2019;19(1):1–8. PMID: 31615457.
Merlo I, Fratantoni E, de Santibañes M, Ardiles V, Sanchez Clariá R, Pekolj J, de Santibañes E, Mazza O. Long-term survival after pancreatic cancer surgery. Medicina (B Aires). 2021;81(5):800–807. PMID: 34633955.
Cong L, Liu Q, Zhang R, Cui M, Zhang X, Gao X, et al. Tumor size classification of the 8th edition of TNM staging system is superior to that of the 7th edition in predicting the survival outcome of pancreatic cancer patients after radical resection and adjuvant chemotherapy. Sci Rep. 2018;8(1):10383. PMID: 29991730.
Aoyama T, Yamamoto N, Kamiya M, Murakawa M, Tamagawa H, Sawazaki S, et al. The lymph node ratio is an independent prognostic factor in pancreatic cancer patients who receive curative resection followed by adjuvant chemotherapy. Anticancer Res. 2018;38(8):4877–82. PMID: 30061263.
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017;161:584–91. PMID: 28040257.
Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96. PMID: 19638912.
Swords DS, Mulvihill SJ, Skarda DE, Finlayson S, Stoddard GJ, Ott MJ, et al. Hospital-level variation in utilization of surgery for clinical stage I-II pancreatic adenocarcinoma. Ann Surg. 2019;269(1):133–42. PMID: 28700442.
Chatterjee D, Katz MH, Rashid A, Wang H, Iuga AC, Varadhachary GR, et al. Perineural and intraneural invasion in posttherapy pancreaticoduodenectomy specimens predicts poor prognosis in patients with pancreatic ductal adenocarcinoma. Am J Surg Pathol. 2012;36(3):409–17. PMID: 22301497.
Yi SQ, Miwa K, Ohta T, Kayahara M, Kitagawa H, Tanaka A, et al. Innervation of the pancreas from the perspective of perineural invasion of pancreatic cancer. Pancreas. 2003;27(3):225–9. PMID: 14508126.
Renz BW, Takahashi R, Tanaka T, Macchini M, Hayakawa Y, Dantes Z, et al. β2 adrenergic-neurotrophin feedforward loop promotes pancreatic cancer. Cancer Cell. 2018;33(1):75-90.e7. PMID: 29249692.
Ceyhan GO, Bergmann F, Kadihasanoglu M, Altintas B, Demir IE, Hinz U, et al. Pancreatic neuropathy and neuropathic pain-a comprehensive pathomorphological study of 546 cases. Gastroenterology. 2009;136(1):177-186.e1. PMID: 18992743.
Crippa S, Pergolini I, Javed AA, KC. Honselmann, M. J. Weiss, F. Di Salvo, et al., “Implications of perineural invasion on disease recurrence and survival after pancreatectomy for pancreatic head ductal adenocarcinoma,” Ann. Surg., vol. Publish Ah, Oct. 2020. PMID: 33086324
Pawlik TM, Gleisner AL, Cameron JL, Winter JM, Assumpcao L, Lillemoe KD, et al. Prognostic relevance of lymph node ratio following pancreaticoduodenectomy for pancreatic cancer. Surgery. 2007;141(5):610–8. PMID: 17462460.
Choi N, Kim JH, Chie EK, Gim J, Kang HC. A meta-analysis of the impact of neutrophil-to-lymphocyte ratio on treatment outcomes after radiotherapy for solid tumors. Med (United States). 2019;98(18):1–8. PMID: 31045780.
McLellan P, Henriques J, Ksontini F, Doat S, Hammel P, Desrame J, et al. Prognostic value of the early change in neutrophil-to-lymphocyte ratio in metastatic pancreatic adenocarcinoma. Clin Res Hepatol Gastroenterol. 2021;45(3):101541. PMID: 33055007.
Ferrone CR, Marchegiani G, Hong TS, Ryan DP, Deshpande V, McDonnell EI, et al. Radiological and surgical implications of neoadjuvant treatment with FOLFIRINOX for locally advanced and borderline resectable pancreatic cancer. Ann Surg. 2015;261(1):12–7. PMID: 25599322.
Barnes CA, Chavez MI, Tsai S, Aldakkak M, George B, Ritch PS, et al. Survival of patients with borderline resectable pancreatic cancer who received neoadjuvant therapy and surgery. Surg (United States). 2019;166(3):277–85. PMID: 31272811.
Versteijne E, Suker M, Groothuis K, Akkermans-Vogelaar JM, Besselink MG, Bonsing BA, et al. Preoperative chemoradiotherapy versus immediate surgery for resectable and borderline resectable pancreatic cancer: results of the Dutch randomized phase III PREOPANC trial. J Clin Oncol. 2020;38(16):1763–73. PMID: 32105518.
Van Eijck CHJ et al. Preoperative chemoradiotherapy to improve overall survival in pancreatic cancer: long-term results of the multicenter randomized phase III PREOPANC trial. J Clin Oncol. 2021;39(15_suppl):4016–4016. https://doi.org/10.1200/JCO.2021.39.15_suppl.4016.
Author information
Authors and Affiliations
Contributions
(I) Conception and design: Martín de Santibañes, Ignacio G. Merlo. (II) Administrative support: Juan Pekolj. (III) Provision of study materials or patients: Oscar Mazza, Rodrigo Sanchez Claria, Juan Pekolj, Martín de Santibañes, Eduardo de Santibañes. (IV) Collection and assembly of data: Ignacio G. Merlo, Eugenia Fratantoni. (V) Data analysis and interpretation: Ignacio G. Merlo, Victoria Ardiles. (VI) Manuscript writing: All authors. (VII) Final approval of manuscript: All authors.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Merlo, I., Ardiles, V., Sanchez-Clariá, R. et al. Prognostic Factors in Resected Pancreatic Ductal Adenocarcinoma: Is Neutrophil-Lymphocyte Ratio a Useful Marker?. J Gastrointest Canc 54, 580–588 (2023). https://doi.org/10.1007/s12029-022-00839-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-022-00839-7