Abstract
Purpose
To clarify the factors affecting the length of hospitalization after laparoscopic gastrectomy based on the physical function, body composition, and postoperative course of the patients.
Methods
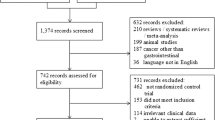
Of the patients with gastric cancer who underwent laparoscopic resection at the Ageo Central General Hospital, Japan, during 2018–2019, 51 underwent physical therapy. Data regarding the objective variables, such as length of postoperative hospital stay, and baseline attributes, such as age, body weight, body mass index (BMI), and corrected limb muscle mass, postoperative course (operation time, the estimated blood loss, the day before walking independently), preoperative physical function (grip strength, 6-min walking distance), and preoperative respiratory function (vital capacity [VC]%, one-second rate) were collected retrospectively from the medical records and analyzed using multiple regression plots.
Results
The most suitable hospital day model after surgery is one that incorporates the total postoperative course, respiratory function, physical function (R2 = 0.45, p < 0001), and operation time (β = 0.12, p < 0.06). The information of the day before independent walking (β = 0.68, p < 0.001) and % VC (β = −0.19, p < 0.04) was extracted as factors.
Conclusion
We concluded that the operation time, walking independence days, and % VC influence the postoperative length of hospital days.

Similar content being viewed by others
References
Rahman R, Asombang AW, Ibdah JA. Characteristics of gastric cancer in Asia. World J Gastroenterol. 2014;20:4483–90.
Foundation for Promotion of Cancer Research. Cancer statistics in Japan 2018. FPCR. 2019. https://www.fpcr.or.jp/pamphlet.html. Accessed 20 June 2019.
Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017;20:1–19.
Kitano S, Shiraishi N, Uyama I, Sugihara K, Tanigawa N. A multicenter study on oncologic outcome of laparoscopic gastrectomy for early cancer in Japan. Ann Surg. 2007;245:68–72.
Miki Y, Makuuchi R, Tokunaga M, Tanizawa Y, Bando E, Kawamura T, Terashima M. Risk factors for postoperative pneumonia after gastrectomy for gastric cancer. Surg Today. 2016;46:552–6.
Ito K, Suka Y, Nagai M, Kawasaki K, Yamamoto M, Koike D, Nomura Y, Tanaka N, Kawaguchi Y. Lower risk of postoperative delirium using laparoscopic approach for major abdominal surgery. Surg Endosc. 2019;33:2121–7.
Hara T, Sano M, Shinomiya M, Nonaka Y, Ichimura S, Nakano T, Matsuzawa M, Sakurai A, Kusano S, Kubo A, Kubota K. Relationships among gender, physical function and surgical procedure in perioperative gastrointestinal cancer patients. Rigakuryoho Kagaku. 2012;27:705–9.
Hayashi K, Yokoyama Y, Nakajima H, Nagino M, Inoue T, Nagaya M, Hattori K, Kadono I, Ito S, Nishida Y. Preoperative 6-minute walk distance accurately predicts postoperative complications after operations for hepato-pancreato-biliary cancer. Surgery. 2017;161:525–32.
Inoue T, Ito S, Kanda M, Niwa Y, Nagaya M, Nishida Y, Hasegawa Y, Koike M, Kodera Y. Preoperative six-minute walk distance as a predictor of postoperative complication in patients with esophageal cancer. Dis Esophagus. 2020;33:doz050.
Grigorakos L, Sotiriou E, Koulendi D, Michail A, Alevizou S, Evagelopoulou P, Karatzas S, Ligidakis N. Preoperative pulmonary evaluation (PPE) as a prognostic factor in patients undergoing upper abdominal surgery. Hepatogastroenterology. 2008;55(85):1229–32.
ESMO. Stomach cancer: a guide for patients - Information based on ESMO Clinical Practice Guidelines - v.2012.1. ESMO. 2019. https://www.esmo.org/content/download/19445/330564/file/stomach. Accessed 20 June 2019.
Best LM, Mughal M, Gurusamy KS. Laparoscopic versus open gastrectomy for gastric cancer. Cochrane Database Syst Rev. 2016;3:CD011389.
Liang Y, Liu H, Nurse L, Zhu Y, Zhao M, Hu Y, Yu J, Li C, Liu K, Li G. Enhanced recovery after surgery for laparoscopic gastrectomy in gastric cancer: a prospective study. Medicine (Baltimore). 2021;100:e2467.
Kang SH, Lee Y, Min SH, Park YS, Ahn SH, Park DJ, Kim HH. Multimodal Enhanced Recovery After Surgery (ERAS) Program is the optimal perioperative care in patients undergoing totally laparoscopic distal gastrectomy for gastric cancer: a prospective, randomized, clinical trial. Ann Surg Oncol. 2018;25:3231–8.
Olin K, Eriksdotter-Jönhagen M, Jansson A, Herrington MK, Kristiansson M, Permert J. Postoperative delirium in elderly patients after major abdominal surgery. Br J Surg. 2005;92:1559–64.
Bundgaard-Nielsen M, Jørgensen CC, Jørgensen TB, Ruhnau B, Secher NH, Kehlet H. Orthostatic intolerance and the cardiovascular response to early postoperative mobilization. Br J Anaesth. 2009;102:756–62.
Kim KM, An JY, Kim HI, Cheong JH, Hyung WJ, Noh SH. Major early complications following open, laparoscopic and robotic gastrectomy. Br J Surg. 2012;99:1681–7.
Ali J, Weisel RD, Layug AB, Kripke BJ, Hechtman HB. Consequences of postoperative alterations in respiratory mechanics. Am J Surg. 1974;128:376–82.
Ford GT, Whitelaw WA, Rosenal TW, Cruse PJ, Guenter CA. Diaphragm function after upper abdominal surgery in humans. Am Rev Respir Dis. 1983;127:431–6.
Simonneau G, Vivien A, Sartene R, Kunstlinger F, Samii K, Noviant Y, Duroux P. Diaphragm dysfunction induced by upper abdominal surgery. Role of postoperative pain. Am Rev Respir Dis. 1983;128:899–903.
Dureuil B, Cantineau JP, Desmonts JM. Effects of upper or lower abdominal surgery on diaphragmatic function. Br J Anaesth. 1987;59:1230–5.
Steffen TM, Hacker TA, Mollinger L. Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys Ther. 2002;82:128–37.
Soares SM, Nucci LB, da Silva MM, Campacci TC. Pulmonary function and physical performance outcomes with preoperative physical therapy in upper abdominal surgery: a randomized controlled trial. Clin Rehabil. 2013;27:616–27.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Chisa Hirukawa, Tatsuro Fukuda, Yuka Hidaka, Yukiho Makita, Kyosuke Fukuda, and Yuta Sakamoto. The first draft of the manuscript was written by Takashi Amari and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This study was approved by the institutional ethics committee (approval number: 603).
Consent to Participate and Publication
Written informed consent for the use of the data and publication of the article was obtained from the patients.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Amari, T., Hirukawa, C., Fukuda, T. et al. Factors Affecting the Length of Hospital Days After Laparoscopic Gastrectomy for Elderly Patients with Gastric Cancer. J Gastrointest Canc 53, 472–479 (2022). https://doi.org/10.1007/s12029-021-00633-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-021-00633-x