Abstract
There are many studies on the biomarkers for the prognosis in the treatment of metastatic colorectal cancer. Neutrophil-lymphocyte radio (NLR) and platelet-lymphocyte radio (PLR) are of interest with studies revealing the relationship between inflammatory biomarkers and cancer. Our study is a retrospective file study and the contribution of NLR and PLR to progression-free survival (PFS) and overall survival (OS) before first-line chemotherapy was investigated regardless of treatment. The cutoff values of NLR and PLR were determined using ROC curve analysis. NLR and PLR were divided into two groups according to the cut-off points. OS and PFS associated with NLR and PLR were performed by the Kaplan-Meier method. In our study, we could not demonstrate the prognostic potential of pre-treatment NLR and PLR in patients with mCRC treated with first-line chemotherapy. Our study showed that the use of these biomarkers in mCRC is limited.
Introduction
There are many studies on the biomarkers for the prognosis in the treatment of metastatic colorectal cancer. Neutrophil-lymphocyte radio (NLR) and platelet-lymphocyte radio (PLR) are of interest with studies revealing the relationship between inflammatory biomarkers and cancer.
Material and Method
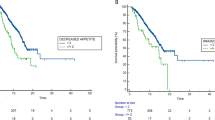
Our study is a retrospective file study and the contribution of NLR and PLR to progression-free survival (PFS) and overall survival (OS) before first-line chemotherapy was investigated regardless of treatment. The cutoff values of NLR and PLR were determined using ROC curve analysis. NLR and PLR were divided into two groups according to the cut-off points. OS and PFS associated with NLR and PLR were performed by the Kaplan-Meier method.
Result
In our study, we could not demonstrate the prognostic potential of pre-treatment NLR and PLR in patients with mCRC treated with first-linechemotherapy.
Conclusion
Our study showed that the use of these biomarkers in mCRC is limited.


Similar content being viewed by others
References
Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–386. https://doi.org/10.1002/ijc.29210
Van Cutsem E, Cervantes A, Nordlinger B, et al. Metastatic colorectal cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2014;25 Suppl 3:iii1–9. https://doi.org/10.1093/annonc/mdu260
Hamers PAH, Elferink MAG, Stellato RK, et al. Informing metastatic colorectal cancer patients by quantifying multiple scenarios for survival time based on real-life data. Int J Cancer. 2020;15;148(2):296–306. https://doi.org/10.1002/ijc.33200
Stein A, Bokemeyer C. How to select the optimal treatment for first line metastatic colorectal cancer. World J Gastroenterol. 2014;20:899–907. https://doi.org/10.3748/wjg.v20.i4.899.
De Divitiis C, Nasti G, Montano M, et al. Prognostic and predictive response factors in colorectal cancer patients: between hope and reality. World J Gastroenterol. 2014;20:15049–59. https://doi.org/10.3748/wjg.v20.i41.15049
Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–7. https://doi.org/10.1038/nature01322.
Lu H, Ou yang W, Huang C. Inflammation, a key event in cancer development. Mol Cancer Res. 2006;4:221–33. https://doi.org/10.1158/1541-7786.MCR-05-0261
Tartour E, Zitvogel L. Lung cancer: potential targets for immunotherapy. Lancet Respir Med. 2013;1:551–63. https://doi.org/10.1016/S2213-2600(13)70159-0.
Aerts JG, Hegmans JP. Tumor-specific cytotoxic T cells are crucial for efficacy of immunomodulatory antibodies in patients with lung cancer. Cancer Res. 2013;73(8):2381 2388. https://doi.org/10.1158/0008-5472.CAN-12-3932
Shang K, Bai YP, Wang C, et al. Crucial involvement of tumor-associated neutrophils in the regulation of chronic colitis-associated carcinogenesis in mice.PLoS One. 2012;7(12):e51848. https://doi.org/10.1371/journal.pone.0051848
Sagiv JY, Michaeli J, Assi S, et al. Phenotypic diversity and plasticity in circulating neutrophil subpopulations in cancer. Cell Rep. 2015;10(4):562–73. https://doi.org/10.1016/j.celrep.2014.12.039
Sionov RV, Fridlender ZG, Granot Z. The multifaceted roles neutrophils play in the tumor microenvironment. Cancer Microenviron. 2015;8(3):125–58. https://doi.org/10.1007/s12307-014-0147-5.
Pilatova K, Zdrazilova-Dubska L, Klement GL The role of platelets in tumour growth. Klin Onkol. 2012;25(Suppl 2):2S50–7.
Malietzis G, Giacometti M, Kennedy RH, et al. The emerging role of neutrophil to lymphocyte ratio in determining colorectal cancer treatment outcomes: a systematic review and meta-analysis. Ann Surg Oncol. 2014;21:3938–46. https://doi.org/10.1245/s10434-014-3815-2
Feng JF, Huang Y, Chen QX. The combination of platelet count and neutrophil lymphocyte ratio is a predictive factor in patients with esophageal squamous cell carcinoma. Transl Oncol. 2014;7:632–7. https://doi.org/10.1016/j.tranon.2014.07.009.
Galizia G, Lieto E, Zamboli A, et al. Neutrophil to lymphocyte ratio is a strong predictor of tumor recurrence in early colon cancers: a propensity score-matched analysis. Surgery. 2015;158:112–20. https://doi.org/10.1016/j.surg.2015.02.006
Shin JS, Suh KW, Oh SY. Preoperative neutrophil to lymphocyte ratio predicts survival in patients with T1–2N0 colorectal cancer. J Surg Oncol. 2015;112:654–7 https://doi.org/10.1002/jso.24061
Krauthamer M, Rouvinov K, Ariad S, et al. A study of inflammation-based predictors of tumor response to neoadjuvant chemoradiotherapy for locally advanced rectal cancer. Oncology. 2013;85:27–32. https://doi.org/10.1159/000348385
Kim IY, You SH, Kim YW. Neutrophil-lymphocyte ratio predicts pathologic tumor response and survival after preoperative chemoradiation for rectal cancer. BMC Surg. 2014;14:94. https://doi.org/10.1186/1471-2482-14-94.
Pichler M, Absenger G, Stotz M, et al. The elevated preoperative platelet to lymphocyte ratio predicts decreased time to recurrence in colon cancer patients. Am J Surg. 2014;208:210–4. https://doi.org/10.1016/j.amjsurg.2013.10.030.
Zhang Y, Jiang C, Li J, Sun J, Qu X. Prognostic significance of preoperative neutrophil/lymphocyte ratio and nplatelet/lymphocyte ratio in patients with gall bladder carcinoma. Clin Transl Oncol. 2015;17:810–8. https://doi.org/10.1097/MD.0000000000014550.
Bozkurt O, Karaca H, Berk V, et al. Predicting the role of the pretreatment neutrophil to lymphocyte ratio in the survival of early triple- negative breast cancer patients. JBUON. 2015;20:1432–9.
Roxburgh CSD, McMillan D. Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Future Oncol. 2010;6:149–63. https://doi.org/10.2217/fon.09.136.
Chua W, Charles KA, Baracos VE, Clarke SJ. Neutrophil/lymphocyte ratio predicts chemotherapy outcomes in patients with advanced colorectal cancer. Br J Cancer. 2011;104:1288–95. https://doi.org/10.1038/bjc.2011.100.
Dell’Aquila E, Cremolini C, et al. Prognostic and predictive role of neutrophil/lymphocytes ratio in metastatic colorectal cancer: a retrospective analysis of the tribe study by gono. Ann Oncol. 2018;29:924–30. https://doi.org/10.1093/annonc/mdy004.
Matsuda A, Yamada T, Matsuda S, et al. Prognostic role of the platelet-to-lymphocyte ratio for patients with metastatic colorectal cancer treated with aflibercept. In Vivo. 2020;34(5): 2667–2673. https://doi.org/10.21873/invivo.12086
Dogan E, Bozkurt O, Sakalar T, et al. Impact of neutrophil-lymphocyte and platelet-lymphocyte ratio on antiEGFR and bevacizumab efficacy in metastatic colorectal cancer. JBUON 2019;24(5): 1861–1869
Nogueira-Costa G, Fernandes I, Gameiro R, et al. Prognostic utility of neutrophil-to-lymphocyte ratio in patients with metastatic colorectal cancer treated using different modalities. Curr Oncol. 2020;27(5): 237–243. https://doi.org/10.3747/co.27.6573
Yang J, Guo X, Wang M, Ma X, Ye X, Lin P. Pre-treatment inflammatory indexes as predictors of survival and cetuximab efficacy in metastatic colorectal cancer patients with wild-type RAS. Sci Rep. 2017;7:17166. https://doi.org/10.1038/s41598-017-17130-6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bulut, G., Ozdemir, Z.N. Prognostic Significance of Neutrophil-Lymphocyte Ratio and Platelet-Lymphocyte Ratio in Metastatic Colorectal Cancer. J Gastrointest Canc 53, 1–6 (2022). https://doi.org/10.1007/s12029-021-00616-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-021-00616-y