Abstract
Background
NSQIP Risk Calculator was developed to allow surgeons to inform their patients about their individual risks for surgery. Its ability to predict complication rates and length of stay (LOS) has made it an appealing tool for both patients and surgeons. However, the NSQIP Risk Calculator has been criticized for its generality and lack of detail towards surgical subspecialties, including the hepatopancreaticobiliary (HPB) surgery. We wish to determine whether the NSQIP Risk Calculator is predictive of post-operative complications and LOS with respect to Whipple’s resections for our patient population. As well, we wish to identify strategies to optimize early surgical outcomes in patients with pancreatic cancer.
Methods
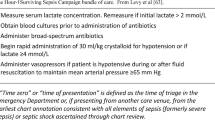
We conducted a retrospective review of patients who underwent elective Whipple’s procedure for benign or malignant pancreatic head lesions at Health Sciences North (Sudbury, Ontario), a tertiary care center, from February 2014 to August 2016. Comparisons of LOS and post-operative complications between NSQIP-predicted and actual ones were carried out. NSQIP-predicted complications rates were obtained using the NSQIP Risk Calculator through pre-defined preoperative risk factors. Clinical outcomes examined, at 30 days post-operation, included pneumonia, cardiac events, surgical site infection (SSI), urinary tract infection (UTI), venous thromboembolism (VTE), renal failure, readmission, and reoperation for procedural complications. As well, mortality, disposition to nursing or rehabilitation facilities, and LOS were assessed.
Results
A total of 40 patients underwent Whipple’s procedure at our center from February 2014 to August 2016. The average age was 68 (50–85), and there were 22 males and 18 females. The majority of patients had independent baseline functional status (39/40) with minimal pre-operative comorbidities. The overall post-operative morbidity was 47.5% (19/40). The rate of serious complication was 17.5% with four Clavien grade II, two grade III, and one grade V complications. One mortality occurred within 30 days after surgery. NSQIP Risk Calculator was predictive for the majority of post-surgical complication types, including pneumonia, SSI, VTE, reoperation, readmission, and disposition to rehabilitation or nursing home. Our center appears to have a higher rate of UTI than NSQIP predicted (O/E = 3.9), as well, the rate of cardiac complication (O/E = 3.1) also appears to be higher at our center. With respect to readmission rates (O/E = 0.6) and renal failure (O/E = 0), NSQIP provided overestimated rates. The average LOS was 11.9 ± 0.9 days, which was not significantly different from the average LOS of 11.5 ± 0.3 days predicted by NSQIP (p = 0.3). Overall, 80% of discharges occurred less than or within 3 days of that predicted by NSQIP.
Conclusion
NSQIP Risk Calculator is predictive of post-operative complications and LOS for patients who have undergone Whipple’s at our center. A more HPB-focused NSQIP calculator may accurately project post-operative complication in the pre-operative period. Nevertheless, the generic NSQIP has allowed us to examine our existing practice of post-operative care and has paved way to reduce cardiac and urinary complications in the future.

Similar content being viewed by others
References
Fernandez-del Castillo C, Morales-Oyarvide V, McGrath D, Wargo JA, Ferrone CR, Thayer SP, Lillemoe KD, Warshaw AL. Evolution of the Whipple procedure at the Massachusetts General Hospital. Surgery. 2012;152(3 Suppl 1):S56–63. doi:10.1016/j.surg.2012.05.022.
Are C, Dhir M, Ravipati L. History of pancreaticoduodenectomy: early misconceptions, initial milestones and the pioneers. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2011;13(6):377–84. doi:10.1111/j.1477-2574.2011.00305.x.
Bakkevold KE, Kambestad B. Morbidity and mortality after radical and palliative pancreatic cancer surgery. Risk factors influencing the short-term results. Ann Surg. 1993;217(4):356–68.
Dimick JB, Pronovost PJ, Cowan JA Jr, Lipsett PA, Stanley JC, Upchurch GR Jr. Variation in postoperative complication rates after high-risk surgery in the United States. Surgery. 2003;134(4):534–40. doi:10.1016/S0039. discussion 540-531
Gupta PK, Turaga KK, Miller WJ, Loggie BW, Foster JM. Determinants of outcomes in pancreatic surgery and use of hospital resources. J Surg Oncol. 2011;104(6):634–40. doi:10.1002/jso.21923.
Cohen ME, Liu Y, Ko CY, Hall BL. Improved surgical outcomes for ACS NSQIP hospitals over time: evaluation of hospital cohorts with up to 8 years of participation. Ann Surg. 2016;263(2):267–73. doi:10.1097/SLA.0000000000001192.
Cohen ME, Ko CY, Bilimoria KY, Zhou L, Huffman K, Wang X, Liu Y, Kraemer K, Meng X, Merkow R, Chow W, Matel B, Richards K, Hart AJ, Dimick JB, Hall BL. Optimizing ACS NSQIP modeling for evaluation of surgical quality and risk: patient risk adjustment, procedure mix adjustment, shrinkage adjustment, and surgical focus. J Am Coll Surg. 2013;217(2):336–346 e331. doi:10.1016/j.jamcollsurg.2013.02.027.
Bilimoria KY, Liu Y, Paruch JL, Zhou L, Kmiecik TE, Ko CY, Cohen ME. Development and evaluation of the universal ACS NSQIP surgical risk calculator: a decision aid and informed consent tool for patients and surgeons. J Am Coll Surg. 2013;217(5):833–842 e831-833. doi:10.1016/j.jamcollsurg.2013.07.385.
Hall BL, Hamilton BH, Richards K, Bilimoria KY, Cohen ME, Ko CY. Does surgical quality improve in the American College of Surgeons National Surgical Quality Improvement Program: an evaluation of all participating hospitals. Ann Surg. 2009;250(3):363–76. doi:10.1097/SLA.0b013e3181b4148f.
Khuri SF, Henderson WG, Daley J, Jonasson O, Jones RS, Campbell DA Jr, Fink AS, Mentzer RM Jr, Steeger JE, Principal Site Investigators of the Patient Safety in Surgery S. The patient safety in surgery study: background, study design, and patient populations. J Am Coll Surg. 2007;204(6):1089–102. doi:10.1016/j.jamcollsurg.2007.03.028.
Guillamondegui OD, Gunter OL, Hines L, Martin BJ, Gibson W, Clarke PC, Cecil WT, Cofer JB. Using the National Surgical Quality Improvement Program and the Tennessee Surgical Quality Collaborative to improve surgical outcomes. J Am Coll Surg. 2012;214(4):709–714; discussion 714-706. doi:10.1016/j.jamcollsurg.2011.12.012.
Ho CK, Kleeff J, Friess H, Buchler MW. Complications of pancreatic surgery. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2005;7(2):99–108. doi:10.1080/13651820510028936.
Crist DW, Sitzmann JV, Cameron JL. Improved hospital morbidity, mortality, and survival after the Whipple procedure. Ann Surg. 1987;206(3):358–65.
Andren-Sandberg A. Complications of pancreatic surgery. N Am J Med Sci. 2011;3(12):531–5. doi:10.4297/najms.2011.3531.
Greco M, Capretti G, Beretta L, Gemma M, Pecorelli N, Braga M. Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg. 2014;38(6):1531–41. doi:10.1007/s00268-013-2416-8.
Saint S, Greene MT, Krein SL, Rogers MA, Ratz D, Fowler KE, Edson BS, Watson SR, Meyer-Lucas B, Masuga M, Faulkner K, Gould CV, Battles J, Fakih MG. A program to prevent catheter-associated urinary tract infection in acute care. N Engl J Med. 2016;374(22):2111–9. doi:10.1056/NEJMoa1504906.
Fleisher LA, Fleischmann KE, Auerbach AD, Barnason SA, Beckman JA, Bozkurt B, Davila-Roman VG, Gerhard-Herman MD, Holly TA, Kane GC, Marine JE, Nelson MT, Spencer CC, Thompson A, Ting HH, Uretsky BF, Wijeysundera DN. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130(24):2215–45. doi:10.1161/CIR.0000000000000105.
Parikh P, Shiloach M, Cohen ME, Bilimoria KY, Ko CY, Hall BL, Pitt HA. Pancreatectomy risk calculator: an ACS-NSQIP resource. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2010;12(7):488–97. doi:10.1111/j.1477-2574.2010.00216.x.
Epelboym I, Gawlas I, Lee JA, Schrope B, Chabot JA, Allendorf JD. Limitations of ACS-NSQIP in reporting complications for patients undergoing pancreatectomy: underscoring the need for a pancreas-specific module. World J Surg. 2014;38(6):1461–7. doi:10.1007/s00268-013-2439-1.
Pitt HA, Kilbane M, Strasberg SM, Pawlik TM, Dixon E, Zyromski NJ, Aloia TA, Henderson JM, Mulvihill SJ. ACS-NSQIP has the potential to create an HPB-NSQIP option. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2009;11(5):405–13. doi:10.1111/j.1477-2574.2009.00074.x.
Greenblatt DY, Kelly KJ, Rajamanickam V, Wan Y, Hanson T, Rettammel R, Winslow ER, Cho CS, Weber SM. Preoperative factors predict perioperative morbidity and mortality after pancreaticoduodenectomy. Ann Surg Oncol. 2011;18(8):2126–35. doi:10.1245/s10434-011-1594-6.
Mise Y, Day RW, Vauthey JN, Brudvik KW, Schwarz L, Prakash L, Parker NH, Katz MH, Conrad C, Lee JE, Fleming JB, Aloia TA. After pancreatectomy, the "90 days from surgery" definition is superior to the "30 days from discharge" definition for capture of clinically relevant readmissions. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2016;20(1):77–84; discussion 84. doi:10.1007/s11605-015-2984-z.
Strasberg SM, Hall BL. Postoperative morbidity index: a quantitative measure of severity of postoperative complications. J Am Coll Surg. 2011;213(5):616–26. doi:10.1016/j.jamcollsurg.2011.07.019.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
No funding was received for this study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Jiang, H.Y., Kohtakangas, E.L., Asai, K. et al. Predictive Power of the NSQIP Risk Calculator for Early Post-Operative Outcomes After Whipple: Experience from a Regional Center in Northern Ontario. J Gastrointest Canc 49, 288–294 (2018). https://doi.org/10.1007/s12029-017-9949-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-017-9949-2