Abstract
Background
Our objective was to assess the utility of the 1-h suppression ratio (SR) as a biomarker of cerebral injury and neurologic prognosis after cardiac arrest (CA) in the pediatric hospital setting.
Methods
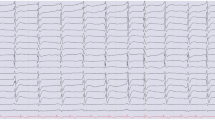
Prospectively, we reviewed data from children presenting after CA and monitored by continuous electroencephalography (cEEG). Patients aged 1 month to 21 years were included. The SR, a quantitative measure of low-voltage cEEG (≤ 3 µV) content, was dichotomized as present or absent if there was > 0% suppression for one continuous hour. A multivariate logistic regression analysis was performed including age, sex, type of CA (i.e., in-hospital or out-of-hospital), and the presence of SR as a predictor of global anoxic cerebral injury as confirmed by magnetic resonance imaging (MRI).
Results
We included 84 patients with a median age of 4 years (interquartile range 0.9–13), 64% were male, and 49% (41/84) had in-hospital CA. Cerebral injury was seen in 50% of patients, of whom 65% had global injury. One-hour SR presence, independent of amount, predicted cerebral injury with 81% sensitivity (95% confidence interval (CI) (66–91%) and 98% specificity (95% CI 88–100%). Multivariate logistic regression analyses indicated that SR was a significant predictor of both cerebral injury (β = 6.28, p < 0.001) and mortality (β = 3.56, p < 0.001).
Conclusions
The SR a sensitive and specific marker of anoxic brain injury and post-CA mortality in the pediatric population. Once detected in the post-CA setting, the 1-h SR may be a useful threshold finding for deployment of early neuroprotective strategies prior or for prompting diagnostic neuroimaging.


Similar content being viewed by others
References
Robinson JA, LaPage MJ, Atallah J, et al. Outcomes of pediatric patients with defibrillators following initial presentation with sudden cardiac arrest. Circ Arrhythm Electrophysiol. 2021;14:e008517.
Topjian AA, de Caen A, Wainwright MS, et al. Pediatric post-cardiac arrest care: a scientific statement from the American Heart Association. Circulation. 2019;140:e194–233.
Herman ST, Abend NS, Bleck TP, et al. Consensus statement on continuous EEG in critically ill adults and children, part I: indications. J Clin Neurophysiol. 2015;32:87–95.
Grundmann S, Busch HJ. Neurologic prognosis after cardiac arrest. N Engl J Med. 2009;361:1999 (author reply 1999–2000).
Nesseler N, Leurent G, Seguin P. Neurologic prognosis after cardiac arrest. N Engl J Med. 2009;361:1999 (author reply 1999–2000).
Young GB. Clinical practice. Neurologic prognosis after cardiac arrest. N Engl J Med. 2009;361:605–11.
Sansevere AJ, DiBacco ML, Akhondi-Asl A, et al. EEG features of brain injury during extracorporeal membrane oxygenation in children. Neurology. 2020;95:e1372–80.
Amorim E, Rittenberger JC, Baldwin ME, Callaway CW, Popescu A, Post Cardiac Arrest S. Malignant EEG patterns in cardiac arrest patients treated with targeted temperature management who survive to hospital discharge. Resuscitation. 2015;90:127–32.
Bevers MB, Scirica BM, Avery KR, Henderson GV, Lin AP, Lee JW. Combination of clinical exam, MRI and EEG to predict outcome following cardiac arrest and targeted temperature management. Neurocrit Care. 2018;29:396–403.
Ostendorf AP, Hartman ME, Friess SH. Early electroencephalographic findings correlate with neurologic outcome in children following cardiac arrest. Pediatr Crit Care Med. 2016;17:667–76.
Lee S, Zhao X, Davis KA, Topjian AA, Litt B, Abend NS. Quantitative EEG predicts outcomes in children after cardiac arrest. Neurology. 2019;92:e2329–38.
Sansevere AJ, Hahn CD, Abend NS. Conventional and quantitative EEG in status epilepticus. Seizure. 2019;68:38–45.
Stewart CP, Otsubo H, Ochi A, Sharma R, Hutchison JS, Hahn CD. Seizure identification in the ICU using quantitative EEG displays. Neurology. 2010;75:1501–8.
Swisher CB, Sinha SR. Utilization of quantitative EEG trends for critical care continuous EEG monitoring: a survey of neurophysiologists. J Clin Neurophysiol. 2016;33:538–44.
Du Pont-Thibodeau G, Sanchez SM, Jawad AF, et al. Seizure detection by critical care providers using amplitude-integrated electroencephalography and color density spectral array in pediatric cardiac arrest patients. Pediatr Crit Care Med. 2017;18:363–9.
Topjian AA, Fry M, Jawad AF, et al. Detection of electrographic seizures by critical care providers using color density spectral array after cardiac arrest is feasible. Pediatr Crit Care Med. 2015;16:461–7.
Dell’anna AM, Scolletta S, Donadello K, Taccone FS. Early neuroprotection after cardiac arrest. Curr Opin Crit Care. 2014;20:250–8.
Hirsch LJ, Fong MWK, Leitinger M, et al. American clinical neurophysiology society’s standardized critical care EEG terminology: 2021 version. J Clin Neurophysiol. 2021;38:1–29.
Hirsch LJ, LaRoche SM, Gaspard N, et al. American clinical neurophysiology society’s standardized critical care EEG terminology: 2012 version. J Clin Neurophysiol. 2013;30:1–27.
Abend NS, Gutierrez-Colina A, Zhao H, et al. Interobserver reproducibility of electroencephalogram interpretation in critically ill children. J Clin Neurophysiol. 2011;28:15–9.
Lewis DW, Johnson EL. Prognosis of periodic and rhythmic patterns in adult and pediatric populations. J Clin Neurophysiol. 2018;35:303–8.
Babcock DS, Han BK, Weiss RG, Ryckman FC. Brain abnormalities in infants on extracorporeal membrane oxygenation: sonographic and CT findings. AJR Am J Roentgenol. 1989;153:571–6.
LaRovere KL, Vonberg FW, Prabhu SP, et al. Patterns of head computed tomography abnormalities during pediatric extracorporeal membrane oxygenation and association with outcomes. Pediatr Neurol. 2017;73:64–70.
Sansevere AJ, Arya R, Sanchez Fernandez I, et al. Electroencephalographic reporting for refractory status epilepticus. J Clin Neurophysiol. 2019;36:365–70.
Abend NS, Topjian A, Ichord R, et al. Electroencephalographic monitoring during hypothermia after pediatric cardiac arrest. Neurology. 2009;72:1931–40.
Sansevere AJ, DiBacco ML, Pearl PL, Rotenberg A. Quantitative electroencephalography for early detection of elevated intracranial pressure in critically Ill children: case series and proposed protocol. J Child Neurol. 2022;37:5–11.
Munjal NK, Bergman I, Scheuer ML, Genovese CR, Simon DW, Patterson CM. Quantitative electroencephalography (EEG) predicting acute neurologic deterioration in the pediatric intensive care unit: a case series. J Child Neurol. 2022;37:73–9.
Ducharme-Crevier L, Press CA, Kurz JE, Mills MG, Goldstein JL, Wainwright MS. Early presence of sleep spindles on electroencephalography is associated with good outcome after pediatric cardiac arrest. Pediatr Crit Care Med. 2017;18:452–60.
Menache CC, Bourgeois BF, Volpe JJ. Prognostic value of neonatal discontinuous EEG. Pediatr Neurol. 2002;27:93–101.
Korotchikova I, Stevenson NJ, Walsh BH, Murray DM, Boylan GB. Quantitative EEG analysis in neonatal hypoxic ischaemic encephalopathy. Clin Neurophysiol. 2011;122:1671–8.
van’t Westende C, Geraedts VJ, van Ramesdonk T, et al. Neonatal quantitative electroencephalography and long-term outcomes: a systematic review. Dev Med Child Neurol. 2022;64:413–20.
Doyle OM, Greene BR, Murray DM, Marnane L, Lightbody G, Boylan GB. The effect of frequency band on quantitative EEG measures in neonates with hypoxic-ischaemic encephalopathy. Annu Int Conf IEEE Eng Med Biol Soc. 2007;2007:717–21.
Kota S, Massaro AN, Chang T, et al. Prognostic value of continuous electroencephalogram delta power in neonates with hypoxic-ischemic encephalopathy. J Child Neurol. 2020;35:517–25.
Press CA, Morgan L, Mills M, et al. Spectral electroencephalogram analysis for the evaluation of encephalopathy grade in children with acute liver failure. Pediatr Crit Care Med. 2017;18:64–72.
Funding
This study is not funded.
Author information
Authors and Affiliations
Contributions
AJS participated in conception, study design, data collection, data analysis, manuscript preparation, editing and submission. As the primary author AJS takes full responsibility for all aspects of this work. AJ participated in study design, data analysis, manuscript preparation editing, and approval. MLD participated in study design, data collection, manuscript preparation, editing, and approval. KC participated in study design, data collection, manuscript preparation editing, and approval. AR participated in conception, study design, manuscript preparation, editing, and approval.
Corresponding author
Ethics declarations
Conflicts of interest
Melissa DiBacco is supported in part by the National Institute of Health/National Institute of Neurological Disorders and Stroke (R01 HD 091142). Dr. DiBacco is now employed at Agios Pharmaceuticals. The work represented in this article was completed prior to employment at Agios Pharmaceuticals, and there is no conflict of interest with the work represented in this article. For the remaining authors, no conflicts were declared.
Ethical Approval/Informed Consent
This article has not been submitted or published elsewhere and adheres to all ethical guidelines. This is an institution review board–approved study at our institution.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sansevere, A.J., Janatti, A., DiBacco, M.L. et al. Background EEG Suppression Ratio for Early Detection of Cerebral Injury in Pediatric Cardiac Arrest. Neurocrit Care (2024). https://doi.org/10.1007/s12028-023-01920-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12028-023-01920-0