Abstract
Background
Many children with severe traumatic brain injury (TBI) receive magnetic resonance imaging (MRI) during hospitalization. There are insufficient data on how different patterns of injury on early MRI inform outcomes.
Methods
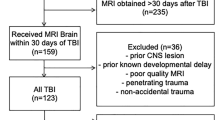
Children (3–17 years) admitted in 2010–2021 for severe TBI (Glasgow Coma Scale [GCS] score < 9) were identified using our site’s trauma registry. We used multivariable modeling to determine whether the hemorrhagic diffuse axonal injury (DAI) grade and the number of regions with restricted diffusion (subcortical white matter, corpus callosum, deep gray matter, and brainstem) on MRI obtained within 7 days of injury were independently associated with time to follow commands and with Functional Independence Measure for Children (WeeFIM) scores at the time of discharge from inpatient rehabilitation. We controlled for the clinical variables age, preadmission cardiopulmonary resuscitation, pupil reactivity, motor GCS score, and fever (> 38 °C) in the first 12 h.
Results
Of 260 patients, 136 (52%) underwent MRI within 7 days of injury at a median of 3 days (interquartile range [IQR] 2–4). Patients with early MRI were a median age of 11 years (IQR 7–14), 8 (6%) patients received cardiopulmonary resuscitation, 19 (14%) patients had bilateral unreactive pupils, the median motor GCS score was 1 (IQR 1–4), and 82 (60%) patients had fever. Grade 3 DAI was present in 46 (34%) patients, and restricted diffusion was noted in the corpus callosum in 75 (55%) patients, deep gray matter in 29 (21%) patients, subcortical white matter in 23 (17%) patients, and the brainstem in 20 (15%) patients. After controlling for clinical variables, an increased number of regions with restricted diffusion, but not hemorrhagic DAI grade, was independently associated with longer time to follow commands (hazard ratio 0.68, 95% confidence interval 0.53–0.89) and worse WeeFIM scores (estimate β − 4.67, 95% confidence interval − 8.33 to − 1.01).
Conclusions
Regional restricted diffusion on early MRI is independently associated with short-term outcomes in children with severe TBI. Multicenter cohort studies are needed to validate these findings and elucidate the association of early MRI features with long-term outcomes in children with severe TBI.



Similar content being viewed by others
References
Coronado VG, Xu L, Basavaraju SV, et al. Surveillance for traumatic brain injury-related deaths—United States, 1997–2007. MMWR Surveill Summ. 2011;60(5):1–32.
Faul M, Coronado V. Epidemiology of traumatic brain injury. Handb Clin Neurol. 2015;127:3–13. https://doi.org/10.1016/B978-0-444-52892-6.00001-5.
Aitken ME, McCarthy ML, Slomine BS, et al. Family burden after traumatic brain injury in children. Pediatrics. 2009;123(1):199–206. https://doi.org/10.1542/peds.2008-0607.
Kirschen MP, Walter JK. Ethical issues in neuroprognostication after severe pediatric brain injury. Semin Pediatr Neurol. 2015;22(3):187–95. https://doi.org/10.1016/j.spen.2015.05.004.
Suskauer SJ, Huisman TA. Neuroimaging in pediatric traumatic brain injury: current and future predictors of functional outcome. Dev Disabil Res Rev. 2009;15(2):117–23. https://doi.org/10.1002/ddrr.62.
Kochanek PM, Tasker RC, Carney N, et al. Guidelines for the management of pediatric severe traumatic brain injury, third edition: update of the brain trauma foundation guidelines. Pediatr Crit Care Med. 2019;20(3S Supp1 1):S1–82. https://doi.org/10.1097/PCC.0000000000001735.
Ferrazzano PA, Rosario BL, Wisniewski SR, et al. Use of magnetic resonance imaging in severe pediatric traumatic brain injury: assessment of current practice. J Neurosurg Pediatr. 2019;23(4):471–9. https://doi.org/10.3171/2018.10.PEDS18374.
Babikian T, Freier MC, Tong KA, et al. Susceptibility weighted imaging: neuropsychologic outcome and pediatric head injury. Pediatr Neurol. 2005;33(3):184–94. https://doi.org/10.1016/j.pediatrneurol.2005.03.015.
Babikian T, Tong KA, Galloway NR, Freier-Randall MC, Obenaus A, Ashwal S. Diffusion-weighted imaging predicts cognition in pediatric brain injury. Pediatr Neurol. 2009;41(6):406–12. https://doi.org/10.1016/j.pediatrneurol.2009.06.002.
Galloway NR, Tong KA, Ashwal S, Oyoyo U, Obenaus A. Diffusion-weighted imaging improves outcome prediction in pediatric traumatic brain injury. J Neurotrauma. 2008;25(10):1153–62. https://doi.org/10.1089/neu.2007.0494.
Smitherman E, Hernandez A, Stavinoha PL, et al. Predicting outcome after pediatric traumatic brain injury by early magnetic resonance imaging lesion location and volume. J Neurotrauma. 2016;33(1):35–48. https://doi.org/10.1089/neu.2014.3801.
Janas AM, Qin F, Hamilton S, et al. Diffuse axonal injury grade on early MRI is associated with worse outcome in children with moderate-severe traumatic brain injury. Neurocrit Care. 2022;36(2):492–503. https://doi.org/10.1007/s12028-021-01336-8.
Liu AY, Maldjian JA, Bagley LJ, Sinson GP, Grossman RI. Traumatic brain injury: diffusion-weighted MR imaging findings. AJNR Am J Neuroradiol. 1999;20(9):1636–41.
Katayama Y, Becker DP, Tamura T, Hovda DA. Massive increases in extracellular potassium and the indiscriminate release of glutamate following concussive brain injury. J Neurosurg. 1990;73(6):889–900. https://doi.org/10.3171/jns.1990.73.6.0889.
Katayama Y, Becker DP, Tamura T, Ikezaki K. Early cellular swelling in experimental traumatic brain injury: a phenomenon mediated by excitatory amino acids. Acta Neurochir Suppl (Wien). 1990;51:271–3. https://doi.org/10.1007/978-3-7091-9115-6_92.
Hovda DA, Becker DP, Katayama Y. Secondary injury and acidosis. J Neurotrauma. 1992;9(Suppl 1):S47-60.
Barzó P, Marmarou A, Fatouros P, Corwin F, Dunbar J. Magnetic resonance imaging-monitored acute blood-brain barrier changes in experimental traumatic brain injury. J Neurosurg. 1996;85(6):1113–21. https://doi.org/10.3171/jns.1996.85.6.1113.
Ewing-Cobbs L, Prasad M, Kramer L, et al. Acute neuroradiologic findings in young children with inflicted or noninflicted traumatic brain injury. Childs Nerv Syst 2000;16(1):25–33; discussion 34. https://doi.org/10.1007/s003810050006.
Gentry LR. Imaging of closed head injury. Radiology. 1994;191(1):1–17. https://doi.org/10.1148/radiology.191.1.8134551.
Ahmad I. “T2 shine through effect” of vasogenic oedema on DWI. J Coll Physicians Surg Pak. 2013;23(4):311.
Hammoud DA, Wasserman BA. Diffuse axonal injuries: pathophysiology and imaging. Neuroimaging Clin N Am. 2002;12(2):205–16. https://doi.org/10.1016/s1052-5149(02)00011-4.
Msall ME, DiGaudio K, Rogers BT, et al. The Functional Independence Measure for Children (WeeFIM). Conceptual basis and pilot use in children with developmental disabilities. Clin Pediatr (Phila). 1994;33(7):421–30. https://doi.org/10.1177/000992289403300708.
Msall ME, Tremont MR. Measuring functional status in children with genetic impairments. Am J Med Genet. 1999;89(2):62–74. https://doi.org/10.1002/(sici)1096-8628(19990625)89:2%3c62::aid-ajmg3%3e3.0.co;2-t.
Ziviani J, Ottenbacher KJ, Shephard K, Foreman S, Astbury W, Ireland P. Concurrent validity of the Functional Independence Measure for Children (WeeFIM) and the pediatric evaluation of disabilities inventory in children with developmental disabilities and acquired brain injuries. Phys Occup Ther Pediatr. 2001;21(2–3):91–101.
Msall ME, DiGaudio K, Duffy LC, LaForest S, Braun S, Granger CV. WeeFIM. Normative sample of an instrument for tracking functional independence in children. Clin Pediatr (Phila). 1994;33(7):431–8. https://doi.org/10.1177/000992289403300709.
Calkins CM, Bensard DD, Partrick DA, Karrer FM. A critical analysis of outcome for children sustaining cardiac arrest after blunt trauma. J Pediatr Surg. 2002;37(2):180–4. https://doi.org/10.1053/jpsu.2002.30251.
Hazinski MF, Chahine AA, Holcomb GW 3rd, Morris JA Jr. Outcome of cardiovascular collapse in pediatric blunt trauma. Ann Emerg Med. 1994;23(6):1229–35. https://doi.org/10.1016/s0196-0644(94)70346-9.
Hickey RW, Cohen DM, Strausbaugh S, Dietrich AM. Pediatric patients requiring CPR in the prehospital setting. Ann Emerg Med. 1995;25(4):495–501. https://doi.org/10.1016/s0196-0644(95)70265-2.
Martin SK, Shatney CH, Sherck JP, et al. Blunt trauma patients with prehospital pulseless electrical activity (PEA): poor ending assured. J Trauma 2002;53(5):876–80; discussion 880–1. https://doi.org/10.1097/00005373-200211000-00011.
Natale JE, Joseph JG, Helfaer MA, Shaffner DH. Early hyperthermia after traumatic brain injury in children: risk factors, influence on length of stay, and effect on short-term neurologic status. Crit Care Med. 2000;28(7):2608–15. https://doi.org/10.1097/00003246-200007000-00071.
Perron AD, Sing RF, Branas CC, Huynh T. Predicting survival in pediatric trauma patients receiving cardiopulmonary resuscitation in the prehospital setting. Prehosp Emerg Care. 2001;5(1):6–9. https://doi.org/10.1080/10903120190940245.
Suz P, Vavilala MS, Souter M, Muangman S, Lam AM. Clinical features of fever associated with poor outcome in severe pediatric traumatic brain injury. J Neurosurg Anesthesiol. 2006;18(1):5–10. https://doi.org/10.1097/01.ana.0000189079.26212.37.
Zwingmann J, Mehlhorn AT, Hammer T, Bayer J, Südkamp NP, Strohm PC. Survival and neurologic outcome after traumatic out-of-hospital cardiopulmonary arrest in a pediatric and adult population: a systematic review. Crit Care. 2012;16(4):R117. https://doi.org/10.1186/cc11410.
Mikkonen ED, Skrifvars MB, Reinikainen M, et al. Validation of prognostic models in intensive care unit-treated pediatric traumatic brain injury patients. J Neurosurg Pediatr. 2019. https://doi.org/10.3171/2019.4.Peds1983.
Bao L, Chen D, Ding L, Ling W, Xu F. Fever burden is an independent predictor for prognosis of traumatic brain injury. PLoS ONE. 2014;9(3): e90956. https://doi.org/10.1371/journal.pone.0090956.
Li J, Jiang JY. Chinese Head Trauma Data Bank: effect of hyperthermia on the outcome of acute head trauma patients. J Neurotrauma. 2012;29(1):96–100. https://doi.org/10.1089/neu.2011.1753.
Heagerty PJ, Lumley T, Pepe MS. Time-dependent ROC curves for censored survival data and a diagnostic marker. Biometrics. 2000;56(2):337–44. https://doi.org/10.1111/j.0006-341x.2000.00337.x.
Tong KA, Ashwal S, Holshouser BA, et al. Diffuse axonal injury in children: clinical correlation with hemorrhagic lesions. Ann Neurol. 2004;56(1):36–50. https://doi.org/10.1002/ana.20123.
Zheng WB, Liu GR, Li LP, Wu RH. Prediction of recovery from a post-traumatic coma state by diffusion-weighted imaging (DWI) in patients with diffuse axonal injury. Neuroradiology. 2007;49(3):271–9. https://doi.org/10.1007/s00234-006-0187-8.
Mohamadpour M, Whitney K, Bergold PJ. The importance of therapeutic time window in the treatment of traumatic brain injury. Front Neurosci. 2019;13:07. https://doi.org/10.3389/fnins.2019.00007.
Diaz-Arrastia R, Kochanek PM, Bergold P, et al. Pharmacotherapy of traumatic brain injury: state of the science and the road forward: report of the Department of Defense Neurotrauma Pharmacology Workgroup. J Neurotrauma. 2014;31(2):135–58. https://doi.org/10.1089/neu.2013.3019.
Molteni E, Ranzini MBM, Beretta E, Modat M, Strazzer S. Individualized prognostic prediction of the long-term functional trajectory in pediatric acquired brain injury. J Pers Med. 2021. https://doi.org/10.3390/jpm11070675.
Rubin ML, Yamal JM, Chan W, Robertson CS. Prognosis of six-month glasgow outcome scale in severe traumatic brain injury using hospital admission characteristics, injury severity characteristics, and physiological monitoring during the first day post-injury. J Neurotrauma. 2019;36(16):2417–22. https://doi.org/10.1089/neu.2018.6217.
Davis KC, Slomine BS, Salorio CF, Suskauer SJ. Time to follow commands and duration of posttraumatic amnesia predict GOS-E peds scores 1 to 2 years after TBI in children requiring inpatient rehabilitation. J Head Trauma Rehabil. 2016;31(2):E39-47. https://doi.org/10.1097/htr.0000000000000159.
Lundine JP, Koterba C, Shield C, Shi J, Hoskinson KR. Predicting outcomes 2 months and 1 year after inpatient rehabilitation for youth with TBI using duration of impaired consciousness and serial cognitive assessment. J Head Trauma Rehabil. 2023;38(2):E99-e108. https://doi.org/10.1097/htr.0000000000000784.
Austin CA, Slomine BS, Dematt EJ, Salorio CF, Suskauer SJ. Time to follow commands remains the most useful injury severity variable for predicting WeeFIM® scores 1 year after paediatric TBI. Brain Inj. 2013;27(9):1056–62. https://doi.org/10.3109/02699052.2013.794964.
Slomine BS, Suskauer SJ, Nicholson R, Giacino JT. Preliminary validation of the coma recovery scale for pediatrics in typically developing young children. Brain Inj. 2019;33(13–14):1640–5. https://doi.org/10.1080/02699052.2019.1658221.
Funding
Analytic support was provided by the University of Colorado Section of Pediatric Critical Care. Dr. Maddux received support from the Eunice Kennedy Shriver National Institutes of Health and Human Development (K23HD096018).
Author information
Authors and Affiliations
Contributions
AMJ, KRM, and ABM designed the research; KRM performed the statistical analysis; AMJ, NVS, and JMW collected data; all authors contributed to the interpretation of the data; AMJ drafted the manuscript; all authors made critical revisions to the manuscript for intellectual content; AMJ had primary responsibility for the final content; and all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical Approval/Informed Consent
The study was approved by the Colorado Multiple Institutional Review Board (protocol #22-1376) and was conducted in accordance with institutional guidelines. Consent was not required (retrospective study).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Janas, A.M., Miller, K.R., Stence, N.V. et al. Utility of Early Magnetic Resonance Imaging to Enhance Outcome Prediction in Critically Ill Children with Severe Traumatic Brain Injury. Neurocrit Care (2023). https://doi.org/10.1007/s12028-023-01898-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12028-023-01898-9