Abstract
Background
Patients with intracerebral hemorrhage (ICH) related to cerebral amyloid angiopathy (CAA) are at increased risk of developing epilepsy and cognitive disorders such as Alzheimer’s disease (AD), mild cognitive impairment (MCI), and vascular dementia. In a retrospective cohort observation study of patients hospitalized for ICH with CAA versus ICH without CAA, we evaluated the prevalence of neurological comorbidities at admission and the risk of new diagnosis of epilepsy, relevant cognitive disorders, and mortality at 1 year.
Methods
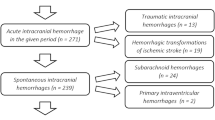
In the TriNetX health research network, adult patients aged ≥ 55 years hospitalized with a diagnosis of ICH were stratified based on presence or absence of concomitant CAA diagnosis. Demographics and medical comorbidities were compared by using χ2 test and Student’s t-test. After 1:1 propensity score matching, 1-year survival was assessed with Kaplan–Meier curves. The 1-year risk of new diagnosis of epilepsy, AD, MCI, vascular dementia, and dementia unspecified was assessed with Cox proportional hazards estimate.
Results
The study included a total of 1757 patients with ICH and CAA and 53,364 patients with ICH without CAA. Patients with CAA were older compared with those without CAA (74.1 ± 7.5 vs. 69.8 ± 8.8 years, p ≤ 0.001). Compared with ICH without CAA, patients with ICH and CAA had higher baseline prevalence of cerebral infarction (30% vs. 20%), nontraumatic ICH (36% vs. 7%), nontraumatic subarachnoid hemorrhage (14% vs. 5%), epilepsy (11% vs. 6%), and AD (5% vs. 2%) with significance at p < 0.001. After propensity score matching, a total of 1746 patients were included in both cohorts. In the matched cohorts, compared with patients with ICH without CAA, patients with ICH and CAA had lower 1-year all-cause mortality (479 [27%] vs. 563 [32%]; hazard ratio [HR] 0.80; 95% confidence interval [CI] 0.71–0.90) and higher risk of new diagnosis of epilepsy (280 [18%] vs. 167 [11%]; HR 1.70; 95% CI 1.40–2.06), AD (101 [6%] vs. 38 [2%]; HR 2.62; 95% CI 1.80–3.80), MCI (85 [5%] vs. 35 [2%]; HR 2.39; 95% CI 1.61–3.54), vascular dementia (117 [7%] vs. 60 [4%]; HR 1.92; 95% CI 1.41–2.62), and dementia unspecified (245 [16%] vs. 150 [9%]; HR 1.70; 95% CI 1.39–2.08).
Conclusions
Among patients admitted for ICH, patients with CAA have lower mortality but have 2–3 times more risk of diagnosis of epilepsy and dementia at 1 year, compared with those without CAA.


Similar content being viewed by others
References
Roh D, Sun CH, Schmidt JM, et al. Primary intracerebral hemorrhage: a closer look at hypertension and cerebral amyloid angiopathy. Neurocrit Care. 2018;29(1):77–83. https://doi.org/10.1007/s12028-018-0514-z.
Nagaraja N, Patel UK. Disparities in diagnosis of cerebral amyloid angiopathy based on hospital characteristics. J Clin Neurosci Off J Neurosurg Soc Australas. 2021;89:39–42.
Charidimou A, Imaizumi T, Moulin S, et al. Brain hemorrhage recurrence, small vessel disease type, and cerebral microbleeds: a meta-analysis. Neurology. 2017;89(8):820–9. https://doi.org/10.1212/WNL.0000000000004259.
Garg A, Ortega-Gutierrez S, Farooqui M, Nagaraja N. Recurrent intracerebral hemorrhage in patients with cerebral amyloid angiopathy: a propensity-matched case-control study. J Neurol. 2022;269(4):2200–5. https://doi.org/10.1007/s00415-021-10937-4.
Che R, Zhang M, Sun H, et al. Long-term outcome of cerebral amyloid angiopathy-related hemorrhage. CNS Neurosci Ther. 2022. https://doi.org/10.1111/cns.13922.
Derex L, Rheims S, Peter-Derex L. Seizures and epilepsy after intracerebral hemorrhage: an update. J Neurol. 2021;268(7):2605–15. https://doi.org/10.1007/s00415-021-10439-3.
Biffi A, Rattani A, Anderson CD, et al. Delayed seizures after intracerebral haemorrhage. Brain. 2016;139(Pt 10):2694–705. https://doi.org/10.1093/brain/aww199.
Stefanidou M, Beiser AS, Himali JJ, et al. Bi-directional association between epilepsy and dementia: the Framingham heart study. Neurology. 2020;95(24):e3241–7. https://doi.org/10.1212/WNL.0000000000011077.
Zhang D, Chen S, Xu S, et al. The clinical correlation between Alzheimer’s disease and epilepsy. Front Neurol. 2022;13:922535. https://doi.org/10.3389/fneur.2022.922535.
Thom M, Liu JY, Thompson P, et al. Neurofibrillary tangle pathology and Braak staging in chronic epilepsy in relation to traumatic brain injury and hippocampal sclerosis: a post-mortem study. Brain. 2011;134(Pt 10):2969–81. https://doi.org/10.1093/brain/awr209.
Vossel KA, Ranasinghe KG, Beagle AJ, et al. Incidence and impact of subclinical epileptiform activity in Alzheimer’s disease. Ann Neurol. 2016;80(6):858–70. https://doi.org/10.1002/ana.24794.
Greenberg SM, Bacskai BJ, Hernandez-Guillamon M, Pruzin J, Sperling R, van Veluw SJ. Cerebral amyloid angiopathy and Alzheimer disease: one peptide, two pathways. Nat Rev Neurol. 2020;16(1):30–42. https://doi.org/10.1038/s41582-019-0281-2.
Kaiser J, Schebesch KM, Brawanski A, Linker RA, Schlachetzki F, Wagner A. Long-term follow-up of cerebral amyloid angiopathy-associated intracranial hemorrhage reveals a high prevalence of atrial fibrillation. J Stroke Cerebrovasc Dis Off J Natl Stroke Assoc. 2019;28(11):104342. https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.104342.
Wang W, Kaelber DC, Xu R, Berger NA. Breakthrough SARS-CoV-2 infections, hospitalizations, and mortality in vaccinated patients with cancer in the US between December 2020 and November 2021. JAMA Oncol. 2022;8(7):1027–34. https://doi.org/10.1001/jamaoncol.2022.1096.
Haukoos JS, Lewis RJ. The propensity score. J Am Med Assoc. 2015;314(15):1637–8. https://doi.org/10.1001/jama.2015.13480.
van Etten ES, Gurol ME, van der Grond J, et al. Recurrent hemorrhage risk and mortality in hereditary and sporadic cerebral amyloid angiopathy. Neurology. 2016;87(14):1482–7. https://doi.org/10.1212/WNL.0000000000003181.
Calviere L, Viguier A, Patsoura S, et al. Risk of intracerebral hemorrhage and mortality after convexity subarachnoid hemorrhage in cerebral amyloid angiopathy. Stroke J Cereb Circ. 2019;50(9):2562–4. https://doi.org/10.1161/STROKEAHA.119.026244.
Poon MT, Fonville AF, Al-Shahi SR. Long-term prognosis after intracerebral haemorrhage: systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2014;85(6):660–7. https://doi.org/10.1136/jnnp-2013-306476.
Fernando SM, Qureshi D, Talarico R, et al. Intracerebral hemorrhage incidence, mortality, and association with oral anticoagulation use: a population study. Stroke J Cereb Circ. 2021;52(5):1673–81. https://doi.org/10.1161/STROKEAHA.120.032550.
Lahti AM, Saloheimo P, Huhtakangas J, et al. Poststroke epilepsy in long-term survivors of primary intracerebral hemorrhage. Neurology. 2017;88(23):2169–75. https://doi.org/10.1212/WNL.0000000000004009.
Chen J, Ye H, Zhang J, Li A, Ni Y. Pathogenesis of seizures and epilepsy after stroke. Acta Epileptol. 2022;4(1):2. https://doi.org/10.1186/s42494-021-00068-8.
Lin HY, Wei QQ, Huang JY, et al. Relationship between mortality and seizures after intracerebral hemorrhage: a systematic review and meta-analysis. Front Neurol. 2022;13:922677. https://doi.org/10.3389/fneur.2022.922677.
Jakel L, De Kort AM, Klijn CJM, Schreuder F, Verbeek MM. Prevalence of cerebral amyloid angiopathy: a systematic review and meta-analysis. Alzheimers Dement. 2022;18(1):10–28. https://doi.org/10.1002/alz.12366.
Greenberg SM, Charidimou A. Diagnosis of cerebral amyloid angiopathy: evolution of the Boston criteria. Stroke J Cereb Circ. 2018;49(2):491–7. https://doi.org/10.1161/STROKEAHA.117.016990.
Moulin S, Labreuche J, Bombois S, et al. Dementia risk after spontaneous intracerebral haemorrhage: a prospective cohort study. Lancet Neurol. 2016;15(8):820–9. https://doi.org/10.1016/S1474-4422(16)00130-7.
Greenberg SM, Vonsattel JP. Diagnosis of cerebral amyloid angiopathy. Sensitivity and specificity of cortical biopsy. Stroke J Cereb Circ. 1997;28(7):1418–22. https://doi.org/10.1161/01.str.28.7.1418.
McCormick N, Bhole V, Lacaille D, Avina-Zubieta JA. Validity of diagnostic codes for acute stroke in administrative databases: a systematic review. PLoS ONE. 2015;10(8):e0135834. https://doi.org/10.1371/journal.pone.0135834.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
NN: Conception and study design, data analysis and interpretation, drafting and revising the article, final approval of version to be published. V Ballur Narayana Reddy: Conception and study design, interpretation of data, drafting and revising the article for important intellectual content, final approval of version to be published.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Ethical approval/informed consent
Authors confirm adherence to ethical guidelines. Institutional review board approval was not required for this study. The study was performed using TriNetX database that uses deidentified aggregate patient data for analysis. No protected health information or personal data are made available to the users of the platform.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nagaraja, N., Ballur Narayana Reddy, V. Prevalence of Concomitant Neurological Disorders and Long-Term Outcome of Patients Hospitalized for Intracerebral Hemorrhage with Versus without Cerebral Amyloid Angiopathy. Neurocrit Care 40, 486–494 (2024). https://doi.org/10.1007/s12028-023-01753-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-023-01753-x