Abstract
Background
Prior studies show hospital admission volume to be associated with poor outcomes following elective procedures and inpatient medical hospitalizations. However, it is unknown whether hospital volume impacts Inpatient outcomes for status epilepticus (SE) hospitalizations. In this study, we aimed to assess the impact of hospital volume on the outcome of patients with SE and related inpatient medical complications.
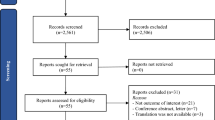
Methods
The 2005 to 2013 National Inpatient Sample database was queried using International Classification of Diseases 9th Edition diagnosis code 345.3 to identify patients undergoing acute hospitalization for SE. The National Inpatient Sample hospital identifier was used as a unique facility identifier to calculate the average volume of patients with SE seen in a year. The study cohort was divided into three groups: low volume (0–7 patients with SE per year), medium volume (8–22 patients with SE per year), and high volume (> 22 patients with SE per year). Multivariate logistic regression analyses were used to assess whether medium or high hospital volume had lower rates of inpatient medical complications compared with low-volume hospitals.
Results
A total of 137,410 patients with SE were included in the analysis. Most patients (n = 50,939; 37%) were treated in a low-volume hospital, 31% (n = 42,724) were treated in a medium-volume facility, and 18% (n = 25,207) were treated in a high-volume hospital. Patients undergoing treatment at medium-volume hospitals (vs. low-volume hospitals) had higher odds of pulmonary complications (odds ratio [OR] 1.18 [95% confidence interval {CI} 1.12–1.25]; p < 0.001), sepsis (OR 1.24 [95% CI 1.08–1.43] p = 0.002), and length of stay (OR 1.13 [95% CI 1.0 –1.19] p < 0.001). High-volume hospitals had significantly higher odds of urinary tract infections (OR 1.21 [95% CI 1.11–1.33] p < 0.001), pulmonary complications (OR 1.19 [95% CI 1.10–1.28], p < 0.001), thrombosis (OR 2.13 [95% CI 1.44–3.14], p < 0.001), and renal complications (OR 1.21 [95% CI 1.07–1.37], p = 0.002). In addition, high-volume hospitals had lower odds of metabolic (OR 0.81 [95% CI 0.72–0.91], p < 0.001), neurological complications (OR 0.80 [95% CI 0.69–0.93], p = 0.004), and disposition to a facility (OR 0.89 [95% CI 0.82–0.96], p < 0.001) compared with lower-volume hospitals.
Conclusions
Our study demonstrates certain associations between hospital volume and outcomes for SE hospitalizations. Further studies using more granular data about the type, severity, and duration of SE and types of treatment are warranted to better understand how hospital volume may impact care and prognosis of patients.
Similar content being viewed by others
References
Chee TT, Ryan AM, Wasfy JH, Borden WB. Current State of Value-Based Purchasing Programs. Circulation. 2016;133:2197–205.
Squitieri L, Bozic KJ, Pusic AL. The role of patient-reported outcome measures in value-based payment reform. Value Health. 2017;20:834–6.
Cowan RA, O’Cearbhaill RE, Gardner GJ, et al. Is it time to centralize ovarian cancer care in the United States? Ann Surg Oncol. 2016;23:989–93.
Casey MF, Wisnivesky J, Le VH, et al. The relationship between centralization of care and geographic barriers to cystectomy for bladder cancer. Bladder Cancer. 2016;2:319–27.
Aquina CT, Probst CP, Becerra AZ, et al. High volume improves outcomes: the argument for centralization of rectal cancer surgery. Surgery. 2016;159:736–48.
Siemens DR, Visram K, Wei X, Booth C. Effect of centralization on complex surgical care: A population-based case study of radical cystectomy. Can Urol Assoc J. 2020;14:91–6.
Vonlanthen R, Lodge P, Barkun JS, et al. Toward a Consensus on Centralization in Surgery. Ann Surg. 2018;268:712–24.
Io M. Interpreting the volume-outcome relationship in the context of health care quality: workshop summary. Washington, DC: The National Academies Press; 2000.
Hastrup S, Johnsen SP, Terkelsen T, et al. Effects of centralizing acute stroke services: a prospective cohort study. Neurology. 2018;91:e236–48.
Ostermann M, Vincent JL. How much centralization of critical care services in the era of telemedicine? Crit Care. 2019;23:423.
Saposnik G, Baibergenova A, O’Donnell M, et al. Hospital volume and stroke outcome: does it matter? Neurology. 2007;69:1142–51.
Horvath L, Fekete I, Molnar M, Valoczy R, Marton S, Fekete K. The outcome of status epilepticus and long-term follow-up. Front Neurol. 2019;10:427.
Lu M, Faure M, Bergamasco A, et al. Epidemiology of status epilepticus in the United States: a systematic review. Epilepsy Behav. 2020;112:107459.
Betjemann JP, Josephson SA, Lowenstein DH, Burke JF. Trends in status epilepticus-related hospitalizations and mortality: redefined in us practice over time. JAMA Neurol. 2015;72:650–5.
Hocker SE, Britton JW, Mandrekar JN, Wijdicks EF, Rabinstein AA. Predictors of outcome in refractory status epilepticus. JAMA Neurol. 2013;70:72–7.
Claassen J, Lokin JK, Fitzsimmons B-FM, Mendelsohn FA, Mayer SA. Predictors of functional disability and mortality after status epilepticus. Neurology. 2002;58:139–42.
Goz V, Weinreb JH, Schwab F, Lafage V, Errico TJ. Comparison of complications, costs, and length of stay of three different lumbar interbody fusion techniques: an analysis of the Nationwide Inpatient Sample database. Spine J. 2014;14:2019–27.
Malik AT, Phillips FM, Kim J, Yu E, Khan SN. Posterior lumbar fusions at physician-owned hospitals - is it time to reconsider the restrictions of the Affordable Care Act? Spine J. 2019;19:1566–72.
Poorthuis MHF, Brand EC, Halliday A, Bulbulia R, Bots ML, de Borst GJ. High operator and hospital volume are associated with a decreased risk of death and stroke after carotid revascularization: a systematic review and meta-analysis. Ann Surg. 2019;269:631–41.
Wilson CT, Fisher ES, Welch HG, Siewers AE, Lucas FLUS. trends in CABG hospital volume: the effect of adding cardiac surgery programs. Health Aff (Millwood). 2007;26:162–8.
Chou YY, Hwang JJ, Tung YC. Optimal surgeon and hospital volume thresholds to reduce mortality and length of stay for CABG. PLoS ONE. 2021;16:e0249750.
Gutacker N, Bloor K, Cookson R, et al. Hospital surgical volumes and mortality after coronary artery bypass grafting: using international comparisons to determine a safe threshold. Health Serv Res. 2017;52:863–78.
Anis HK, Mahmood BM, Klika AK, et al. Hospital volume and postoperative infections in total knee arthroplasty. J Arthroplasty. 2020;35:1079–83.
Jeschke E, Citak M, Gunster C, et al. Are TKAs performed in high-volume hospitals less likely to undergo revision than TKAs performed in low-volume hospitals? Clin Orthop Relat Res. 2017;475:2669–74.
Koltsov JCB, Marx RG, Bachner E, McLawhorn AS, Lyman S. Risk-based hospital and surgeon-volume categories for total hip arthroplasty. J Bone Joint Surg Am. 2018;100:1203–8.
Wilson S, Marx RG, Pan TJ, Lyman S. Meaningful thresholds for the volume-outcome relationship in total knee arthroplasty. J Bone Joint Surg Am. 2016;98:1683–90.
Kaplan GG, McCarthy EP, Ayanian JZ, Korzenik J, Hodin R, Sands BE. Impact of hospital volume on postoperative morbidity and mortality following a colectomy for ulcerative colitis. Gastroenterology. 2008;134:680–7.
Lee KJ, Kim JY, Kang J, et al. Hospital volume and mortality in acute ischemic stroke patients: effect of adjustment for stroke severity. J Stroke Cerebrovasc Dis. 2020;29:104753.
Huguet M, Joutard X, Ray-Coquard I, Perrier L. What underlies the observed hospital volume-outcome relationship? BMC Health Serv Res. 2022;22:70.
Hellinger F. Practice makes perfect: a volume-outcome study of hospital patients with HIV disease. J Acquir Immune Defic Syndr. 2008;47:226–33.
Gandjour A, Lauterbach KW. The practice-makes-perfect hypothesis in the context of other production concepts in health care. Am J Med Qual. 2003;18:171–5.
Kahn JM, Ten Have TR, Iwashyna TJ. The relationship between hospital volume and mortality in mechanical ventilation: an instrumental variable analysis. Health Serv Res. 2009;44:862–79.
Nguyen YL, Wallace DJ, Yordanov Y, et al. The volume-outcome relationship in critical care: a systematic review and meta-analysis. Chest. 2015;148:79–92.
Sadeghi M, Eshraghi M, Akers KG, et al. Outcomes of status epilepticus and their predictors in the elderly-A systematic review. Seizure. 2020;81:210–21.
Marawar R, Basha M, Mahulikar A, Desai A, Suchdev K, Shah A. Updates in Refractory Status Epilepticus. Crit Care Res Pract. 2018;20:9768949.
Goulden R, Whitehouse T, Murphy N, et al. Association between hospital volume and mortality in status epilepticus: a national cohort study. Crit Care Med. 2018;46:1969–76.
Jette N, Reid AY, Quan H, Hill MD, Wiebe S. How accurate is ICD coding for epilepsy? Epilepsia. 2010;51:62–9.
Gainza-Lein M, Fernandez IS, Ulate-Campos A, Loddenkemper T, Ostendorf AP. Timing in the treatment of status epilepticus: From basics to the clinic. Seizure. 2019;68:22–30.
Funding
This work received no funding.
Author information
Authors and Affiliations
Contributions
MJS MBBS: concept, data acquisition, data analysis, article writing, and article review. DZ MD: concept, article writing, and article review. AK MD: concept, data acquisition, data analysis, article writing, and article review. MMB MD: concept, article writing, and article review. RM MD: concept, data acquisition, data analysis, article writing, and article review. The final manuscript was approved by all authors.
Corresponding author
Ethics declarations
Conflicts of interest
Maysaa Basha and Rohit Marawar have received funds for Investigator-Initiated studies from Eisai Co Ltd. Maryam J. Syed, Deepti Zutshi, and Ayaz Khawaja declare that they have no conflict of interest.
Ethical Approval
All authors confirm that this article adheres to ethical guidelines.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Syed, M.J., Zutshi, D., Khawaja, A. et al. Understanding the Influence of Hospital Volume on Inpatient Outcomes Following Hospitalization for Status Epilepticus. Neurocrit Care 38, 26–34 (2023). https://doi.org/10.1007/s12028-022-01656-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-022-01656-3