Abstract
Background
Traumatic brain injury (TBI) induces complex systemic hemostatic alterations associated with secondary brain damage and death. We specifically investigated perioperative changes of hemostasis in patients with isolated TBI undergoing major neurosurgery and searched for their influence on outcome.
Methods
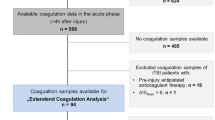
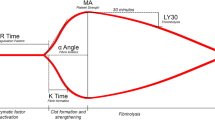
Serial analysis (four time points, T0–T3) of conventional coagulation assay and rotational thromboelastometry data acquired during 72 h from admission of 68 patients who underwent craniotomy to remove hematoma and/or to decompress the brain was performed. The primary outcome was in-hospital mortality. Secondary outcomes were the prevalence of hypocoagulation and increased clotting activity, coagulation parameters between survivors and nonsurvivors, and cutoff values of coagulation parameters predictive of mortality.
Results
Overall mortality was 22%. The prevalence of hypocoagulation according to rotational thromboelastometry decreased from 35.8% (T0) to 15.9% (T3). Lower fibrinogen levels, hyperfibrinolysis and fibrinolysis shutdown in the early period (T0–T1) following TBI were associated with higher mortality. Optimal cutoff values were identified: fibrin polymerization thromboelastometry (FIBTEM) clot amplitude at 10 min after clotting time ≤ 13 mm at T0 and FIBTEM clot amplitude at 10 min after clotting time ≤ 16.5 mm at T1 increased the odds of death by 6.0 (95% confidence interval [CI] 1.54–23.13, p = 0.010) and 9.7 (95% CI 2.06–45.36, p = 0.004), respectively. FIBTEM maximum clot firmness ≤ 14.5 mm at T0 and FIBTEM maximum clot firmness ≤ 18.5 mm at T1 increased the odds of death by 6.3 (95% CI 1.56–25.69, p = 0.010) and 9.1 (95% CI 1.88–44.39, p = 0.006). Fibrinogen < 3 g/L on postoperative day 1 (T1) was associated with a 9.5-fold increase of in-hospital mortality (95% CI 1.72–52.98, p = 0.01). Increased clotting activity was not associated with mortality.
Conclusions
Rotational thromboelastometry adds important information for identifying patients with TBI at increased risk of death. Early fibrinogen-related coagulation disorders are associated with mortality of patients with TBI undergoing major neurosurgical procedures. Maintenance of higher fibrinogen levels might be necessary for neurosurgical patients with acute TBI.







Similar content being viewed by others
References
Maegele M, Aversa J, Marsee MK, et al. Changes in coagulation following brain injury. Semin Thromb Hemost. 2020;46:155–66.
Laroche M, Kutcher ME, Huang MC, Cohen MJ, Manley GT. Coagulopathy after traumatic brain injury. Neurosurgery. 2012;70:1334–45.
Maegele M, Schöchl H, Menovsky T, et al. Coagulopathy and haemorrhagic progression in traumatic brain injury: advances in mechanisms, diagnosis, and management. Lancet Neurol. 2017;16:630.
Lustenberger T, Talving P, Kobayashi L, et al. Time course of coagulopathy in isolated severe traumatic brain injury. Injury. 2010;41:924–8.
Harhangi BS, Kompanje E, Leebeek F, Maas A. Coagulation disorders after traumatic brain injury. Acta Neurochir (Wien). 2008;150:165–75.
Epstein DS, Mitra B, Cameron PA, Fitzgerald M, Rosenfeld JV. Acute traumatic coagulopathy in the setting of isolated traumatic brain injury: Definition, incidence and outcomes. Br J Neurosurg. 2015;29:118.
Wafaisade A, Lefering R, Tjardes T, et al. Acute Coagulopathy in Isolated Blunt Traumatic Brain Injury. Neurocrit Care. 2010;12:211–9.
Görlinger K, Dirkmann D, Hanke AA. Rotational Thromboelastometry (ROTEM®). In: Gonzales E, Moore HB, Moore EE, editors. Trauma Induced Coagulopathy. Switzerland: Springer International Publishing; 2016. p. 267.
Wikkelsø A, Wetterslev J, Møller AM, Afshari A. Thromboelastography (TEG) or thromboelastometry (ROTEM) to monitor haemostatic treatment versus usual care in adults or children with bleeding. Cochrane Database Syst Rev. 2016;2016:CD007871.
Kvint S, Schuster J, Kumar MA. Neurosurgical applications of viscoelastic hemostatic assays. Neurosurg Focus. 2017;43:E9.
Shammassian BH, Ronald A, Smith A, Sajatovic M, Mangat HS, Kelly ML. Viscoelastic hemostatic assays and outcomes in traumatic brain injury: a systematic literature review. World Neurosurg. 2022;159(221):236.e4.
Gennarelli TA, Wodzin E. AIS 2005: a contemporary injury scale. Injury. 2006;37:1083–91.
Carney N, Totten AM, O’Reilly C, et al. Guidelines for the management of severe traumatic brain injury. Fourth Edition Neurosurgery. 2017;80:6–15.
Dimitrova-Karamfilova A, Patokova Y, Solarova T, Petrova I, Natchev G. Rotation thromboelastography for assessment of hypercoagulation and thrombosis in patients with cardiovascular diseases. J Life Sci. 2012;6:28–35.
Gomez-Builes JC, Acuna SA, Nascimento B, Madotto F, Rizoli SB. Harmful or physiologic: diagnosing fibrinolysis shutdown in a trauma cohort with rotational thromboelastometry. Anesth Analg. 2018;127:840–9.
Posti JP, Luoto TM, Rautava P, Kytö V. Mortality after trauma craniotomy is decreasing in older adults-a nationwide population-based study. World Neurosurg. 2021;152:e313–20.
Schöchl H, Solomon C, Traintinger S, et al. Thromboelastometric (ROTEM) findings in patients suffering from isolated severe traumatic brain injury. J Neurotrauma. 2011;28:2033–41.
Windeløv NA, Welling KL, Ostrowski SR, Johansson PI. The prognostic value of thrombelastography in identifying neurosurgical patients with worse prognosis. Blood Coagul Fibrinolysis. 2011;22:416–9.
Epstein DS, Mitra B, O’Reilly G, Rosenfeld JV, Cameron PA. Acute traumatic coagulopathy in the setting of isolated traumatic brain injury: A systematic review and meta-analysis. Injury. 2014;45:819–24.
Beynon C, Unterberg AW, Sakowitz OW. Point of care coagulation testing in neurosurgery. J Clin Neurosci. 2015;22:252–7.
Kunio NR, Differding JA, Watson KM, Stucke RS, Schreiber MA. Thrombelastography-identified coagulopathy is associated with increased morbidity and mortality after traumatic brain injury. Am J Surg. 2012;203:584–8.
Cannon JW, Dias JD, Kumar MA, et al. Use of thromboelastography in the evaluation and management of patients with traumatic brain injury: a systematic review and meta-analysis. Crit Care Explor. 2021;3: e0526.
Rao A, Lin A, Hilliard C, et al. The utility of thromboelastography for predicting the risk of progression of intracranial hemorrhage in traumatic brain injury patients. Neurosurgery. 2017;64:182–7.
Kozek-Langenecker SA, Ahmed AB, Afshari A, et al. Management of severe perioperative bleeding: guidelines from the European Society of Anaesthesiology: First update 2016. Eur J Anaesthesiol. 2017;34:332–95.
CRASH-3 trial collaborators. Effects of tranexamic acid on death, disability, vascular occlusive events and other morbidities in patients with acute traumatic brain injury (CRASH-3): a randomised, placebo-controlled trial. Lancet 2019;394:1713–23.
Massaro AM, Doerfler S, Nawalinski K, et al. Thromboelastography defines late hypercoagulability after TBI: a pilot study. Neurocrit Care. 2015;22:45–51.
Kupcinskiene K, Trepenaitis D, Petereit R, et al. Monitoring of hypercoagulability by thromboelastography in bariatric surgery. Med Sci Monit. 2017;23:1819–26.
Müller MC, Balvers K, Binnekade JM, et al. Thromboelastometry and organ failure in trauma patients: a prospective cohort study. Crit Care. 2014;18:687–96.
Funding
None.
Author information
Authors and Affiliations
Contributions
MR participated in study organization, data collection, statistical analysis, and article preparation. VC participated in statistical analysis and article preparation. DB participated in study organization, data collection and performed critical review of the article. NB participated in data collection, consulted regarding neurointensive care issues, and performed critical review of the article. RV participated in data collection, consulted regarding neurosurgical issues, and performed critical review of the article. KR consulted regarding data analysis and article preparation, and performed critical review of the article. AM participated in study organization, critical data analysis and article preparation. The final manuscript was approved by all authors.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethical Approval/Informed Consent
The authors confirm adherence to ethical guidelines. Ethical approval was provided by the Regional Ethics Committee of Biomedical Research (number: BE-2–17). Written consent was obtained from all participants or their responsible parties before any analysis of the available data.
Clinical trial registration
Clinicaltrials.gov: NCT03616808.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rimaitis, M., Cechanovičiūtė, V., Bilskienė, D. et al. Dynamic Changes of Hemostasis in Patients with Traumatic Brain Injury Undergoing Craniotomy: Association with in-Hospital Mortality. Neurocrit Care 38, 714–725 (2023). https://doi.org/10.1007/s12028-022-01639-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-022-01639-4