Abstract
Background
Early neurological deterioration (END) after endovascular thrombectomy (EVT) is strongly associated with poor prognosis in patients with large vessel occlusion. The relationship between body temperature and END after EVT is unknown, which we aimed to investigate in this study.
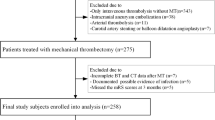
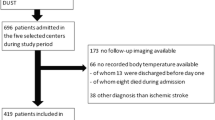
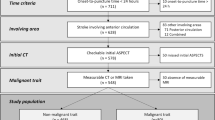
Methods
END was defined as an increase of four or more points on the National Institutes of Health Stroke Scale score compared with the baseline assessment within 24 h. Logistic regression and restricted cubic spline models were used to assess the relationship between body temperature and END.
Results
Among 7741 consecutive patients with ischemic stroke, 406 patients with large vessel occlusion who underwent EVT were enrolled. In total, 88 (21.7%) patients developed END. Logistic regression showed that the maximum body temperature within 24 h (odds ratio [OR] = 1.97 per °C, 95% confidence interval [CI] 1.17–3.32, p = 0.010) was independently associated with END. This association was nonlinear and J shaped (p for nonlinearity = 0.010), and the risk of END increased when the maximum body temperature within 24 h was lower or higher than 37.0 °C. Fever burden is also independently associated with END (OR = 1.06 per °C × hour, 95% CI 1.01–1.11, p = 0.012). In addition, the timing of fever onset was independently associated with END, and the highest risk of END was associated with fever onset within 6 h after EVT (OR = 3.92, 95% CI 1.25–12.27, p = 0.019).
Conclusions
In summary, there is a J-shaped association between the maximum body temperature within 24 h after EVT and END. Moreover, the risk of END differed according to the timing of fever onset.




Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author on reasonable request.
Change history
05 March 2022
A Correction to this paper has been published: https://doi.org/10.1007/s12028-022-01451-0
References
Campbell BCV, Khatri P. Stroke. Lancet (London, England). 2020;396(10244):129–42. https://doi.org/10.1016/s0140-6736(20)31179-x.
Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387(10029):1723–31. https://doi.org/10.1016/s0140-6736(16)00163-x.
Kim JM, Bae JH, Park KY, et al. Incidence and mechanism of early neurological deterioration after endovascular thrombectomy. J Neurol. 2019;266(3):609–15. https://doi.org/10.1007/s00415-018-09173-0.
Zhang YB, Su YY, He YB, Liu YF, Liu G, Fan LL. Early neurological deterioration after recanalization treatment in patients with acute ischemic stroke: a retrospective study. Chin Med J (Engl). 2018;131(2):137–43. https://doi.org/10.4103/0366-6999.222343.
Seners P, Turc G, Oppenheim C, Baron JC. Incidence, causes and predictors of neurological deterioration occurring within 24 h following acute ischaemic stroke: a systematic review with pathophysiological implications. J Neurol Neurosurg Psychiatry. 2015;86(1):87–94. https://doi.org/10.1136/jnnp-2014-308327.
Irvine HJ, Battey TW, Ostwaldt AC, et al. Early neurological stability predicts adverse outcome after acute ischemic stroke. Int J Stroke. 2016;11(8):882–9. https://doi.org/10.1177/1747493016654484.
Dávalos A, Castillo J, Pumar JM, Noya M. Body temperature and fibrinogen are related to early neurological deterioration in acute ischemic stroke. Cerebrovasc Dis. 1997;7(2):64–9.
Meden P, Overgaard K, Pedersen H, Boysen G. The influence of body temperature on infarct volume and thrombolytic therapy in a rat embolic stroke model. Brain Res. 1994;647(1):138.
Dehkharghani S, Bowen M, Haussen DC, et al. Body temperature modulates infarction growth following endovascular reperfusion. AJNR Am J Neuroradiol. 2017;38(1):46–51. https://doi.org/10.3174/ajnr.A4969.
van der Worp HB, Sena ES, Donnan GA, Howells DW, Macleod MR. Hypothermia in animal models of acute ischaemic stroke: a systematic review and meta-analysis. Brain. 2007;130(Pt 12):3063–74. https://doi.org/10.1093/brain/awm083.
Powers WJ, Derdeyn CP, Biller J, et al. 2015 American Heart Association/American Stroke Association Focused Update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46(10):3020–35. https://doi.org/10.1161/str.0000000000000074.
Liu L, Chen W, Zhou H, et al. Chinese Stroke Association guidelines for clinical management of cerebrovascular disorders: executive summary and 2019 update of clinical management of ischaemic cerebrovascular diseases. Stroke Vasc Neurol. 2020;5(2):159–176. https://doi.org/10.1136/svn-2020-000378.
Waqas M, Rai AT, Vakharia K, Chin F, Siddiqui AH. Effect of definition and methods on estimates of prevalence of large vessel occlusion in acute ischemic stroke: a systematic review and meta-analysis. J Neurointerv Surg. 2020;12(3):260–5. https://doi.org/10.1136/neurintsurg-2019-015172.
Barber PA, Demchuk AM, Zhang J, Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score. Lancet (London, England) 2000;355(9216):1670–4. https://doi.org/10.1016/s0140-6736(00)02237-6
Brott T, Adams HP Jr, Olinger CP, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989;20(7):864–70. https://doi.org/10.1161/01.str.20.7.864.
Adams HP, Jr., Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in acute stroke treatment. Stroke 1993;24(1):35–41. https://doi.org/10.1161/01.str.24.1.35
Suh SH, Cloft HJ, Fugate JE, Rabinstein AA, Liebeskind DS, Kallmes DF. Clarifying differences among thrombolysis in cerebral infarction scale variants: is the artery half open or half closed? Stroke. 2013;44(4):1166–8. https://doi.org/10.1161/strokeaha.111.000399.
Smith CJ, Kishore AK, Vail A, et al. Diagnosis of stroke-associated pneumonia: recommendations from the pneumonia in stroke consensus group. Stroke. 2015;46(8):2335–40. https://doi.org/10.1161/STROKEAHA.115.009617.
Boehme AK, Kumar AD, Dorsey AM, et al. Infections present on admission compared with hospital-acquired infections in acute ischemic stroke patients. J Stroke Cerebrovasc Dis. 2013;22(8):e582–9. https://doi.org/10.1016/j.jstrokecerebrovasdis.2013.07.020
Friedant AJ, Gouse BM, Boehme AK, et al. A simple prediction score for developing a hospital-acquired infection after acute ischemic stroke. J Stroke Cerebrovasc Dis. 2015;24(3):680–6. https://doi.org/10.1016/j.jstrokecerebrovasdis.2014.11.014.
Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis. 2008;25(5):457–507. https://doi.org/10.1159/000131083.
Phipps MS, Desai RA, Wira C, Bravata DM. Epidemiology and outcomes of fever burden among patients with acute ischemic stroke. Stroke. 2011;42(12):3357–62. https://doi.org/10.1161/strokeaha.111.621425.
Petersen NH, Ortega-Gutierrez S, Wang A, et al. Decreases in blood pressure during thrombectomy are associated with larger infarct volumes and worse functional outcome. Stroke. 2019;50(7):1797–804. https://doi.org/10.1161/strokeaha.118.024286.
Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8(5):551–61. https://doi.org/10.1002/sim.4780080504.
Groenwold RH, Donders AR, Roes KC, Harrell FE Jr, Moons KG. Dealing with missing outcome data in randomized trials and observational studies. Am J Epidemiol. 2012;175(3):210–7. https://doi.org/10.1093/aje/kwr302.
Tiainen M, Meretoja A, Strbian D, et al. Body temperature, blood infection parameters, and outcome of thrombolysis-treated ischemic stroke patients. Int J Stroke. 2013;8(8):632–8. https://doi.org/10.1111/ijs.12039.
Diprose WK, Liem B, Wang MTM, et al. Impact of body temperature before and after endovascular thrombectomy for large vessel occlusion stroke. Stroke. 2020;51(4):1218–25. https://doi.org/10.1161/STROKEAHA.119.028160.
Li Z, Zhang H, Han J, et al. Time course and clinical relevance of neurological deterioration after endovascular recanalization therapy for anterior circulation large vessel occlusion stroke. Front Aging Neurosci. 2021;13:651614. https://doi.org/10.3389/fnagi.2021.651614.
Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46–110. https://doi.org/10.1161/str.0000000000000158.
Saxena M, Young P, Pilcher D, et al. Early temperature and mortality in critically ill patients with acute neurological diseases: trauma and stroke differ from infection. Intensive Care Med. 2015;41(5):823–32. https://doi.org/10.1007/s00134-015-3676-6.
Campos F, Blanco M, Barral D, Agulla J, Ramos-Cabrer P, Castillo J. Influence of temperature on ischemic brain: basic and clinical principles. Neurochem Int. 2012;60(5):495–505. https://doi.org/10.1016/j.neuint.2012.02.003.
Castillo J, Dávalos A, Marrugat J, Noya M. Timing for fever-related brain damage in acute ischemic stroke. Stroke. 1998;29(12):2455–60. https://doi.org/10.1161/01.str.29.12.2455.
Kim SH, Saver JL. Initial body temperature in ischemic stroke: nonpotentiation of tissue-type plasminogen activator benefit and inverse association with severity. Stroke. 2015;46(1):132–6. https://doi.org/10.1161/STROKEAHA.114.006107.
Acknowledgement
We thank Professor Cairong Zhu from the School of Public Health SCU, who kindly assisted with the design of the statistical method for our analysis.
Funding
This work was supported by the National Key Research and Development Program of China (Nos. 2018YFC1311400, 2018YFC1311401), the National Natural Science Foundation of China (Grant No. 81772435), the Science & Technology Department of Sichuan Province (No. 2020YFS0155), and West China Nursing Discipline Special Fund Project, Sichuan University (HXHL20021).
Author information
Authors and Affiliations
Contributions
Study conception and design: LH, YL, and MC. Data acquisition: YL, MC, JB, LF. Data analysis and interpretation: YL, MC, SD, JB. Statistical analysis: YL, SD. Article draft: YL, JF, SD, MM. Critical revision of the manuscript for important intellectual content: LH, LF, YL, MC, JF, SD, MM, JB. Approved the submitted version: LH, LF, YL, MC, JF, SD, MM, JB.
Corresponding authors
Ethics declarations
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval/informed consent
The authors confirm adherence to ethical guidelines and indicate ethical approvals (institutional review board). This study was performed in accordance with ethics principles of the 1964 Declaration of Helsinki and its later amendments and approved by the Ethics Committee of West China Hospital. The need to obtain informed consent was waived because of the retrospective and observational nature of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article was updated to correct the equal contribution note.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Luo, Y., Chen, M., Fang, J. et al. Relationship Between Body Temperature and Early Neurological Deterioration after Endovascular Thrombectomy for Acute Ischemic Stroke with Large Vessel Occlusion. Neurocrit Care 37, 399–409 (2022). https://doi.org/10.1007/s12028-021-01416-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-021-01416-9