Abstract
Background
Patients with aneurysmal subarachnoid hemorrhage (aSAH) may develop refractory arterial cerebral vasospasm requiring multiple endovascular interventions. The aim of our study is to evaluate variables associated with need for repeat endovascular treatments in refractory vasospasm and to identify differences in outcomes following one versus multiple treatments.
Methods
We retrospectively reviewed patients treated for aSAH between 2017 and 2020 at two tertiary care centers. We included patients who underwent treatment (intraarterial infusion of vasodilatory agents or mechanical angioplasty) for radiographically diagnosed vasospasm in our analysis. Patients were divided into those who underwent single treatment versus those who underwent multiple endovascular treatments for vasospasm.
Results
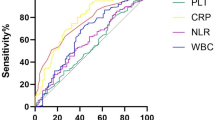
Of the total 418 patients with aSAH, 151 (45.9%) underwent endovascular intervention for vasospasm. Of 151 patients, 95 (62.9%) underwent a single treatment and 56 (37.1%) underwent two or more treatments. Patients were more likely to undergo multiple endovascular treatments if they had a Hunt–Hess score > 2 (odds ratio [OR] 5.10 [95% confidence interval (CI) 1.82–15.84]; p = 0.003), a neutrophil-to-lymphocyte ratio > 8.0 (OR 3.19 [95% CI 1.40–7.62]; p = 0.028), and more than two fevers within the first 5 days of admission (OR 7.03 [95% CI 2.68–20.94]; p < 0.001). Patients with multiple treatments had poorer outcomes, including increased length of stay, delayed cerebral ischemia, in-hospital complications, and higher modified Rankin scores at discharge.
Conclusions
A Hunt–Hess score > 2, a neutrophil-to-lymphocyte ratio > 8.0, and early fevers may be predictive of need for multiple endovascular interventions in refractory cerebral vasospasm after aSAH. These patients have poorer functional outcomes at discharge and higher rates of in-hospital complications.


Similar content being viewed by others
Data availability
Data pertaining to this study are available on reasonable request to the corresponding author.
References
van Gijn J, Rinkel GJ. Subarachnoid haemorrhage: diagnosis, causes and management. Brain. 2001;124:249–78.
Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. N Engl J Med. 2006;354:387–96.
Connolly ES, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2012;43:1711–37.
Geraghty JR, Lara-Angulo MN, Spegar M, Reeh J, Testai FD. Severe cognitive impairment in aneurysmal subarachnoid hemorrhage: Predictors and relationship to functional outcome. J Stroke Cerebrovasc Dis. 2020;29:105027.
Rabinstein AA, Pichelmann MA, Friedman JA, Piepgras DG, Nichols DA, McIver JI, et al. Symptomatic vasospasm and outcomes following aneurysmal subarachnoid hemorrhage: a comparison between surgical repair and endovascular coil occlusion. J Neurosurg. 2003;98:319–25.
Pickard JD, Murray GD, Illingworth R, Shaw MD, Teasdale GM, Foy PM, et al. Effect of oral nimodipine on cerebral infarction and outcome after subarachnoid haemorrhage: British aneurysm nimodipine trial. BMJ. 1989;298:636–42.
Andereggen L, Beck J, Z’Graggen WJ, Schroth G, Andres RH, Murek M, et al. Feasibility and safety of repeat instant endovascular interventions in patients with refractory cerebral vasospasms. AJNR Am J Neuroradiol. 2017;38:561–7.
Chang JJ, Triano M, Corbin MJ, Desale S, Liu A-H, Felbaum DR, et al. Transcranial Doppler velocity and associations with delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage. J Neurol Sci. 2020;415:116934.
Findlay JM, Nisar J, Darsaut T. Cerebral vasospasm: a review. Can J Neurol Sci. 2016;43:15–32.
Park E-S, Kim D-W, Kang S-D. Endovascular treatment of symptomatic vasospasm after aneurysmal subarachnoid hemorrhage: a three-year experience. J Cerebrovasc Endovasc Neurosurg. 2017;19:155–61.
Neumann A, Ditz C, Schacht H, Aulmann L, Tronnier VM, Schramm P, et al. Symptomatic cerebral vasospasm after spontaneous subarachnoid hemorrhage: comparison of single and multiple intra-arterial treatment with respect to the functional outcome. J Neurol Surg A Cent Eur Neurosurg. 2020;81:220–6.
Mortimer AM, Steinfort B, Faulder K, Erho T, Dexter M, Assaad N, et al. Institution of sustained endovascular treatment prior to clinical deterioration in patients with severe angiographic vasospasm: a retrospective observational study of clinico-radiological outcomes. J Neuroradiol. 2015;42:176–83.
Jun P, Ko NU, English JD, Dowd CF, Halbach VV, Higashida RT, et al. Endovascular treatment of medically refractory cerebral vasospasm following aneurysmal subarachnoid hemorrhage. AJNR Am J Neuroradiol. 2010;31:1911–6.
Andaluz N, Tomsick TA, Tew JM, van Loveren HR, Yeh H-S, Zuccarello M. Indications for endovascular therapy for refractory vasospasm after aneurysmal subarachnoid hemorrhage: experience at the University of Cincinnati. Surg Neurol. 2002;58:131–8 (discussion 138).
Hockel K, Diedler J, Steiner J, Birkenhauer U, Danz S, Ernemann U, et al. Long-term, continuous intra-arterial nimodipine treatment of severe vasospasm after aneurysmal subarachnoid hemorrhage. World Neurosurg. 2016;88:104–12.
Kieninger M, Flessa J, Lindenberg N, Bele S, Redel A, Schneiker A, et al. Side effects of long-term continuous intra-arterial nimodipine infusion in patients with severe refractory cerebral vasospasm after subarachnoid hemorrhage. Neurocrit Care. 2018;28:65–76.
Scaravilli V, Tinchero G, Citerio G. Participants in the international multi-disciplinary consensus conference on the critical care management of subarachnoid hemorrhage. Fever management in SAH. Neurocrit Care. 2011;15:287–94.
Park YK, Yi H-J, Choi K-S, Lee Y-J, Chun H-J, Kwon SM. Predictive factors of fever after aneurysmal subarachnoid hemorrhage and its impact on delayed cerebral ischemia and clinical outcomes. World Neurosurg. 2018;114:e524–31.
Lai PMR, See AP, Silva MA, Gormley WB, Frerichs KU, Aziz-Sultan MA, et al. Noninfectious fever in aneurysmal subarachnoid hemorrhage: association with cerebral vasospasm and clinical outcome. World Neurosurg. 2019;122:e1014–9.
Saripalli M, Tan D, Chandra RV, Lai LT. Predictive relevance of early temperature elevation on the risk of delayed cerebral ischemia development following aneurysmal subarachnoid hemorrhage. World Neurosurg. 2021;150:e474–81.
Fernandez A, Schmidt JM, Claassen J, Pavlicova M, Huddleston D, Kreiter KT, et al. Fever after subarachnoid hemorrhage: risk factors and impact on outcome. Neurology. 2007;68:1013–9.
Tam AKH, Ilodigwe D, Mocco J, Mayer S, Kassell N, Ruefenacht D, et al. Impact of systemic inflammatory response syndrome on vasospasm, cerebral infarction, and outcome after subarachnoid hemorrhage: exploratory analysis of CONSCIOUS-1 database. Neurocrit Care. 2010;13:182–9.
Carhuapoma JR, Gupta K, Coplin WM, Muddassir SM, Meratee MM. Treatment of refractory fever in the neurosciences critical care unit using a novel, water-circulating cooling device. A single-center pilot experience. J Neurosurg Anesthesiol. 2003;15:313–8.
Niven DJ, Gaudet JE, Laupland KB, Mrklas KJ, Roberts DJ, Stelfox HT. Accuracy of peripheral thermometers for estimating temperature: a systematic review and meta-analysis. Ann Intern Med. 2015;163:768–77.
Weng W-J, Yang C, Huang X-J, Zhang Y-M, Liu J-F, Yao J-M, et al. Effects of brain temperature on the outcome of patients with traumatic brain injury: a prospective observational study. J Neurotrauma. 2019;36:1168–74.
Provencio JJ, Fu X, Siu A, Rasmussen PA, Hazen SL, Ransohoff RM. CSF neutrophils are implicated in the development of vasospasm in subarachnoid hemorrhage. Neurocrit Care. 2010;12:244–51.
Al-Mufti F, Amuluru K, Damodara N, Dodson V, Roh D, Agarwal S, et al. Admission neutrophil-lymphocyte ratio predicts delayed cerebral ischemia following aneurysmal subarachnoid hemorrhage. J Neurointerv Surg. 2019;11:1135–40.
Giede-Jeppe A, Reichl J, Sprügel MI, Lücking H, Hoelter P, Eyüpoglu IY, et al. Neutrophil-to-lymphocyte ratio as an independent predictor for unfavorable functional outcome in aneurysmal subarachnoid hemorrhage. J Neurosurg. 2019;132:400–7.
Chang JJ, Dowlati E, Triano M, Kalegha E, Krishnan R, Kasturiarachi BM, et al. Admission neutrophil to lymphocyte ratio for predicting outcome in subarachnoid hemorrhage. J Stroke Cerebrovasc Dis. 2021;30:105936.
Lattanzi S, Cagnetti C, Rinaldi C, Angelocola S, Provinciali L, Silvestrini M. Neutrophil-to-lymphocyte ratio improves outcome prediction of acute intracerebral hemorrhage. J Neurol Sci. 2018;387:98–102.
Świtońska M, Piekuś-Słomka N, Słomka A, Sokal P, Żekanowska E, Lattanzi S. Neutrophil-to-lymphocyte ratio and symptomatic hemorrhagic transformation in ischemic stroke patients undergoing revascularization. Brain Sci. 2020;10:E771.
Jackson CM, Choi J, Routkevitch D, Pant A, Saleh L, Ye X, et al. PD-1+ monocytes mediate cerebral vasospasm following subarachnoid hemorrhage. Neurosurgery. 2021;88:855–63.
Feghali J, Kim J, Gami A, Rapaport S, Caplan JM, McDougall CG, et al. Monocyte-based inflammatory indices predict outcomes following aneurysmal subarachnoid hemorrhage. Neurosurg Rev. 2021;44:3499–507.
Fan BB, Sun XC, Huang ZJ, Yang XM, Guo ZD, He ZH. Hypoperfusion assessed by pressure reactivity index is associated with delayed cerebral ischemia after subarachnoid hemorrhage: an observational study. Chin Neurosurg J. 2021;7:16.
Funding
None.
Author information
Authors and Affiliations
Contributions
ED and WM contributed equally to this article. Study design: ED, WM, JJC, RAA. Data acquisition: ED, WM, AC, JJC. Data analysis and interpretation: ED, WM, SS, DRF, JCM, AHL, RAA. Manuscript preparation: ED, WM, AC, JJC. Revision of manuscript for important intellectual content: JCM, DRF, SS, JJC, AHL, RAA. Approval of the final version of the manuscript: all authors.
Corresponding author
Ethics declarations
Conflicts of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements) or nonfinancial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this article.
Ethical approval/informed consent
The authors confirm adherence to ethical guidelines, and ethical approvals were used of informed consent, as appropriate. This study was approved by the Institutional Review Board at Georgetown University (IRB Approval STUDY00003977).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dowlati, E., Mualem, W., Carpenter, A. et al. Early Fevers and Elevated Neutrophil-to-Lymphocyte Ratio are Associated with Repeat Endovascular Interventions for Cerebral Vasospasm in Patients with Aneurysmal Subarachnoid Hemorrhage. Neurocrit Care 36, 916–926 (2022). https://doi.org/10.1007/s12028-021-01399-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-021-01399-7