Abstract
Background
Helicopter medical transportation (HMT) is a valuable resource that can expedite medical care by shortening transferring times. However, there is conflicting evidence regarding its cost and efficacy. No specific studies have addressed its use in patients transferred to the neuroscience intensive care unit (NSICU).
Methods
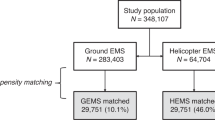
This was a retrospective study performed at a university hospital in the coastal southeastern USA. The flight logs for the air ambulance company were reviewed, and all patients undergoing HMT to the NSICU during a 1-year period were identified. Flight logs and medical records were reviewed to obtain basic demographics, diagnosis, mortality, transportation distance, and performance of time-sensitive interventions (TSIs) to include ventriculostomy placement, emergency craniotomy, emergency craniectomy, emergency aneurysm obliteration, emergency spine surgery, emergent endovascular procedures, subdural drain placement, emergent shunt revision, and continuous electroencephalography (EEG) performed within 4 h of admission. We analyzed the cost of HMT and correlated the clinical variables with the performance of TSIs.
Results
A total of 101 patients underwent HMT during a 12-month period; 26 underwent 30 TSIs (4 underwent 2 TSIs) and an additional 4 were transported for EEG monitoring. The only clinical variable associated with a TSI was subarachnoid hemorrhage with ventriculostomy placement. Continuous EEG monitoring performed in four patients with suspected status epilepticus did not show status epilepticus in any of them (one was performed after 4 h). Transportation distance was less than 60 miles in four patients who underwent TSIs. The total cost of HMT was $3,360,573: $842,672 for those who underwent TSIs and $2,517,901 for those who did not. When compared with ground transportation, an excess cost of $3,129,415.25 was incurred by using HMT. There was no difference in the median cost of transportation between patients who underwent TSIs and those who did not ($30,210 vs. $30,211). The median cost transportation difference between HMT and ground transportation was significantly different (p < 0.001), with a median excess cost of $28,023 (range $15,553–76,155) per patient.
Conclusions
The majority of patients who were transferred via HMT did not undergo TSIs, and among those who underwent TSIs, approximately one in six was transported from a hospital located less than 60 miles away from the NSICU; the distances of ground and air transportation are equivalent. Helicopter transfers may play a role in subarachnoid hemorrhage management. A significant expense was incurred by using HMT for the majority of patients (75%) who did not undergo TSIs.

Similar content being viewed by others
References
Floccare DJ, Stuhlmiller DF, Braithwaite SA, Thomas SH, Madden JF, Hankins DG, et al. Appropriate and safe utilization of helicopter emergency medical services: a joint position statement with resource document. Prehosp Emerg Care. 2013;17(4):521–5.
Svenson JE, O’Connor JE, Lindsay MB. Is air transport faster? A comparison of air versus ground transport times for interfacility transfer in a regional referral system. Air Med J. 2006;25(4):170–2.
Walcott BP, Coumans JV, Mian MK, Nahed BV, Kahle KT. Interfacility helicopter ambulance transport of neurosurgical patients: observations, utilization, and outcomes from a quaternary level care hospital. PLoS ONE. 2011;6(10):e26216.
Delgado MK, Staudenmayer KL, Wang NE, Spain DA, Weir S, Owens DK, et al. Cost-effectiveness of helicopter versus ground emergency medical services for trauma scene transport in the United States. Ann Emerg Med. 2013;62(4):351–64.
Hesselfeldt R, Gyllenborg J, Steinmetz J, Quoc Do H, Hejselbæk J, Rasmussen LS. Is air transport of stroke patients faster than ground transport? A prospective controlled observational study. Emerg Med J. 2014;31:268–72.
Melton JTK, Jain S, Kendrick B. A helicopter emergency ambulance service (HEAS) transfer: an analysis of trauma patient case-mix, injury severity and outcome. R Coll Surg Engl. 2007;89:513–6.
Black JJM, Ward ME, Lockey DJ. Appropriate use of helicopters to transport trauma patients from incident scene to hospital in the United Kingdom: an algorithm. Emerg Med J. 2004;21:355–61.
Regenhardt RW, Mecca AP, Flavin SA, Boulouis G, Lauer A, Zachrison KS, et al. Delays in the air or ground transfer of patients for endovascular thrombectomy. Stroke. 2018;49(6):1419–25.
Owen JL, Phillips RT, Conaway C, et al. One year’s trauma mortality experience at Brooke Army Medical Center: is aeromedical transportation of trauma patients necessary? Mil Med. 1999;164:361–5.
Samuels O, Webb A, Culler S, Martin K, Barrow D. Impact of a dedicated neurocritical care team in treating patients with aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2011;14:334–40.
Diaz MA, Hendey GW, Bivins HG. When is the helicopter faster? A comparison of helicopter and ground ambulance transport times. J Trauma. 2005;58:148–53.
Chen X, Gestring ML, Rosengart MR, Billiar TR, Peitzman AB, Sperry JL, et al. Speed is not everything: identifying patients who may benefit from helicopter transport despite faster ground transport. J Trauma Acute Care Surg. 2018;84:549–57.
Kunte SA, Anderson D, Brown-Espaillat K, Froehler MT. Total transfer time for ground vs. air transport for interhospital and scene transfers of acute stroke patients. J Stroke Cerebrovasc Dis. 2021;30:11–7.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
Julio A. Chalela, Melissa Hill and Patrick E. Britell involved in study design, data collection, data analysis and manuscript preparation, and the final manuscript was approved by all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors do not have any conflicts of interest.
Ethical Approval/Informed Consent
We confirm adherence to ethical guidelines and indicate ethical approvals (institutional review board) and the use of informed consent, as appropriate. Retrospective studies require a statement regarding institutional review board approval.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chalela, J.A., Hill, M. & Britell, P.E. Use of Helicopter Medical Transportation to the Neuroscience Intensive Care Unit. Neurocrit Care 36, 797–801 (2022). https://doi.org/10.1007/s12028-021-01371-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-021-01371-5