Abstract
Background
Palliative care has the potential to improve goal-concordant care in severe traumatic brain injury (sTBI). Our primary objective was to illuminate the demographic profiles of patients with sTBI who receive palliative care encounters (PCEs), with an emphasis on the role of race. Secondary objectives were to analyze PCE usage over time and compare health care resource utilization between patients with or without PCEs.
Methods
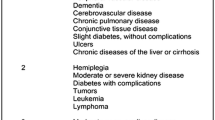
The National Inpatient Sample database was queried for patients age ≥ 18 who had a diagnosis of sTBI, defined by using International Classification of Diseases, 9th Revision codes. PCEs were defined by using International Classification of Diseases, 9th Revision code V66.7 and trended from 2001 to 2015. To assess factors associated with PCE in patients with sTBI, we performed unweighted generalized estimating equations regression. PCE association with decision making was modeled via its effect on rate of percutaneous endoscopic gastrostomy (PEG) tube placement. To quantify differences in PCE-related decisions by race, race was modeled as an effect modifier.
Results
From 2001 to 2015, the proportion of palliative care usage in patients with sTBI increased from 1.5 to 36.3%, with 41.6% White, 22.3% Black, and 25% Hispanic patients with sTBI having a palliative care consultation in 2015, respectively. From 2008 to 2015, we identified 17,673 sTBI admissions. White and affluent patients were more likely to have a PCE than Black, Hispanic, and low socioeconomic status patients. Across all races, patients receiving a PCE resulted in a lower rate of PEG tube placement; however, White patients exhibited a larger reduction of PEG tube placement than Black patients. Patients using palliative care had lower total hospital costs (median $16,368 vs. $26,442, respectively).
Conclusions
Palliative care usage for sTBI has increased dramatically this century and it reduces resource utilization. This is true across races, however, its usage rate and associated effect on decision making are race-dependent, with White patients receiving more PCE and being more likely to decline the use of a PEG tube if they have had a PCE.


Similar content being viewed by others
References
Cooper DJ, Myles PS, McDermott FT, et al. Prehospital hypertonic saline resuscitation of patients with hypotension and severe traumatic brain injury: a randomized controlled trial. JAMA. 2004;291(11):1350–7.
Brooks JC, Strauss DJ, Shavelle RM, Paculdo DR, Hammond FM, Harrison-Felix CL. Long-term disability and survival in traumatic brain injury: results from the National Institute on disability and rehabilitation research model systems. Arch Phys Med Rehabil. 2013;94(11):2203–9.
Giacino JT, Katz DI, Schiff ND, et al. Practice guideline update recommendations summary: disorders of consciousness: report of the guideline development, dissemination, and implementation subcommittee of the American academy of neurology; the American congress of rehabilitation medicine; and the national institute on disability, independent living, and rehabilitation research. Neurology. 2018;91(10):450–60.
van Dijck JTJM, Dijkman MD, Ophuis RH, de Ruiter GCW, Peul WC, Polinder S. In-hospital costs after severe traumatic brain injury: a systematic review and quality assessment. PLoS ONE. 2019;14(5):e0216743.
Lilley EJ, Scott JW, Weissman JS, et al. End-of-life care in older patients after serious or severe traumatic brain injury in low-mortality hospitals compared with all other hospitals. JAMA Surg. 2018;153(1):44–50.
Mosenthal AC, Murphy PA, Barker LK, Lavery R, Retano A, Livingston DH. Changing the culture around end-of-life care in the trauma intensive care unit. J Trauma Inj Infect Crit Care. 2008;64(6):1587–93.
Hwang F, Pentakota SR, Glass NE, Berlin A, Livingston DH, Mosenthal AC. Older patients with severe traumatic brain injury: national variability in palliative care. J Surg Res. 2020;246:224–30.
WHO | WHO Definition of Palliative Care [Internet]. WHO. [cited 2020 Oct 8];Available from: https://www.who.int/cancer/palliative/definition/en/.
Dumanovsky T, Augustin R, Rogers M, Lettang K, Meier DE, Morrison RS. The growth of palliative care in U.S. hospitals: a status report. J Palliat Med. 2016;19(1):8–15.
Morrison RS, Dietrich J, Ladwig S, et al. Palliative care consultation teams cut hospital costs for medicaid beneficiaries. Health Aff. 2011;30(3):454–63.
McGraw C, Vogel R, Redmond D, et al. Comparing satisfaction of trauma patients 55 years or older to their caregivers during palliative care: who faces the burden? J Trauma Acute Care Surg. 2021;90(2):305–12.
Berry C, Ley EJ, Mirocha J, Salim A. Race affects mortality after moderate to severe traumatic brain injury. J Surg Res. 2010;163(2):303–8.
Arango-Lasprilla JC, Rosenthal M, Deluca J, et al. Traumatic brain injury and functional outcomes: does minority status matter? Brain Inj. 2007;21(7):701–8.
Williamson T, Ryser MD, Ubel PA, et al. Withdrawal of life-supporting treatment in severe traumatic brain injury. JAMA Surg. 2020;155:723–31.
Givler A, Bhatt H, Maani-Fogelman PA. The importance of cultural competence in pain and palliative care [Internet]. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2021 [cited 2021 Jun 4]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK493154/.
Waters CM. End-of-life care directives among African Americans: lessons learned–a need for community-centered discussion and education. J Community Health Nurs. 2000;17(1):25–37.
Jones RC, Creutzfeldt CJ, Cox CE, et al. Racial and ethnic differences in health care utilization following severe acute brain injury in the United States. J Intensive Care Med 2020;885066620945911.
Agency for Healthcare Research and Quality, Rockville, MD. HCUP-US NIS Overview [Internet]. Healthcare Cost and Utilization Project (HCUP). 2011. [cited 2020 Nov 5];Available from: https://www.hcup-us.ahrq.gov/nisoverview.jsp.
ICD-10 Coding Guidance for Traumatic Brain Injury Training Slides [Internet]. Defense and Veterans Brain Injury Center. 2015. [cited 2020 Nov 5];Available from: https://dvbic.dcoe.mil/material/icd-10-coding-guidance-traumatic-brain-injury-training-slides.
Clark DE, Osler TM, Hahn DR. ICDPIC: Stata module to provide methods for translating International Classification of Diseases (Ninth Revision) diagnosis codes into standard injury categories and/or scores [Internet]. 2009. Available from: https://ideas.repec.org/c/boc/bocode/s457028.html.
Taylor CA, Greenspan AI, Xu L, Kresnow M-J. Comparability of national estimates for traumatic brain injury-related medical encounters. J Head Trauma Rehabil. 2015;30(3):150–9.
Cohen SM, Lekan D, Risoli T, et al. Association between dysphagia and inpatient outcomes across frailty level among patients ≥ 50 years of age. Dysphagia. 2020;35(5):787–97.
Consumer Price Index Data from 1913 to 2020 [Internet]. US Inflation Calculator. 2008 [cited 2020 Oct 26];Available from: https://www.usinflationcalculator.com/inflation/consumer-price-index-and-annual-percent-changes-from-1913-to-2008/.
Singh T, Peters SR, Tirschwell DL, Creutzfeldt CJ. Palliative care for hospitalized patients with stroke: results from the 2010 to 2012 National inpatient sample. Stroke. 2017;48(9):2534–40.
Murthy SB, Moradiya Y, Hanley DF, Ziai WC. Palliative care utilization in Nontraumatic Intracerebral Hemorrhage in the United States. Crit Care Med. 2016;44(3):575–82.
Ruck JM, Canner JK, Smith TJ, Johnston FM. Use of inpatient palliative care by type of malignancy. J Palliat Med. 2018;21(9):1300–7.
Houchens RL, Ross D, Elixhauser A. HCUP-US Methods Series [Internet]. Agency for Healthcare Research and Quality. [cited 2020 Nov 4];Available from: https://www.hcup-us.ahrq.gov/reports/methods/methods.jsp.
Agency for Healthcare Research and Quality, Rockville, MD. Healthcare Cost and Utilization Project (HCUP) [Internet]. 2008 [cited 2021 Mar 10];Available from: https://www.hcup-us.ahrq.gov/db/vars/siddistnote.jsp?var=hispanic.
Knol MJ, VanderWeele TJ. Recommendations for presenting analyses of effect modification and interaction. Int J Epidemiol. 2012;41(2):514–20.
Yelland LN, Salter AB, Ryan P. Performance of the modified Poisson regression approach for estimating relative risks from clustered prospective data. Am J Epidemiol. 2011;174(8):984–92.
Assmann SF, Hosmer DW, Lemeshow S, Mundt KA. Confidence intervals for measures of interaction. Epidemiology. 1996;7(3):286–90.
Roeland EJ, Triplett DP, Matsuno RK, Boero IJ, Hwang L, Yeung HN, Mell L, Murphy JD. Patterns of palliative care consultation among elderly patients with cancer. J Natl Compr Cancer Netw. 2016;14(4):439–45.
Mosenthal AC. Dying of traumatic brain injury-palliative care too soon, or too late? JAMA Surg. 2020;155(8):731.
Bonner GJ, Freels S, Ferrans C, et al. Advance care planning for african american caregivers of relatives with dementias: cluster randomized controlled trial. Am J Hosp Palliat Care. 2021;38(6):547–56.
Ormseth CH, Falcone GJ, Jasak SD, et al. Minority patients are less likely to undergo withdrawal of care after spontaneous intracerebral hemorrhage. Neurocrit Care. 2018;29(3):419–25.
Johnson KS. Racial and ethnic disparities in palliative care. J Palliat Med. 2013;16(11):1329–34.
Crawley L, Payne R, Bolden J, et al. Palliative and end-of-life care in the African American community. JAMA. 2000;284(19):2518–21.
Kwok AC, Semel ME, Lipsitz SR, et al. The intensity and variation of surgical care at the end of life: a retrospective cohort study. Lancet. 2011;378(9800):1408–13.
Livingston DH, Mosenthal AC. Withdrawing life-sustaining therapy for patients with severe traumatic brain injury. CMAJ. 2011;183(14):1570–1.
Hua M, Li G, Clancy C, Morrison RS, Wunsch H. Validation of the V66.7 code for palliative care consultation in a single academic medical center. J Palliat Med. 2017;20(4):372–7.
Feder SL, Redeker NS, Jeon S, et al. Validation of the ICD-9 diagnostic code for palliative care in patients hospitalized with heart failure within the Veterans health administration. Am J Hosp Palliat Care. 2018;35(7):959–65.
Funding
Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR002553. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
TLW, SMA, CS, LTC, H-JL, JMK designed and conceptualized the study, analyzed and interpreted the data, and drafted the manuscript for intellectual content. TM, ZY, ANG analyzed and interpreted the data and drafted the manuscript for intellectual content. BAP, MEL designed and conceptualized the study and edited the manuscript for intellectual content. PAU, SPL designed and conceptualized the study, analyzed and interpreted the data, and edited the manuscript for intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Lemmon receives salary support from the National Institute of Neurological Disorders and Stroke (K23NS116453). The remaining authors have no conflicts to disclose.
Ethical Approval/Informed Consent
This article complies with ethical approval and informed consent for human studies.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.

Rights and permissions
About this article
Cite this article
Williamson, T.L., Adil, S.M., Shalita, C. et al. Palliative Care Consultations in Patients with Severe Traumatic Brain Injury: Who Receives Palliative Care Consultations and What Does that Mean for Utilization?. Neurocrit Care 36, 781–790 (2022). https://doi.org/10.1007/s12028-021-01366-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-021-01366-2