Abstract
Background
Status myoclonus (SM) after cardiac arrest (CA) may signify devastating brain injury. We hypothesized that SM correlates with severe neurologic and systemic post-cardiac-arrest syndrome (PCAS).
Methods
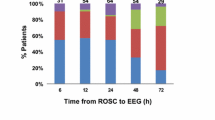
Charts of patients admitted with CA to Mayo Clinic Saint Marys Hospital between 2005 and 2019 were retrospectively reviewed. Data included the neurologic examination, ancillary neurologic tests, and systemic markers of PCAS. Nonsustained myoclonus was clinically differentiated from SM. The cerebral performance category score at discharge was assessed; poor outcome was a cerebral performance category score > 2 prior to withdrawal of life-sustaining therapies or death.
Results
Of 296 patients included, 276 (93.2%) had out-of-hospital arrest and 202 (68.5%) had a shockable rhythm; the mean time to return of spontaneous circulation was 32 ± 19 min. One hundred seventy-six (59.5%) patients had a poor outcome. One hundred one (34.1%) patients had myoclonus, and 74 (73.2%) had SM. Neurologic predictors of poor outcome were extensor or absent motor response to noxious stimulus (p = 0.02, odds ratio [OR] 3.8, confidence interval [CI] 1.2–12.4), SM (p = 0.01, OR 10.3, CI 1.5–205.4), and burst suppression on EEG (p = 0.01, OR 4.6, CI 1.4–17.4). Of 74 patients with SM, 73 (98.6%) had a poor outcome. A nonshockable rhythm (p < 0.001, OR 4.5, CI 2.6–7.9), respiratory arrest (p < 0.001, OR 3.5, CI 1.7–7.2), chronic kidney disease (p < 0.001, OR 3.1, CI 1.6–6.0), and a pressor requirement (p < 0.001, OR 4.4, CI 1.8–10.6) were associated with SM. No patients with SM, anoxic-ischemic magnetic resonance imaging findings, and absent electroencephalographic reactivity had a good outcome.
Conclusions
Sustained status myoclonus after CPR is observed in patients with other reliable indicators of severe acute brain injury and systemic PCAS. These clinical determinants should be incorporated as part of a comprehensive approach to prognostication after CA.
Similar content being viewed by others
References
Wijdicks EF, Parisi JE, Sharbrough FW. Prognostic value of myoclonus status in comatose survivors of cardiac arrest. Ann Neurol. 1994;35(2):239–43.
Young GB, Gilbert JJ, Zochodne DW. The significance of myoclonic status epilepticus in postanoxic coma. Neurology. 1990;40(12):1843–8.
Jumao-as A, Brenner RP. Myoclonic status epilepticus: a clinical and electroencephalographic study. Neurology. 1990;40(8):1199–202.
Elmer J, et al. Association of early withdrawal of life-sustaining therapy for perceived neurological prognosis with mortality after cardiac arrest. Resuscitation. 2016;102:127–35.
Dhakar MB, et al. Electro-clinical characteristics and prognostic significance of post anoxic myoclonus. Resuscitation. 2018;131:114–20.
Seder DB, et al. Neurologic outcomes and postresuscitation care of patients with myoclonus following cardiac arrest. Crit Care Med. 2015;43(5):965–72.
Greer DM, Rosenthal ES, Wu O. Neuroprognostication of hypoxic–ischaemic coma in the therapeutic hypothermia era. Nat Rev Neurol. 2014;10(4):190–203.
Greer DM. Unexpected good recovery in a comatose post-cardiac arrest patient with poor prognostic features. Resuscitation. 2013;84(6):e81–2.
Greer DM, et al. Clinical examination for prognostication in comatose cardiac arrest patients. Resuscitation. 2013;84(11):1546–51.
Neumar RW, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; and the Stroke Council. Circulation. 2008;118(23):2452–83.
Nolan JP, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication: a scientific statement from the International Liaison Committee on Resuscitation; the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; the Council on Stroke (Part 1). Int Emerg Nurs. 2009;17(4):203–25.
Nielsen N, et al. Targeted temperature management at 33°C versus 36°C after cardiac arrest. N Engl J Med. 2013;369(23):2197–206.
Hawkes MA, Rabinstein AA. Neurological prognostication after cardiac arrest in the era of target temperature management. Curr Neurol Neurosci Rep. 2019;19(2):10.
Nolan JP, et al. European resuscitation council and European society of intensive care medicine 2015 guidelines for post-resuscitation care. Intensive Care Med. 2015;41(12):2039–56.
Wijdicks EF, Young GB. Myoclonus status in comatose patients after cardiac arrest. Lancet. 1994;343(8913):1642–3.
Wijdicks EF, et al. Practice parameter: prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2006;67(2):203–10.
Fugate JE, et al. Predictors of neurologic outcome in hypothermia after cardiac arrest. Ann Neurol. 2010;68(6):907–14.
Krumholz A, Stern BJ, Weiss HD. Outcome from coma after cardiopulmonary resuscitation: relation to seizures and myoclonus. Neurology. 1988;38(3):401–5.
van Zijl JC, et al. Electroencephalographic findings in posthypoxic myoclonus. J Intensive Care Med. 2016;31(4):270–5.
Rossetti AO, et al. Predictors of awakening from postanoxic status epilepticus after therapeutic hypothermia. Neurology. 2009;72(8):744–9.
Kamps MJA, et al. Prognostication of neurologic outcome in cardiac arrest patients after mild therapeutic hypothermia: a meta-analysis of the current literature. Intensive Care Med. 2013;39(10):1671–82.
Rossetti AO, Rabinstein AA, Oddo M. Neurological prognostication of outcome in patients in coma after cardiac arrest. Lancet Neurol. 2016;15(6):597–609.
Sandroni C, et al. Predictors of poor neurological outcome in adult comatose survivors of cardiac arrest: a systematic review and meta-analysis. Part 2: patients treated with therapeutic hypothermia. Resuscitation. 2013;84(10):1324–38.
Rossetti AO, et al. Prognostication after cardiac arrest and hypothermia: a prospective study. Ann Neurol. 2010;67(3):301–7.
Ben-Hamouda N, et al. Contemporary approach to neurologic prognostication of coma after cardiac arrest. Chest. 2014;146(5):1375–86.
Rossetti AO, et al. Status epilepticus: an independent outcome predictor after cerebral anoxia. Neurology. 2007;69(3):255–60.
Barbella G, et al. Prediction of regaining consciousness despite an early epileptiform EEG after cardiac arrest. Neurology. 2020;94(16):e1675–83.
Oh SH, et al. Prognostic value of somatosensory evoked potential in cardiac arrest patients without withdrawal of life-sustaining therapy. Resuscitation. 2020;150:154–61.
Maciel CB, et al. Corneal reflex testing in the evaluation of a comatose patient: an ode to precise semiology and examination skills. Neurocrit Care. 2020;33(2):399–404.
English WA, Giffin NJ, Nolan JP. Myoclonus after cardiac arrest: pitfalls in diagnosis and prognosis. Anaesthesia. 2009;64(8):908–11.
Braksick SA, et al. Post-ischemic myoclonic status following cardiac arrest in young drug users. Neurocrit Care. 2017;26(2):280–3.
Hahn DK, Geocadin RG, Greer DM. Quality of evidence in studies evaluating neuroimaging for neurologic prognostication in adult patients resuscitated from cardiac arrest. Resuscitation. 2014;85(2):165–72.
Ruijter BJ, et al. Early electroencephalography for outcome prediction of postanoxic coma: a prospective cohort study. Ann Neurol. 2019;86(2):203–14.
Rossetti AO, et al. Electroencephalography predicts poor and good outcomes after cardiac arrest: a two-center study*. Crit Care Med. 2017;45(7):e674–82.
Beuchat I, et al. MRI–EEG correlation for outcome prediction in postanoxic myoclonus. A Multicenter Study. 2020;95(4):e335–41.
Dutta A, et al. Incidence, predictors, and prognosis of acute kidney injury among cardiac arrest survivors. J Intensive Care Med. 2020;36:550–6.
Dragancea I, et al. Neurological prognostication after cardiac arrest and targeted temperature management 33 degrees C versus 36 degrees C: results from a randomised controlled clinical trial. Resuscitation. 2015;93:164–70.
Hirsch KG, et al. Prognostic value of diffusion-weighted MRI for post-cardiac arrest coma. Neurology. 2020;94(16):e1684–92.
Hirsch KG, et al. Prognostic value of a qualitative brain MRI scoring system after cardiac arrest. J Neuroimaging. 2015;25(3):430–7.
Acknowledgements
Mania Hajeb, MD, and Marianella Hernandez, MD, both collected data.
Funding
None.
Author information
Authors and Affiliations
Contributions
TC, MD, authored, conceptualized, drafted, and revised the manuscript and analyzed and acquired data. She had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. SB, MD, conceptualized and revised the manuscript and analyzed data. AAR, MD, authored, conceptualized, drafted, and revised the manuscript. EW, MD, PhD, authored, conceptualized, drafted, and revised the manuscript.
Corresponding author
Ethics declarations
Ethical Approval/Informed Consent
The Mayo Clinic Institutional Review Board approved this study. Patients and/or their authorized representatives provided written consent for their deidentified information to be used for research purposes.
Conflict of interest
The authors report no disclosures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chakraborty, T., Braksick, S., Rabinstein, A. et al. Status Myoclonus with Post-cardiac-arrest Syndrome: Implications for Prognostication. Neurocrit Care 36, 387–394 (2022). https://doi.org/10.1007/s12028-021-01344-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-021-01344-8