Abstract
Background
Severe intracranial hypertension is strongly associated with mortality. Guidelines recommend medical management involving sedation, hyperosmotic agents, barbiturates, hypothermia, and surgical intervention. When these interventions are maximized or are contraindicated, refractory intracranial hypertension poses risk for herniation and death. We describe a novel intervention of verticalization for treating intracranial hypertension refractory to aggressive medical treatment.
Methods
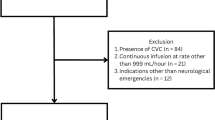
This study was a single-center retrospective review of six cases of refractory intracranial hypertension in a tertiary care center. All patients were treated with a standard-of-care algorithm for lowering intracranial pressure (ICP) yet maintained an ICP greater than 20 mmHg. They were then treated with verticalization for at least 24 h. We compared the median ICP, the number of ICP spikes greater than 20 mmHg, and the percentage of ICP values greater than 20 mmHg in the 24 h before verticalization vs. after verticalization. We assessed the use of hyperosmotic therapies and any changes in the mean arterial pressure and cerebral perfusion pressure related with the intervention.
Results
Five patients were admitted with subarachnoid hemorrhage and one with intracerebral hemorrhage. All patients had ICP monitoring by external ventricular drain. The median opening pressure was 30 mmHg (25th–75th interquartile range 22.5–30 mmHg). All patients demonstrated a reduction in ICP after verticalization, with a significant decrease in the median ICP (12 vs. 8 mmHg; p < 0.001), the number of ICP spikes (12 vs. 2; p < 0.01), and the percentage of ICP values greater than 20 mmHg (50% vs. 8.3%; p < 0.01). There was a decrease in total medical interventions after verticalization (79 vs. 41; p = 0.05) and a lower total therapy intensity level score after verticalization. The most common adverse effects included asymptomatic bradycardia (n = 3) and pressure wounds (n = 4).
Conclusions
Verticalization is an effective noninvasive intervention for lowering ICP in intracranial hypertension that is refractory to aggressive standard management and warrants further study.



Similar content being viewed by others
References
Freeman WD. Management of intracranial pressure. Continuum (Minneap Minn). 2015;21(5 Neurocritical Care):1299–323.
Marmarou A, Saad A, Aygok G, Rigsbee M. Contribution of raised ICP and hypotension to CPP reduction in severe brain injury: correlation to outcome. Acta Neurochir Suppl. 2005;95:277–80.
Aiolfi A, Benjamin E, Khor D, Inaba K, Lam L, Demetriades D. Brain trauma foundation guidelines for intracranial pressure monitoring: compliance and effect on outcome. World J Surg. 2017;41(6):1543–9.
Connolly ES Jr, Rabinstein AA, Carhuapoma JR, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2012;43(6):1711–37.
Hemphill JC 3rd, Greenberg SM, Anderson CS, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46(7):2032–60.
Kelly DF, Goodale DB, Williams J, et al. Propofol in the treatment of moderate and severe head injury: a randomized, prospective double-blinded pilot trial. J Neurosurg. 1999;90(6):1042–52.
Ropper AH. Management of raised intracranial pressure and hyperosmolar therapy. Pract Neurol. 2014;14(3):152–8.
Marshall GT, James RF, Landman MP, et al. Pentobarbital coma for refractory intra-cranial hypertension after severe traumatic brain injury: mortality predictions and one-year outcomes in 55 patients. J Trauma. 2010;69(2):275–83.
Hayman EG, Kurland DB, Grunwald Z, Urday S, Sheth KN, Simard JM. Decompressive craniectomy in neurocritical care. Semin Neurol. 2016;36(6):508–19.
Trial of decompressive craniectomy for traumatic intracranial hypertension. J Intensive Care Soc. 2017;18(3):236–8.
Cooper DJ, Rosenfeld JV, Murray L, et al. Decompressive craniectomy in diffuse traumatic brain injury. N Engl J Med. 2011;364(16):1493–502.
Andrews PJ, Harris BA, Murray GD. Hypothermia for intracranial hypertension after traumatic brain injury. N Engl J Med. 2016;374(14):1385.
Presneill J, Gantner D, Nichol A, et al. Statistical analysis plan for the POLAR-RCT: the Prophylactic hypOthermia trial to Lessen trAumatic bRain injury-Randomised Controlled Trial. Trials. 2018;19(1):259.
Cadena R, Shoykhet M, Ratcliff JJ. Emergency neurological life support: intracranial hypertension and herniation. Neurocrit Care. 2017;27(Suppl 1):82–8.
Vidale S, Bellocchi S, Taborelli A. Surgery for cerebral haemorrhage—STICH II trial. Lancet. 2013;382(9902):1401–2.
Levey AS, Eckardt KU, Dorman NM, et al. Nomenclature for kidney function and disease: executive summary and glossary from a kidney disease: improving global outcomes (KDIGO) consensus conference. Kidney Dis (Basel). 2020;6(5):309–17.
Ziai WC, Melnychuk E, Thompson CB, Awad I, Lane K, Hanley DF. Occurrence and impact of intracranial pressure elevation during treatment of severe intraventricular hemorrhage. Crit Care Med. 2012;40(5):1601–8.
Eide PK, Fremming AD. A new method and software for quantitative analysis of continuous intracranial pressure recordings. Acta Neurochir (Wien). 2001;143(12):1237–47.
Gregori-Pla C, Blanco I, Camps-Renom P, et al. Early microvascular cerebral blood flow response to head-of-bed elevation is related to outcome in acute ischemic stroke. J Neurol. 2019;266(4):990–7.
Gorbachev VI, Likholetova NV, Gorbacheva SM, Sedova EY. Effects of body positioning in patients with non-traumatic intracranial hemorrhages. Zh Nevrol Psikhiatr Im S S Korsakova. 2016;116(11):131–6 (Russian).
Feldman Z, Kanter MJ, Robertson CS, et al. Effect of head elevation on intracranial pressure, cerebral perfusion pressure, and cerebral blood flow in head-injured patients. J Neurosurg. 1992;76(2):207–11.
Kenning JA, Toutant SM, Saunders RL. Upright patient positioning in the management of intracranial hypertension. Surg Neurol. 1981;15(2):148–52.
Rosner MJ, Coley IB. Cerebral perfusion pressure, intracranial pressure, and head elevation. J Neurosurg. 1986;65(5):636–41.
Aries MJ, Elting JW, Stewart R, De Keyser J, Kremer B, Vroomen P. Cerebral blood flow velocity changes during upright positioning in bed after acute stroke: an observational study. BMJ Open. 2013;3(8):e002960.
Kumble S, Zink EK, Burch M, Deluzio S, Stevens RD, Bahouth MN. Physiological effects of early incremental mobilization of a patient with acute intracerebral and intraventricular hemorrhage requiring dual external ventricular drainage. Neurocrit Care. 2017;27(1):115–9.
Fazilleau S. Early in-bed tilting in neurological intensive care unit: feasibility and interest. Ann Phys Rehabil Med. 2016;59:e153.
Carvalho LB, Kramer S, Borschmann K, Chambers B, Thijs V, Bernhardt J. Cerebral haemodynamics with head position changes post-ischaemic stroke: a systematic review and meta-analysis. J Cereb Blood Flow Metab. 2020;40(10):1917–33.
Grande PO. Critical evaluation of the lund concept for treatment of severe traumatic head injury, 25 years after its introduction. Front Neurol. 2017;8:315.
Asgeirsson B, Grande PO. Local vascular responses to elevation of an organ above the heart. Acta Physiol Scand. 1996;156(1):9–18.
Dorfman JD, Burns JD, Green DM, DeFusco C, Agarwal S. Decompressive laparotomy for refractory intracranial hypertension after traumatic brain injury. Neurocrit Care. 2011;15(3):516–8.
Joseph DK, Dutton RP, Aarabi B, Scalea TM. Decompressive laparotomy to treat intractable intracranial hypertension after traumatic brain injury. J Trauma. 2004;57(4):687–93 (discussion 693–5).
Shehabi Y, Bellomo R, Kadiman S, et al. Sedation intensity in the first 48 hours of mechanical ventilation and 180-day mortality: a multinational prospective longitudinal cohort study. Crit Care Med. 2018;46(6):850–9.
Devlin JW, Skrobik Y, Gelinas C, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018;46(9):e825–73.
Torre-Healy A, Marko NF, Weil RJ. Hyperosmolar therapy for intracranial hypertension. Neurocrit Care. 2012;17(1):117–30.
Roberts I, Sydenham E. Barbiturates for acute traumatic brain injury. Cochrane Database Syst Rev. 2012;12:CD000033.
Hainsworth R. Pathophysiology of syncope. Clin Auton Res. 2004;14(Suppl 1):18–24.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the conception and design, acquisition of data, and/or analysis and interpretation of data. All authors provided critical revision of the manuscript content, and all authors approved the final version of the manuscript for publication.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to disclose.
Ethical approval/informed consent
This project adhered to ethical guidelines and requirements and was approved by the local institutional review board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
12028_2021_1323_MOESM1_ESM.docx
LR: Lindegaard Ratio; MCA: Middle Cerebral Artery; MV: Mean Velocity; PBD: Post-Bleed Day; PI: Pulsatility Index; SAH: Subarachnoid Hemorrhage; TCD: Transcranial Doppler. (DOCX 18 kb)
Rights and permissions
About this article
Cite this article
Lachance, B.B., Chang, W., Motta, M. et al. Verticalization for Refractory Intracranial Hypertension: A Case Series. Neurocrit Care 36, 463–470 (2022). https://doi.org/10.1007/s12028-021-01323-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-021-01323-z