Abstract
Background
Despite one third of children with acquired brain injury (ABI) experiencing new functional impairments following critical care admission, there is limited research investigating the impact of new functional impairments on overall health-related quality of life (HRQOL) or among important HRQOL domains. We aimed to investigate the association between new functional impairments, measured by the Functional Status Scale (FSS), and HRQOL in pediatric patients with ABI after critical care.
Methods
We conducted a secondary analysis of a prospective observational study of 275 children aged 2 months to 18 years with ABI. The primary exposure evaluated was change in FSS from baseline at hospital discharge, categorized per prior work (no change, 1–2 point increase, and ≥ 3 point increase). The primary outcome was overall HRQOL 6 months after hospital discharge, measured by the Pediatric Quality of Life Inventory (PedsQL) total score. Secondary outcomes were PedsQL domain scores. PedsQL total and domain scores were transformed into age-standardized z scores for analyses. Multiple linear regression models evaluated the association between FSS change category and HRQOL (overall and domain z scores) when controlling for demographic and clinical characteristics and were reported as β-coefficients with 95% confidence intervals.
Results
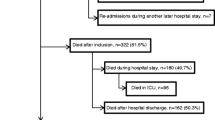
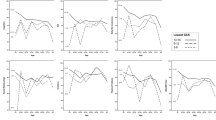
Complete data were analyzed for 195 (71%) children, including 127 with traumatic brain injury. New functional impairment was common with 32 (16%) patients experiencing FSS increases ≥ 3, 50 (26%) patients with FSS increases of 1–2 points, and 113 (58%) patients with no change from prehospital baseline. The majority of children (63%) demonstrated HRQOL ratings ≥ 1 standard deviation below healthy age-based standards (z scores ≤ − 1). Regression models demonstrated older age, female sex, presence of comorbidities, and preadmission cardiopulmonary resuscitation were all significantly associated with poorer overall HRQOL (all p < 0.05). FSS increase ≥ 3 at discharge was significantly associated with worse overall HRQOL at follow-up (β = − 1.07; 95% confidence interval = − 1.63 to − 0.52) when controlling for the aforementioned significant factors, and significantly improved model fit (p value for change = 0.001). Similar findings in secondary analyses were found for physical domain scores, with FSS increase showing a significant association with worse physical HRQOL scores and improvements in model fit. Change in FSS was not significantly associated with other HRQOL domain scores (emotional, social, school, psychosocial).
Conclusions
Many children with ABI after critical care experience new functional impairments (FSS increases) and worse HRQOL than healthy peers. FSS increase at discharge is a significant risk factor for worse HRQOL in the months after hospital discharge and improves HRQOL models beyond illness and demographic variables alone.
Similar content being viewed by others
References
Williams CN, Eriksson CO, Kirby A, et al. Hospital mortality and functional outcomes in pediatric neurocritical care. Hosp Pediatr. 2019;9(12):958–66.
Pollack MM, Holubkov R, Funai T, et al. Pediatric intensive care outcomes: development of new morbidities during pediatric critical care. Pediatr Crit Care Med. 2014;15(9):821.
Pollack MM, Holubkov R, Funai T, et al. Relationship between the functional status scale and the pediatric overall performance category and pediatric cerebral performance category scales. JAMA Pediatr. 2014;168(7):671–6.
Manning JC, Pinto NP, Rennick JE, Colville G, Curley MA. Conceptualizing post intensive care syndrome in children—the PICS-p framework. Pediatr Crit Care Med. 2018;19(4):298–300.
Watson RS, Choong K, Colville G, et al. Life after critical illness in children—toward an understanding of pediatric post-intensive care syndrome. J Pediatr. 2018;198:16–24.
Herrup EA, Wieczorek B, Kudchadkar SR. Characteristics of postintensive care syndrome in survivors of pediatric critical illness: a systematic review. World J Crit Care Med. 2017;6(2):124.
Williams CN, Hartman ME, Guilliams KP, et al. Postintensive care syndrome in pediatric critical care survivors: therapeutic options to improve outcomes after acquired brain injury. Curr Treat Options Neurol. 2019;21(10):49.
Hartman ME, Williams CN, Hall TA, Bosworth CC, Piantino JA. Post-intensive care syndrome for the pediatric neurologist. Pediatr Neurol. 2020;108:47–53.
Hall TA, Leonard S, Bradbury K, et al. Post-intensive care syndrome in a cohort of infants & young children receiving integrated care via a pediatric critical care & neurotrauma recovery program: a pilot investigation. Clin Neuropsychol. 2020. https://doi.org/10.1080/13854046.2020.1797176.
Cordts KMP, Hall TA, Hartman ME, et al. Sleep measure validation in a pediatric neurocritical care acquired brain injury population. Neurocrit Care. 2019;33:1–11.
Aspesberro F, Fesinmeyer MD, Zhou C, Zimmerman JJ, Mangione-Smith R. Construct validity and responsiveness of the pediatric quality of life inventory 4.0 generic core scales and infant scales in the PICU. Pediatr Crit Care Med. 2016;17(6):e272–9.
Cunha F, Mota T, Teixeira-Pinto A, et al. Factors associated with health-related quality of life changes in survivors to pediatric intensive care. Pediatr Crit Care Med|Soc Crit Care Med. 2013;14(1):e8–15.
Erickson SJ, Montague EQ, Gerstle MA. Health-related quality of life in children with moderate-to-severe traumatic brain injury. Dev Neurorehabil. 2010;13(3):175–81.
Polic B, Mestrovic J, Markic J, et al. Long-term quality of life of patients treated in paediatric intensive care unit. Eur J Pediatr. 2013;172(1):85–90.
Mestrovic J, Kardum G, Sustic A, et al. Neurodevelopmental disabilities and quality of life after intensive care treatment. J Paediatr Child Health. 2007;43(10):673–6.
Brown EA, Kenardy J, Chandler B, et al. Parent-reported health-related quality of life in children with traumatic brain injury: a prospective study. J Pediatr Psychol. 2016;41(2):244–55.
Knoester H, Bronner MB, Bos AP, Grootenhuis MA. Quality of life in children three and nine months after discharge from a paediatric intensive care unit: a prospective cohort study. Health Qual Life Outcomes. 2008;6(1):21.
Green L, Godfrey C, Soo C, Anderson V, Catroppa C. A preliminary investigation into psychosocial outcome and quality-of-life in adolescents following childhood traumatic brain injury. Brain Inj. 2013;27(7–8):872–7.
Colville G, Pierce C. Children’s self-reported quality of life after intensive care treatment. Pediatr Crit Care Med. 2013;14(4):446.
Ambuehl J, Karrer A, Riedel T, Schibler A. Quality of life of survivors of paediatric intensive care. Swiss Med Wkly. 2007;137(21–22):312–6.
Fineblit S, Selci E, Loewen H, Ellis M, Russell K. Health-related quality of life after pediatric mild traumatic brain injury/concussion: a systematic review. J Neurotrauma. 2016;33(17):1561–8.
Aspesberro F, Mangione-Smith R, Zimmerman JJ. Health-related quality of life following pediatric critical illness. Intensive Care Med. 2015;41(7):1235–46.
Conlon NP, Breatnach C, O’Hare BP, Mannion DW, Lyons BJ. Health-related quality of life after prolonged pediatric intensive care unit stay. Pediatr Crit Care Med. 2009;10(1):41–4.
Namachivayam P, Taylor A, Montague T, et al. Long-stay children in intensive care: long-term functional outcome and quality of life from a 20-yr institutional study. Pediatr Crit Care Med|Soc Crit Care Med. 2012;13(5):520–8.
Ebrahim S, Singh S, Hutchison JS, et al. Adaptive behavior, functional outcomes, and quality of life outcomes of children requiring urgent ICU admission. Pediatr Crit Care Med. 2013;14(1):10–8.
Treble-Barna A, Beers SR, Houtrow AJ, et al. PICU-based rehabilitation and outcomes assessment: a survey of pediatric critical care physicians. Pediatr Crit Care Med. 2019;20(6):274–82.
Dodd JN, Hall TA, Guilliams K, et al. Optimizing neurocritical care follow-up through the integration of neuropsychology. Pediatr Neurol. 2018;89:58–62.
Williams CN, Kirby A, Piantino J. If you build it, they will come: initial experience with a multi-disciplinary pediatric neurocritical care follow-up clinic. Children. 2017;4(9):83.
Bradbury K, Willimas CN, Leonard S, et al. Emotional aspects of pediatric post-intensive care syndrome following traumatic brain injury. J Child Adolesc Trauma. 2021;14(2):177–87.
Williams CN, Lim MM, Shea SA. Sleep disturbance after pediatric traumatic brain injury: critical knowledge gaps remain for the critically injured. Nat Sci Sleep. 2018;10:225.
Pinto NP, Rhinesmith EW, Kim TY, Ladner PH, Pollack MM. Long-term function after pediatric critical illness: results from the survivor outcomes study. Pediatr Crit Care Med. 2017;18(3):e122–30.
Heneghan JA, Pollack MM. Morbidity: changing the outcome paradigm for pediatric critical care. Pediatr Clin. 2017;64(5):1147–65.
Varni JW, Seid M, Kurtin PS. PedsQLTM 4.0: reliability and validity of the Pediatric Quality of Life InventoryTM version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39:800–12.
Varni JW, Limbers CA, Neighbors K, et al. The PedsQLTM infant scales: feasibility, internal consistency reliability, and validity in healthy and ill infants. Qual Life Res. 2011;20(1):45–55.
Desai AD, Zhou C, Stanford S, Haaland W, Varni JW, Mangione-Smith RM. Validity and responsiveness of the pediatric quality of life inventory (PedsQL) 4.0 generic core scales in the pediatric inpatient setting. JAMA Pediatr. 2014;168(2):1114–21.
Kruse S, Schneeberg A, Brussoni M. Construct validity and impact of mode of administration of the PedsQL among a pediatric injury population. Health Qual Life Outcomes. 2014;12(1):1–9.
Bisegger C, Cloetta B, Von Bisegger U, Abel T, Ravens-Sieberer U. Health-related quality of life: gender differences in childhood and adolescence. Sozial-und Präventivmedizin. 2005;50(5):281–91.
Varni JW, Limbers CA, Burwinkle TM. Impaired health-related quality of life in children and adolescents with chronic conditions: a comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the PedsQLTM 4.0 Generic Core Scales. Health Qual Life Outcomes. 2007;5(1):43.
Moreau JF, Fink EL, Hartman ME, et al. Hospitalizations of children with neurological disorders in the United States. Pediatr Crit Care Med. 2013;14(8):801.
Williams CN, Piantino J, McEvoy C, Fino N, Eriksson CO. The burden of pediatric neurocritical care in the United States. Pediatr Neurol. 2018;89:31–8.
Maddux AB, Cox-Martin M, Dichiaro M, Bennett TD. The association between the functional status scale and the pediatric functional independence measure in children who survive traumatic brain injury. Pediatr Crit Care Med. 2018;19(11):1046.
Author information
Authors and Affiliations
Contributions
Drs. Holding, Turner, and Williams were involved in all aspects of manuscript preparation, including conceptualization, conducting statistical analyses, data collection, and writing of the artilce. Dr. Hall was involved in the study conceptualization, data collection and interpretation, and writing of the article. Drs. Leonard and Bradbury were involved in study conceptualization, data collection, and editing of the article. The final manuscript was approved by all authors.
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Williams reports grants from Agency for Healthcare Research and Quality, and grants from the National Heart Lung and Blood Institute, and National Institutes for Health during the conduct of the study. The remaining authors declare no conflicts of interest.
Ethical approval/informed consent
The authors have adhered to the ethical guidelines, and the research was conducted under a waiver from the institutional review board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is related to the Invited commentary available at https://doi.org/10.1007/s12028-021-01270-9
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Holding, E.Z., Turner, E.M., Hall, T.A. et al. The Association Between Functional Status and Health-Related Quality of Life Following Discharge from the Pediatric Intensive Care Unit. Neurocrit Care 35, 347–357 (2021). https://doi.org/10.1007/s12028-021-01271-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-021-01271-8