Abstract
Objective
Cerebral autoregulation (CA) impairment may pose a risk factor for neurological complications among children supported by extracorporeal membrane oxygenation (ECMO). Our first objective was to investigate the feasibility of CA continuous monitoring during ECMO treatment and to describe its evolution over time. The second objective was to analyze the association between CA impairment and neurological outcome.
Design
Observational prospective study.
Patients and Setting
Twenty-nine children treated with veno-arterial or veno-venous ECMO in the PICU of Nantes University Hospital, France, and the PICU of the IRCCS Giannina Gaslini Institute in Genoa, Italy.
Measurements
A correlation coefficient between the variations of regional cerebral oxygen saturation and the variations of mean arterial blood pressure (MAP) was calculated as an index of CA (cerebral oxygenation reactivity index, COx). A COx > 0.3 was considered as indicative of autoregulation impairment. COx—MAP plots were investigated allowing determining optimal MAP (MAPopt) and limits of autoregulation: lower (LLA) and upper (ULA). Neurological outcome was assessed by the onset of an acute neurological event (ANE) after ECMO start.
Results
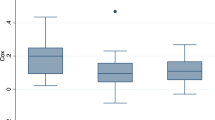
We included 29 children (median age 84 days, weight 4.8 kg). MAPopt, LLA, and ULA were detected in 90.8% (84.3–93.3) of monitoring time. Mean COx was significantly higher during day 1 of ECMO compared to day 2 [0.1 (0.02–0.15) vs. 0.01 (− 0.05 to 0.1), p = 0.002]. Twelve children experienced ANE (34.5%). The mean COx and the percentage of time spent with a COx > 0.3 were significantly higher among ANE+ compared to ANE− patients [0.09 (0.01–0.23) vs. 0.04 (− 0.02 to 0.06), p = 0.04 and 33.3% (24.8–62.1) vs. 20.8% (17.3–23.7) p = 0.001]. ANE+ patients spent significantly more time with MAP below LLA [17.2% (6.5–32.9) vs. 5.6% (3.6–9.9), p = 0.02] and above ULA [13% (5.3–38.4) vs. 4.2% (2.7–7.4), p = 0.004], respectively.
Conclusion
CA assessment is feasible in pediatric ECMO. The first 24 h following ECMO represents the most critical period regarding CA. Impaired autoregulation is significantly more severe among patients who experience ANE.




Similar content being viewed by others
Change history
02 May 2023
A Correction to this paper has been published: https://doi.org/10.1007/s12028-023-01727-z
References
Dalton HJ, Reeder R, Garcia-Filion P, Holubkov R, Berg RA, Zuppa A, et al. Factors associated with bleeding and thrombosis in children receiving extracorporeal membrane oxygenation. Am J Respir Crit Care Med. 2017;196(6):10.
Lidegran MK, Mosskin M, Ringertz HG, Frenckner BP, Lindén VB. Cranial CT for diagnosis of intracranial complications in adult and pediatric patients during ECMO: clinical benefits in diagnosis and treatment. Acad Radiol. 2007;14(1):62–71.
Paulson OB, Strandgaard S, Edvinsson L. Cerebral autoregulation. Cerebrovasc Brain Metab Rev. 1990;2(2):161–92.
Rivera-Lara L, Zorrilla-Vaca A, Geocadin R, Ziai W, Healy R, Thompson R, et al. Predictors of outcome with cerebral autoregulation monitoring: a systematic review and meta-analysis. Crit Care Med. 2017;45(4):695–704.
Brady KM, Lee JK, Kibler KK, Smielewski P, Czosnyka M, Easley RB, et al. Continuous time-domain analysis of cerebrovascular autoregulation using near-infrared spectroscopy. Stroke. 2007;38(10):2818–25.
Burton VJ, Gerner G, Cristofalo E, Chung S, Jennings JM, Parkinson C, et al. A pilot cohort study of cerebral autoregulation and 2-year neurodevelopmental outcomes in neonates with hypoxic-ischemic encephalopathy who received therapeutic hypothermia. BMC Neurol. 2018. https://doi.org/10.1186/s12883-015-0464-4.
Lee JK, Brady KM, Chung S-E, Jennings JM, Whitaker EE, Aganga D, et al. A pilot study of cerebrovascular reactivity autoregulation after pediatric cardiac arrest. Resuscitation. 2014;85(10):1387–93.
Aries MJH, Czosnyka M, Budohoski KP, Steiner LA, Lavinio A, Kolias AG, et al. Continuous determination of optimal cerebral perfusion pressure in traumatic brain injury. Crit Care Med. 2012;40(8):2456–63.
Ono M, Brady K, Easley RB, Brown C, Kraut M, Gottesman RF, et al. Duration and magnitude of blood pressure below cerebral autoregulation threshold during cardiopulmonary bypass is associated with major morbidity and operative mortality. J Thorac Cardiovasc Surg. 2014;147(1):483–9.
Crippa IA, Subirà C, Vincent JL et al. Impaired cerebral autoregulation is associated with brain dysfunction in patients with sepsis. Crit Care 2018;22(1):327
Short BL, Walker LK, Bender KS, Traystman RJ. Impairment of cerebral autoregulation during extracorporeal membrane oxygenation in newborn lambs. Pediatr Res. 1993;33(3):289–94.
Ingyinn M, Rais-Bahrami K, Viswanathan M, Short BL. Altered cerebrovascular responses after exposure to venoarterial extracorporeal membrane oxygenation: role of the nitric oxide pathway. Pediatr Crit Care Med. 2006;7(4):368–73.
Tian F, Morriss MC, Chalak L, Venkataraman R, Ahn C, Liu H, et al. Impairment of cerebral autoregulation in pediatric extracorporeal membrane oxygenation associated with neuroimaging abnormalities. Neurophotonics. 2017;4(04):1.
Zamora CA, Oshmyansky A, Bembea M, Berkowitz I, Alqahtani E, Liu S, et al. Resistive index variability in anterior cerebral artery measurements during daily transcranial duplex sonography. J Ultrasound Med. 2016;35(11):2459–65
Busch DR, Baker WB, Mavroudis CD, Ko TS, Lynch JM, McCarthy AL, et al. Noninvasive optical measurement of microvascular cerebral hemodynamics and autoregulation in the neonatal ECMO patient. Pediatr Res. 2020. https://doi.org/10.1038/s41390-020-0841-6.
Czosnyka M, Brady K, Reinhard M, Smielewski P, Steiner LA. Monitoring of cerebrovascular autoregulation: facts, myths, and missing links. Neurocrit Care. 2009;10:373–86.
Depreitere B, Güiza F, Van den Berghe G, Schuhmann MU, Maier G, Piper I, et al. Pressure autoregulation monitoring and cerebral perfusion pressure target recommendation in patients with severe traumatic brain injury based on minute-by-minute monitoring data. J Neurosurg. 2014;120(6):1451–7.
Liu X, Maurits NM, Aries MJH, Czosnyka M, Ercole A, Donnelly J, et al. Monitoring of optimal cerebral perfusion pressure in traumatic brain injured patients using a multi-window weighting algorithm. J Neurotrauma. 2017;34(22):3081–8.
Beqiri E, Smielewski P, Robba C, Czosnyka M, Cabeleira MT, Tas J, et al. Feasibility of individualised severe traumatic brain injury management using an automated assessment of optimal cerebral perfusion pressure: the COGiTATE phase II study protocol. BMJ Open. 2019;9(9):e030727.
Bell JL, Saenz L, Domnina Y, Baust T, Panigrahy A, Bell MJ, et al. Acute neurologic injury in children admitted to the cardiac intensive care unit. Ann Thorac Surg. 2019;107:1831–7.
Cavayas YA, Munshi L, Del Sorbo L, Fan E. The early change in PaCO2 after extracorporeal membrane oxygenation initiation is associated with neurological complications. Am J Respir Crit Care Med. 2020;201(12):1525–35.
Hervey-Jumper SL, Annich GM, Yancon AR, Garton HJL, Muraszko KM, Maher CO. Neurological complications of extracorporeal membrane oxygenation in children: clinical article. J Neurosurg Pediatr. 2011;7(4):338–44.
Okochi S, Shakoor A, Barton S, Zenilman AR, Street C, Streltsova S, et al. Prevalence of seizures in pediatric extracorporeal membrane oxygenation patients as measured by continuous electroencephalography. Neurocrit Care. 2018;19(12):6.
Cashen K, Reeder R, Dalton HJ, Berg RA, Shanley TP, Newth CJL, et al. Hyperoxia and hypocapnia during pediatric extracorporeal membrane oxygenation: associations with complications, mortality, and functional status among survivors. Pediatr Crit Care Med. 2018;19(3):9.
Walker LK, Short BL, Traystman RJ. Impairment of cerebral autoregulation during venovenous extracorporeal membrane oxygenation in the newborn lamb. Crit Care Med. 1996;24(12):2001–6.
LaRovere KL, Vonberg FW, Prabhu SP, Kapur K, Harini C, Garcia-Jacques R, et al. Patterns of head computed tomography abnormalities during pediatric extracorporeal membrane oxygenation and association with outcomes. Pediatr Neurol. 2017;73:64–70.
Luyt C-E, Bréchot N, Demondion P, Jovanovic T, Hékimian G, Lebreton G, et al. Brain injury during venovenous extracorporeal membrane oxygenation. Intensive Care Med. 2016;42(5):897–907.
Cavayas YA, Munshi L, del Sorbo L, Fan E. The early change in PaCO2 after extracorporeal membrane oxygenation initiation is associated with neurological complications. Am J Respir Crit Care Med. 2020. https://doi.org/10.1164/rccm.202001-0023OC.
Heggen JA, Fortenberry JD, Tanner AJ, Reid CA, Mizzell DW, Pettignano R. Systemic hypertension associated with venovenous extracorporeal membrane oxygenation for pediatric respiratory failure. J Pediatr Surg. 2004;39(11):1626–31.
van Heijst A, Liem D, Hopman J, van der Staak F, Sengers R. Oxygenation and hemodynamics in left and right cerebral hemispheres during induction of veno-arterial extracorporeal membrane oxygenation. J Pediatr. 2004;144(2):223–8.
Papademetriou M, Tachtsidis I, Elliott MJ, Hoskote A, Elwell CE. Wavelet cross-correlation to investigate regional variations in cerebral oxygenation in infants supported on extracorporeal membrane oxygenation. Adv Exp Med Biol. 2013;765:203–9.
Robba C, Santori G, Czosnyka M, Corradi F, Citerio G. Optic nerve sheath diameter: the next steps. Intensive Care Med. 2019. https://doi.org/10.1007/s00134-019-05769-w.
Robba C, Cardim D, Czosnyka M, Abecasis F, Pezzato S, Buratti S, et al. Ultrasound non-invasive intracranial pressure assessment in paediatric neurocritical care: a pilot study. Childs Nerv Syst. 2019;36(1):117–24.
Funding
None.
Author information
Authors and Affiliations
Contributions
The study concept and design were given by NJ, PB, AC and PLL. Data acquisition was performed by NJ, EB, SP, AM, JML, AC, PB, MC and PS. Data analysis was performed by NJ, EB, MC and PS. NJ prepared the first draft of the manuscript. Interpretation of the data was done by NJ, EB, SP, AM, CR, JML, AC, PB, MC, PLL and PS. All authors provided critical feedback of the manuscript and approved the final version.
Corresponding author
Ethics declarations
Conflict of Interest
Joram has nothing to disclose. Beqiri has nothing to disclose. Pezzato has nothing to disclose. Moscatelli has nothing to disclose. Robba has nothing to disclose. Liet has nothing to disclose. Chenouard has nothing to disclose. Bourgoin has nothing to disclose. Czosnyka reports personal fees from Cambridge Enterprise Ltd, UK, during the conduct of the study. Léger has nothing to disclose. Smielewski reports and receives part of licensing fees for the brain monitoring software ICM+ (Cambridge Enterprise Ltd, Cambridge, UK) used in this project.
Ethical Approval/Informed Consent
The study was approved by the local Ethics Committees. Information of the parents was provided before inclusion.
Trial Registration
ClinicalTrials.gov (NCT04282525, February 21, 2020) https://clinicaltrials.gov/ct2/results?cond=&term=NCT04282525&cntry=&state=&city=&dist=
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original article has been updated to correct the author name Andrea Moscatelli.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12028_2020_1111_MOESM1_ESM.doc
Supplemental Digital Content-table 1. Autoregulation parameters during ECMO run according to the type of cannulation (DOC 39 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Joram, N., Beqiri, E., Pezzato, S. et al. Continuous Monitoring of Cerebral Autoregulation in Children Supported by Extracorporeal Membrane Oxygenation: A Pilot Study. Neurocrit Care 34, 935–945 (2021). https://doi.org/10.1007/s12028-020-01111-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-020-01111-1