Abstract
Background
Controversy surrounds utilization of induced hypothermia (IHT) in comatose cardiac arrest (CA) survivors with a non-shockable rhythm.
Methods
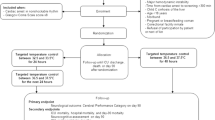
We conducted a meta-analysis and trial sequential analysis (TSA) comparing IHT with no IHT approaches in patients with CA and a non-shockable rhythm. The primary outcome of interest was favorable neurological outcomes (FNO) defined using the Cerebral Performance Category (CPC) score of 1 or 2. Secondary endpoints were survival at discharge and survival beyond 90 days.
Results
A total of 9 studies with 10,386 patients were included. There was no difference between both groups in terms of FNO (13% vs. 13%, RR 1.34, 95% CI 0.96–1.89, p = 0.09, I2 = 88%), survival at discharge (20% vs. 22%, RR 1.09, 95% CI 0.88–1.36, p = 0.42, I2 = 76%), or survival beyond 90 days (16% vs. 15%, RR 0.92, 95% CI 0.61–1.40, p = 0.69, I2 = 83%). The TSA showed firm evidence supporting the lack of benefit of IHT in terms of survival at discharge. However, the Z-curves failed to cross the conventional and TSA (futility) boundaries for FNO and survival beyond 90 days, indicating lack of sufficient evidence to draw firm conclusions regarding these outcomes.
Conclusion
In this meta-analysis of 9 studies, the utilization of IHT was not associated with a survival benefit at discharge. Although the meta-analysis showed lack of benefit of IHT in terms of FNO and survivals beyond 90 days, the corresponding TSA showed high probability of type-II statistical error, and therefore more randomized controlled trials powered for these outcomes are needed.





Similar content being viewed by others
References
Callaway CW, Donnino MW, Fink EL, et al. Part 8: post-cardiac arrest care: 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 Suppl 2):S465–82.
Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. New Engl J Med. 2002;346(8):549–56.
Bernard SA, Gray TW, Buist MD, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. New Engl J Med. 2002;346(8):557–63.
Hess EP, Campbell RL, White RD. Epidemiology, trends, and outcome of out-of-hospital cardiac arrest of non-cardiac origin. Resuscitation. 2007;72(2):200–6.
Frydland M, Kjaergaard J, Erlinge D, et al. Target temperature management of 33 °C and 36 °C in patients with out-of-hospital cardiac arrest with initial non-shockable rhythm: a TTM sub-study. Resuscitation. 2015;89:142–8.
Dumas F, Grimaldi D, Zuber B, et al. Is hypothermia after cardiac arrest effective in both shockable and nonshockable patients? Insights from a large registry. Circulation. 2011;123(8):877–86.
Testori C, Sterz F, Behringer W, et al. Mild therapeutic hypothermia is associated with favourable outcome in patients after cardiac arrest with non-shockable rhythms. Resuscitation. 2011;82(9):1162–7.
Vaahersalo J, Hiltunen P, Tiainen M, et al. Therapeutic hypothermia after out-of-hospital cardiac arrest in Finnish intensive care units: the FINNRESUSCI study. Intensive Care Med. 2013;39(5):826–37.
Mader TJ, Nathanson BH, Soares WE 3rd, Coute RA, McNally BF. Comparative effectiveness of therapeutic hypothermia after out-of-hospital cardiac arrest: insight from a large data registry. Ther Hypothermia Temp Manag. 2014;4(1):21–31.
Perman SM, Grossestreuer AV, Wiebe DJ, Carr BG, Abella BS, Gaieski DF. The utility of therapeutic hypothermia for post-cardiac arrest syndrome patients with an initial nonshockable rhythm. Circulation. 2015;132(22):2146–51.
Chan PS, Berg RA, Tang Y, Curtis LH, Spertus JA. Association between therapeutic hypothermia and survival after in-hospital cardiac arrest. JAMA. 2016;316(13):1375–82.
IntHout J, Ioannidis JP, Borm GF, Goeman JJ. Small studies are more heterogeneous than large ones: a meta-meta-analysis. J Clin Epidemiol. 2015;68(8):860–9.
Becker LB, Aufderheide TP, Geocadin RG, et al. Primary outcomes for resuscitation science studies: a consensus statement from the American Heart Association. Circulation. 2011;124(19):2158–77.
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Thorlund K, Devereaux PJ, Wetterslev J, et al. Can trial sequential monitoring boundaries reduce spurious inferences from meta-analyses? Int J Epidemiol. 2009;38(1):276–86.
Lascarrou JB, Merdji H, Le Gouge A, et al. Targeted temperature management for cardiac arrest with nonshockable rhythm. New Engl J Med. 2019;381:2327–37.
Khan MZ, Sulaiman S, Agrawal P, et al. Targeted temperature management in cardiac arrest patients with a non-shockable rhythm: a national perspective. Am Heart J. Epub 3 May 2020.
Dankiewicz J, Cronberg T, Lilja G, et al. Targeted hypothermia versus targeted Normothermia after out-of-hospital cardiac arrest (TTM2): a randomized clinical trial-Rationale and design. Am Heart J. 2019;217:23–31.
Vaagenes P, Ginsberg M, Ebmeyer U, et al. Cerebral resuscitation from cardiac arrest: pathophysiologic mechanisms. Crit Care Med. 1996;24(2 Suppl):S57–68.
Vaagenes P, Safar P, Moossy J, et al. Asphyxiation versus ventricular fibrillation cardiac arrest in dogs. Differences in cerebral resuscitation effects: a preliminary study. Resuscitation. 1997;35(1):41–52.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conception and design, analysis and interpretation of the data was done by MO and CB. Drafting of the article was done by MBM and SR. Provision of study materials or patients was done by MO, SR, BK and PA. Statistical expertise was done by MO and BK. Administrative, technical, or logistic support was done by CB, SB and PM. Collection and assembly of data was done by SR, PA and MBM. Critical revision of the article for important intellectual content and final approval of the article was done by all authors.
Corresponding author
Ethics declarations
Conflict of interest
All the author have no conflicts of interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Osman, M., Munir, M.B., Regner, S. et al. Induced Hypothermia in Patients with Cardiac Arrest and a Non-shockable Rhythm: Meta-analysis and Trial Sequential Analysis. Neurocrit Care 34, 279–286 (2021). https://doi.org/10.1007/s12028-020-01034-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-020-01034-x