Abstract
Background/Objective
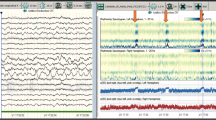
Simplified continuous electroencephalogram (cEEG) monitoring has shown improvement in detecting seizures; however, it is insufficient in detecting abnormal EEG patterns, such as periodic discharges (PDs), rhythmic delta activity (RDA), spikes and waves (SW), and continuous slow wave (CS), as well as nonconvulsive status epilepticus (NCSE). Headset-type continuous video EEG monitoring (HS-cv EEG monitoring; AE-120A EEG Headset™, Nihon Kohden, Tokyo, Japan) is a recently developed easy-to-use technology with eight channels. However, its ability to detect abnormal EEG patterns with raw EEG data has not been comprehensively evaluated. We aimed to examine the diagnostic accuracy of HS-cv EEG monitoring in detecting abnormal EEG patterns and NCSE in patients with altered mental status (AMS) with unknown etiology. We also evaluated the time required to initiate HS-cv EEG monitoring in these patients.
Methods
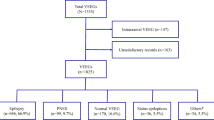
We prospectively observed and retrospectively examined patients who were admitted with AMS between January and December 2017 at the neurointensive care unit at Asakadai Central General Hospital, Saitama, Japan. We excluded patients whose data were missing for various reasons, such as difficulties in recording, and those whose consciousness had recovered between HS-cv EEG and conventional cEEG (C-cEEG) monitoring. For the included patients, we performed HS-cv EEG monitoring followed by C-cEEG monitoring. Definitive diagnosis was confirmed by C-cEEG monitoring with the international 10–20 system. As the primary outcome, we verified the sensitivity and specificity of HS-cv EEG monitoring in detecting abnormal EEG patterns including PDs, RDA, SW, and CS, in detecting the presence of PDs, and in detecting NCSE. As the secondary outcome, we calculated the time to initiate HS-cv EEG monitoring after making the decision.
Results
Fifty patients (76.9%) were included in the final analyses. The median age was 72 years, and 66% of the patients were male. The sensitivity and specificity of HS-cv EEG monitoring for detecting abnormal EEG patterns were 0.974 (0.865–0.999) and 0.909 (0.587–0.998), respectively, and for detecting PDs were 0.824 (0.566–0.926) and 0.970 (0.842–0.999), respectively. We diagnosed 13 (26%) patients with NCSE using HS-cv EEG monitoring and could detect NCSE with a sensitivity and specificity of 0.706 (0.440–0.897) and 0.970 (0.842–0.999), respectively. The median time needed to initiate HS-cv EEG was 57 min (5–142).
Conclusions
HS-cv EEG monitoring is highly reliable in detecting abnormal EEG patterns, with moderate reliability for PDs and NCSE, and rapidly initiates cEEG monitoring in patients with AMS with unknown etiology.




Similar content being viewed by others
References
Claassen J, Mayer SA, Kowalski RG, Emerson RG, Hirsch LJ. Detection of electrographic seizures with continuous EEG monitoring in critically ill patients. Neurology. 2004;62(10):1743–8.
DeLorenzo RJ, Waterhouse EJ, Towne AR, Boggs JG, Ko D, DeLorenzo GA, Brown A, Garnett L. Persistent nonconvulsive status epilepticus after the control of convulsive status epilepticus. Epilepsia. 1998;39(8):833–40.
Vespa PM, Nuwer MR, Nenov V, Ronne-Engstrom E, Hovda DA, Bergsneider M, Kelly DF, Martin NA, Becker DP. Increased incidence and impact of nonconvulsive and convulsive seizures after traumatic brain injury as detected by continuous electroencephalographic monitoring. J Neurosurg. 1999;91(5):750–60.
Towne AR, Waterhouse EJ, Boggs JG, Garnett LK, Brown AJ, Smith JR Jr, DeLorenzo RJ. Prevalence of nonconvulsive status epilepticus in comatose patients. Neurology. 2000;54(2):340–5.
Young GB, Doig GS. Continuous EEG monitoring in comatose intensive care patients: epileptiform activity in etiologically distinct groups. Neurocritical Care. 2005;2(1):5–10.
Alroughani R, Javidan M, Qasem A, Alotaibi N. Non-convulsive status epilepticus; the rate of occurrence in a general hospital. Seizure. 2009;18(1):38–42.
Gururangan K, Razavi B, Parvizi J. Utility of electroencephalography: experience from a U.S. tertiary care medical center. Clin Neurophysiol. 2016;127(10):3335–40.
Park A, Chapman M, McCredie VA, Debicki D, Gofton T, Norton L, Boyd JG. EEG utilization in Canadian intensive care units: a multicentre prospective observational study. Seizure. 2016;43:42–7.
Gavvala J, Abend N, LaRoche S, Hahn C, Herman ST, Claassen J, Macken M, Schuele S, Gerard E. Critical care EEG monitoring research consortium: continuous EEG monitoring: a survey of neurophysiologists and neurointensivists. Epilepsia. 2014;55(11):1864–71.
Hilkman DMW, van Mook W, Mess WH, van Kranen-Mastenbroek V. The use of continuous EEG monitoring in intensive care units in The Netherlands: a national survey. Neurocritical Care. 2018;29(2):195–202.
Brophy GM, Bell R, Claassen J, Alldredge B, Bleck TP, Glauser T, Laroche SM, Riviello JJ Jr, Shutter L, Sperling MR, et al. Guidelines for the evaluation and management of status epilepticus. Neurocritical Care. 2012;17(1):3–23.
Nitzschke R, Muller J, Engelhardt R, Schmidt GN. Single-channel amplitude integrated EEG recording for the identification of epileptic seizures by nonexpert physicians in the adult acute care setting. J Clin Monit Comput. 2011;25(5):329–37.
Young GB, Sharpe MD, Savard M, Al Thenayan E, Norton L, Davies-Schinkel C. Seizure detection with a commercially available bedside EEG monitor and the subhairline montage. Neurocritical Care. 2009;11(3):411–6.
Karakis I, Montouris GD, Otis JA, Douglass LM, Jonas R, Velez-Ruiz N, Wilford K, Espinosa PS. A quick and reliable EEG montage for the detection of seizures in the critical care setting. J Clin Neurophysiol. 2010;27(2):100–5.
Sutter R, Fuhr P, Grize L, Marsch S, Ruegg S. Continuous video-EEG monitoring increases detection rate of nonconvulsive status epilepticus in the ICU. Epilepsia. 2011;52(3):453–7.
Stewart CP, Otsubo H, Ochi A, Sharma R, Hutchison JS, Hahn CD. Seizure identification in the ICU using quantitative EEG displays. Neurology. 2010;75(17):1501–8.
Hirsch LJ, LaRoche SM, Gaspard N, Gerard E, Svoronos A, Herman ST, Mani R, Arif H, Jette N, Minazad Y, et al. American clinical neurophysiology society’s standardized critical care EEG terminology: 2012 version. J Clin Neurophysiol. 2013;30(1):1–27.
Zehtabchi S, Abdel Baki SG, Omurtag A, Sinert R, Chari G, Malhotra S, Weedon J, Fenton AA, Grant AC. Prevalence of non-convulsive seizure and other electroencephalographic abnormalities in ED patients with altered mental status. Am J Emerg Med. 2013;31(11):1578–82.
Kubota Y, Nakamoto H, Egawa S, Kawamata T. Continuous EEG monitoring in ICU. J Intensive Care. 2018;6:39.
Chong DJ, Hirsch LJ. Which EEG patterns warrant treatment in the critically ill? Reviewing the evidence for treatment of periodic epileptiform discharges and related patterns. J Clin Neurophysiol. 2005;22(2):79–91.
Leitinger M, Beniczky S, Rohracher A, Gardella E, Kalss G, Qerama E, Hofler J, Hess Lindberg-Larsen A, Kuchukhidze G, Dobesberger J, et al. Salzburg consensus criteria for non-convulsive status epilepticus-approach to clinical application. Epilepsy Behav. 2015;49:158–63.
Almojuela A, Hasen M, Zeiler FA. The full outline of unresponsiveness (FOUR) score and its use in outcome prediction: a scoping systematic review of the adult literature. Neurocritical Care. 2019;31(1):162–75.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48(3):452–8.
Varelas PN, Hacein-Bey L, Hether T, Terranova B, Spanaki MV. Emergent electroencephalogram in the intensive care unit: indications and diagnostic yield. Clin EEG Neurosci. 2004;35(4):173–80.
Leitinger M, Trinka E, Gardella E, Rohracher A, Kalss G, Qerama E, Hofler J, Hess A, Zimmermann G, Kuchukhidze G, et al. Diagnostic accuracy of the Salzburg EEG criteria for non-convulsive status epilepticus: a retrospective study. Lancet Neurol. 2016;15(10):1054–62.
Sen-Gupta I, Schuele SU, Macken MP, Kwasny MJ, Gerard EE. “Ictal” lateralized periodic discharges. Epilepsy Behav. 2014;36:165–70.
Kurtz P, Gaspard N, Wahl AS, Bauer RM, Hirsch LJ, Wunsch H, Claassen J. Continuous electroencephalography in a surgical intensive care unit. Intensive Care Med. 2014;40(2):228–34.
Rubinos C, Reynolds AS, Claassen J. The Ictal-interictal continuum: to treat or not to treat (and how)? Neurocritical Care. 2018;29(1):3–8.
Claassen J. How I treat patients with EEG patterns on the ictal-interictal continuum in the neuro ICU. Neurocritical Care. 2009;11(3):437–44.
Witsch J, Frey HP, Schmidt JM, Velazquez A, Falo CM, Reznik M, Roh D, Agarwal S, Park S, Connolly ES, et al. Electroencephalographic periodic discharges and frequency-dependent brain tissue hypoxia in acute brain injury. JAMA Neurol. 2017;74(3):301–9.
Laccheo I, Sonmezturk H, Bhatt AB, Tomycz L, Shi Y, Ringel M, DiCarlo G, Harris D, Barwise J, Abou-Khalil B, et al. Non-convulsive status epilepticus and non-convulsive seizures in neurological ICU patients. Neurocritical Care. 2015;22(2):202–11.
Rodriguez Ruiz A, Vlachy J, Lee JW, Gilmore EJ, Ayer T, Haider HA, Gaspard N, Ehrenberg JA, Tolchin B, Fantaneanu TA, et al. Association of periodic and rhythmic electroencephalographic patterns with seizures in critically ill patients. JAMA Neurol. 2017;74(2):181–8.
Gosavi TD, See SJ, Lim SH. Ictal and interictal EEG patterns in patients with nonconvulsive and subtle convulsive status epilepticus. Epilepsy Behav. 2015;49:263–7.
Funding
None.
Author information
Authors and Affiliations
Contributions
Satoshi Egawa and Toru Hifumi were responsible for conception of the article and drafted and revised the manuscript. Yuichi Kubota and Yasuhiro Kuroda helped to make a study design and draft the manuscript. Hidetoshi Nakamoto helped to draft the manuscript. All authors have read and approved the final manuscript and take full responsibility for all aspects of the study.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare a conflict of interest with Nihon Kohden as a cooperative research.
Ethical approval/informed consent
The protocol and consent procedures were approved by the Institutional Review Board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Egawa, S., Hifumi, T., Nakamoto, H. et al. Diagnostic Reliability of Headset-Type Continuous Video EEG Monitoring for Detection of ICU Patterns and NCSE in Patients with Altered Mental Status with Unknown Etiology. Neurocrit Care 32, 217–225 (2020). https://doi.org/10.1007/s12028-019-00863-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-019-00863-9