Abstract
Background
Global ischemia due to cardiac arrest (CA) followed by cardiopulmonary resuscitation (CPR) causes significant neuronal damage in vulnerable areas in the brain. Currently, a majority of patients eventually die after successful CPR due to neurological injury. Statins have pleiotropic effects including anti-inflammatory and/or antioxidant responses. These pleiotropic effects can have a beneficial role in the post-CPR phase. We tested whether two different types of statins, hydrophilic pravastatin and lipophilic simvastatin, attenuated neurological injury following CA/CPR. The efficacy of pravastatin and simvastatin combination treatment was also assessed.
Methods
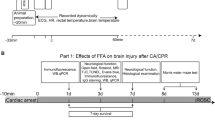
Isoflurane-anesthetized adult male wild-type C57Bl/6 mice subjected to 8-min CA/CPR were randomized into four groups: control, 2 mg/kg pravastatin, 20 mg/kg simvastatin, or a combination of 3 mg/kg pravastatin and 10 mg/kg simvastatin. Neurobehavioral assessment and histological analyses were performed to assess overall general health condition and neuronal injury, respectively.
Results
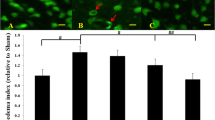
Combination treatment with pravastatin and simvastatin significantly reduced neuronal injury in the striatum and hippocampus, reduced cerebral edema, and improved general health at 4 days after CA/CPR. Combination statin treatment upregulated endothelial nitric oxide synthase mRNA in the brain. Pravastatin alone, but not simvastatin alone, improved general health after CA/CPR. Pravastatin was less potent than simvastatin at reducing neuronal injury in the brain.
Conclusion
Combination treatment with two different types of statins at the correct dose may be a promising approach to neuroprotection following CA/CPR.




Similar content being viewed by others
References
Laver S, Farrow C, Turner D, Nolan J. Mode of death after admission to an intensive care unit following cardiac arrest. Intensive Care Med. 2004;30(11):2126–8.
Neumar RW, Nolan JP, Adrie C, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; and the Stroke Council. Circulation. 2008;118(23):2452–83.
Safar P, Behringer W, Bottiger BW, Sterz F. Cerebral resuscitation potentials for cardiac arrest. Crit Care Med. 2002;30(4 Suppl):S140–4.
White BC, Sullivan JM, DeGracia DJ, et al. Brain ischemia and reperfusion: molecular mechanisms of neuronal injury. J Neurol Sci. 2000;179(S 1–2):1–33.
Dragancea I, Rundgren M, Englund E, Friberg H, Cronberg T. The influence of induced hypothermia and delayed prognostication on the mode of death after cardiac arrest. Resuscitation. 2013;84(3):337–42.
Adrie C, Haouache H, Saleh M, et al. An underrecognized source of organ donors: patients with brain death after successfully resuscitated cardiac arrest. Intensive Care Med. 2008;34(1):132–7.
Newman CB, Preiss D, Tobert JA, et al. Statin safety and associated adverse events: a scientific statement from the American Heart Association. Arterioscler Thromb Vasc Biol. 2019;39(2):e38–81.
Oesterle A, Laufs U, Liao JK. Pleiotropic effects of statins on the cardiovascular system. Circ Res. 2017;120(1):229–43.
Davignon J. Beneficial cardiovascular pleiotropic effects of statins. Circulation. 2004;109(23 Suppl 1):III39–43.
Schachter M. Chemical, pharmacokinetic and pharmacodynamic properties of statins: an update. Fundam Clin Pharmacol. 2005;19(1):117–25.
Garcia-Bonilla L, Campos M, Giralt D, et al. Evidence for the efficacy of statins in animal stroke models: a meta-analysis. J Neurochem. 2012;122(2):233–43.
Wood WG, Eckert GP, Igbavboa U, Muller WE. Statins and neuroprotection: a prescription to move the field forward. Ann N Y Acad Sci. 2010;1199:69–76.
Nezasa K, Higaki K, Takeuchi M, Nakano M, Koike M. Uptake of rosuvastatin by isolated rat hepatocytes: comparison with pravastatin. Xenobiotica. 2003;33(4):379–88.
Carone D, Librizzi L, Cattalini A, et al. Pravastatin acute neuroprotective effects depend on blood brain barrier integrity in experimental cerebral ischemia. Brain Res. 2015;1615:31–41.
Nakano T, Hurn PD, Herson PS, Traystman RJ. Testosterone exacerbates neuronal damage following cardiac arrest and cardiopulmonary resuscitation in mouse. Brain Res. 2010;1357:124–30.
Kofler J, Hattori K, Sawada M, et al. Histopathological and behavioral characterization of a novel model of cardiac arrest and cardiopulmonary resuscitation in mice. J Neurosci Methods. 2004;136(1):33–44.
Allen D, Nakayama S, Kuroiwa M, et al. SK2 channels are neuroprotective for ischemia-induced neuronal cell death. J Cereb Blood Flow Metab. 2011;31(12):2302–12.
Zeynalov E, Chen CH, Froehner SC, et al. The perivascular pool of aquaporin-4 mediates the effect of osmotherapy in postischemic cerebral edema. Crit Care Med. 2008;36(9):2634–40.
Taguchi N, Nakayama S, Tanaka M. Fluoxetine has neuroprotective effects after cardiac arrest and cardiopulmonary resuscitation in mouse. Resuscitation. 2012;83(5):652–6.
Laufs U, La Fata V, Plutzky J, Liao JK. Upregulation of endothelial nitric oxide synthase by HMG CoA reductase inhibitors. Circulation. 1998;97(12):1129–35.
Vaughan CJ, Murphy MB, Buckley BM. Statins do more than just lower cholesterol. Lancet. 1996;348(9034):1079–82.
Gauthier TW, Scalia R, Murohara T, Guo JP, Lefer AM. Nitric oxide protects against leukocyte-endothelium interactions in the early stages of hypercholesterolemia. Arterioscler Thromb Vasc Biol. 1995;15(10):1652–9.
van den Brule JMD, van der Hoeven JG, Hoedemaekers CWE. Cerebral perfusion and cerebral autoregulation after cardiac arrest. Biomed Res Int. 2018;2018:4143636.
Huang Z, Huang PL, Ma J, et al. Enlarged infarcts in endothelial nitric oxide synthase knockout mice are attenuated by nitro-l-arginine. J Cereb Blood Flow Metab. 1996;16(5):981–7.
Endres M, Laufs U, Huang Z, et al. Stroke protection by 3-hydroxy-3-methylglutaryl (HMG)-CoA reductase inhibitors mediated by endothelial nitric oxide synthase. Proc Natl Acad Sci USA. 1998;95(15):8880–5.
Laufs U, Liao JK. Post-transcriptional regulation of endothelial nitric oxide synthase mRNA stability by Rho GTPase. J Biol Chem. 1998;273(37):24266–71.
Kureishi Y, Luo Z, Shiojima I, et al. The HMG-CoA reductase inhibitor simvastatin activates the protein kinase Akt and promotes angiogenesis in normocholesterolemic animals. Nat Med. 2000;6(9):1004–10.
Rezaie-Majd A, Maca T, Bucek RA, et al. Simvastatin reduces expression of cytokines interleukin-6, interleukin-8, and monocyte chemoattractant protein-1 in circulating monocytes from hypercholesterolemic patients. Arterioscler Thromb Vasc Biol. 2002;22(7):1194–9.
Paumelle R, Blanquart C, Briand O, et al. Acute antiinflammatory properties of statins involve peroxisome proliferator-activated receptor-alpha via inhibition of the protein kinase C signaling pathway. Circ Res. 2006;98(3):361–9.
Vasilikos L, Spilgies LM, Knop J, Wong WW. Regulating the balance between necroptosis, apoptosis and inflammation by inhibitors of apoptosis proteins. Immunol Cell Biol. 2017;95(2):160–5.
Barone FC, Arvin B, White RF, et al. Tumor necrosis factor-alpha. A mediator of focal ischemic brain injury. Stroke. 1997;28(6):1233–44.
Cui D, Shang H, Zhang X, Jiang W, Jia X. Cardiac arrest triggers hippocampal neuronal death through autophagic and apoptotic pathways. Sci Rep. 2016;6:27642.
Sheng H, Laskowitz DT, Pearlstein RD, Warner DS. Characterization of a recovery global cerebral ischemia model in the mouse. J Neurosci Methods. 1999;88(1):103–9.
Karki K, Knight RA, Han Y, et al. Simvastatin and atorvastatin improve neurological outcome after experimental intracerebral hemorrhage. Stroke. 2009;40(10):3384–9.
Ryu JH, Park JW, Hwang JY, et al. The attenuation of neurological injury from the use of simvastatin after spinal cord ischemia-reperfusion injury in rats. BMC Anesthesiol. 2018;18(1):31.
Marz P, Otten U, Miserez AR. Statins induce differentiation and cell death in neurons and astroglia. Glia. 2007;55(1):1–12.
Wood WG, Igbavboa U, Muller WE, Eckert GP. Statins, Bcl-2, and apoptosis: cell death or cell protection? Mol Neurobiol. 2013;48(2):308–14.
Kiener PA, Davis PM, Murray JL, et al. Stimulation of inflammatory responses in vitro and in vivo by lipophilic HMG-CoA reductase inhibitors. Int Immunopharmacol. 2001;1(1):105–18.
Qiu Y, Wu Y, Meng M, et al. Rosuvastatin improves myocardial and neurological outcomes after asphyxial cardiac arrest and cardiopulmonary resuscitation in rats. Biomed Pharmacother. 2017;87:503–8.
Bergt S, Grub A, Wagner S, et al. Pravastatin but not simvastatin improves survival and neurofunctional outcome after cardiac arrest and cardiopulmonary resuscitation. JACC Basic Transl Sci. 2017;2(2):149–59.
Funding
This study was supported by JSPS KAKENHI Grant Number 26462743.
Author information
Authors and Affiliations
Contributions
SN designed the study and prepared the protocol. SN, TN, YI, and NT performed experiments. MT contributed to critical revision of the manuscript. SN drafted and revised the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interests.
Ethical approval
The University of Tsukuba Subcommittee on Research Animal Care approved this study (protocol no. 15-125, 16-112).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nakayama, S., Taguchi, N., Isaka, Y. et al. Combined Treatment with Hydrophilic and Lipophilic Statins Improves Neurological Outcomes Following Experimental Cardiac Arrest in Mice. Neurocrit Care 33, 64–72 (2020). https://doi.org/10.1007/s12028-019-00862-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-019-00862-w