Abstract
Background
Management of refractory status epilepticus (SE) commonly involves the induction of burst suppression using intravenous anesthetic agents. However, the endpoints of these therapies are not well defined. Weaning anesthetic agents are complicated by the emergence of electroencephalogram (EEG) patterns along the ictal–interictal continuum (IIC), which have uncertain significance given that IIC patterns may worsen cerebral metabolism and oxygenation, have a dissociation between scalp and depth EEG recordings, or may indicate a late stage of SE itself. Determining the significance of IIC patterns in the unique context of anesthetic weaning is important to prevent the potential for unnecessarily prolonging anesthetic coma.
Methods
Among 118 individuals with SE, we retrospectively identified a series of patients who underwent at least 24 h of burst-suppression therapy, experienced two or more weaning trials, and developed IIC patterns during anesthetic weaning. Anesthetic titration strategies during the emergence of these patterns were examined.
Results
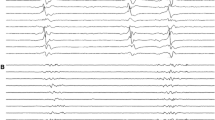
Each of the six individuals who met inclusion criteria experienced aggressive weaning despite the emergence of IIC patterns. The IIC patterns that were encountered during anesthetic weaning (including generalized and lateralized periodic discharges) are described in detail. Favorable outcomes were reported in each subject.
Conclusion
IIC patterns encountered during anesthetic weaning may be transitional and warrant observation, allowing for the emergence of more definitive clinical or electrographic results. The metabolic impact of these IIC patterns on brain activity is uncertain, but weaning strategies that treat IIC as a surrogate of recurrent SE risk further prolonging anesthetic management and its known toxicity. We speculate that these patterns may have a context-specific association with SE relapse, with less-risk conferred when these patterns are observed during the weaning of anesthetic agents after prolonged burst-suppression therapy. Other electrographic features aside from this clinical context may discriminate the risk of SE relapse, such as EEG background activity.







Similar content being viewed by others
References
Bleck TP. Refractory status epilepticus. Curr Opin Crit Care. 2005;11(2):117–20.
Holtkamp M. Treatment strategies for refractory status epilepticus. Curr Opin Crit Care. 2011;17(2):94–100.
Novy J, Logroscino G, Rossetti AO. Refractory status epilepticus: a prospective observational study. Epilepsia. 2010;51(2):251–6.
Mayer SA, Claassen J, Lokin J, Mendelsohn F, Dennis LJ, Fitzsimmons B-F. Refractory status epilepticus: frequency, risk factors, and impact on outcome. Arch Neurol. 2002;59(2):205–10.
Holtkamp M, Othman J, Buchheim K, Meierkord H. Predictors and prognosis of refractory status epilepticus treated in a neurological intensive care unit. J Neurol Neurosurg Psychiatry. 2005;76(4):534–9.
Rossetti AO, Lowenstein DH. Management of refractory status epilepticus in adults: still more questions than answers. Lancet Neurol. 2011;10(10):922–30.
Brophy GM, Bell R, Claassen J, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17(1):3–23.
Shorvon S, Ferlisi M. The treatment of super-refractory status epilepticus: a critical review of available therapies and a clinical treatment protocol. Brain. 2011;134(10):2802–18.
Shorvon S, Trinka E. The London–Innsbruck Status epilepticus colloquia 2007–2011, and the main advances in the topic of status epilepticus over this period. Epilepsia. 2013;54:11–3.
Johnson EL, Martinez NC, Ritzl EK. EEG characteristics of successful burst suppression for refractory status epilepticus. Neurocrit Care. 2016;25(3):407–14.
Thompson SA, Hantus S. Highly epileptiform bursts are associated with seizure recurrence. J Clin Neurophysiol. 2016;33(1):66–71.
Hocker SE, Britton JW, Mandrekar JN, Wijdicks EFM, Rabinstein AA. Predictors of outcome in refractory status epilepticus. JAMA Neurol. 2013;70(1):72–7.
Krishnamurthy KB, Drislane FW. Depth of EEG suppression and outcome in barbiturate anesthetic treatment for refractory status epilepticus. Epilepsia. 1999;40(6):759–62.
Rossetti AO, Logroscino G, Bromfield EB. Refractory status epilepticus. Arch Neurol. 2005;62(11):1698–702.
Krishnamurthy KB, Drislane FW. Relapse and survival after barbiturate anesthetic treatment of refractory status epilepticus. Epilepsia. 1996;37(9):863–7.
Struck AF, Westover MB, Hall LT, Deck GM, Cole AJ, Rosenthal ES. Metabolic correlates of the ictal–interictal continuum: FDG-PET during continuous EEG. Neurocrit Care. 2016;24(3):324–31.
Treiman DM, Walton NY, Kendrick C. A progressive sequence of electroencephalographic changes during generalized convulsive status epilepticus. Epilepsy Res. 1990;5(1):49–60.
Chong DJ, Hirsch LJ. Which EEG patterns warrant treatment in the critically ill? Reviewing the evidence for treatment of periodic epileptiform discharges and related patterns. J Clin Neurophysiol. 2005;22(2):79–91.
Johnson EL, Kaplan PW. Population of the ictal–interictal zone: the significance of periodic and rhythmic activity. Clin Neurophysiol Pract. 2017;2:107–18.
Sivaraju A, Gilmore EJ. Understanding and managing the ictal–interictal continuum in neurocritical care. Curr Treat Options Neurol. 2016;18(2):8.
Claassen J, How I. Treat patients with EEG patterns on the ictal–interictal continuum in the neuro ICU. Neurocrit Care. 2009;11(3):437–44.
Rossetti AO, Oddo M. The neuro-ICU patient and electroencephalography paroxysms: if and when to treat. Curr Opin Crit Care. 2010;16(2):105–9.
Bauer G, Trinka E. Nonconvulsive status epilepticus and coma. Epilepsia. 2010;51(2):177–90.
Funding
The authors did not receive any funding for this manuscript.
Author information
Authors and Affiliations
Contributions
Author Contributions
ASD conceived the project, designed the study, acquired and analyzed the data, and drafted the manuscript. JWL acquired and analyzed the data and revised the manuscript. ESR designed the study, helped with data analysis and revised the manuscript. HV conceived the project, designed the study, acquired and analyzed the data, and revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This study was conducted according to our institution’s guidelines for ethical research. The patient database used in this study was approved by our institutional review board.
Rights and permissions
About this article
Cite this article
Das, A.S., Lee, J.W., Rosenthal, E.S. et al. Successful Wean Despite Emergence of Ictal–Interictal EEG Patterns During the Weaning of Prolonged Burst-Suppression Therapy for Super-Refractory Status Epilepticus. Neurocrit Care 29, 452–462 (2018). https://doi.org/10.1007/s12028-018-0552-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-018-0552-6