Abstract
Background
Adequate identification of the severity of status epilepticus (SE) contributes to individualized treatment. The scales most widely used for this purpose are: Status Epilepticus Severity Score (STESS), Epidemiology-Based Mortality Score in Status Epilepticus (EMSE) and modified Rankin Scale STESS (mRSTESS). The aim of this study was to evaluate the performance of the STESS, EMSE and mRSTESS scales to predict high disability and hospital mortality at discharge (HD/HM).
Methods
A prospective study was conducted in which total of 41 patients were registered from November 2015 to January 2018 at Eugenio Espejo Hospital. Clinical variables such as age, sex, clinical status at the beginning of the SE, initial symptom of SE, as well as the STESS, mRSTESS and EMSE variant scales were studied at the time of the diagnosis of SE.
Results
A total of 41 patients were evaluated, of which 8 (19.5%) had HD at hospital discharge and died 13 (31.7%) during their care. The area under the receiver operating characteristic curve to predict HD/HM was 0.71 (95% CI (confidence interval) 0.55–0.87), 0.81 (95% CI 0.67–0.94), 0.89 (95% CI 0.79–0.99), 0.90 (95% CI 0.80–1.0), 0.89 (95% CI 0.78–0.99) for the STESS, mRSTESS, EMSE-EAC (etiology, age, comorbidities), EMSE-EACEG (etiology, age, comorbidities, electroencephalography) and EMSE-ECLEG (etiology, age, level of consciousness at pre-treatment, electroencephalography), variants of EMSE, respectively. The binary logistic regression demonstrated how the following cut-off points were determined: STESS OR (odd ratio) 4.80 (p = 0.02), mRSTESS OR 7.89 (p = 0.00), EMSE-EAC OR 22.16 (p = 0.00), EMSE-ECLEG OR 18.00 (p = 0.00), EMSE-EACEG OR 14 (p = 0.00).
Conclusions
All of the evaluated scales (STESS, mRSTESS, and EMSE) were shown to be useful in predicting HD/HM. EMSE was observed to be the most effective of the scales, with relative similarities among the variants.
Similar content being viewed by others
Introduction
Status epilepticus (SE) is a frequent neurological emergency, with high morbidity and mortality. In population studies for SE, mortality ranges between 7.6 and 39% [1]. The final outcome of these patients depends on multiple factors, one of which includes the evaluation of severity at the time of diagnosis. The adequate identification of the severity of SE contributes greatly to individualized treatment that can minimize risks of overtreatment and unnecessary prolongation of sedation and stay in the intensive care unit (ICU). Additionally, prediction of the severity is also imperative as to avoid underdiagnosis, as the lack of intensity of adequate treatment may also introduce harmful outcomes.
With this objective, various scales have been described that permit the identification of patients with greater severity and, consequently, with more risk of HD/HM. The most widely used are: Status Epilepticus Severity Score (STESS), Epidemiology-Based Mortality Score in Status Epilepticus (EMSE), and more recently the modified Rankin Scale STESS (mRSTESS), of which includes the introduction of an additional variable, the Rankin Scale [5].
All of these scales were created and evaluated in European populations, with few studies evaluating the scales within Asian and Latin American populations [6, 7].
Previous studies exist evaluating and comparing the STESS and EMSE scales; however, these studies do not include the mRSTESS. It is necessary to identify the performance of the these three scales in our particular environment, one in which therapeutic limitations exist due to the lack of new antiepileptic drugs, second line treatment of SE, and diagnostic because of the inability to provide continuous electroencephalographic neuromonitoring.
We proposed to carry out the present work to evaluate the performance of these scales in our given environment as to predict HD/HM, as well as validate the effectiveness of these scales in our Ecuadorian patients.
Methods
A study was conducted with the variables collected prospectively, and the analysis performed retrospectively, in our database from November 2015 to January 2018 at Eugenio Espejo Hospital, the main public health-care center in Quito, Ecuador. The objective of this research was to evaluate the performance of the STESS, EMSE, and mRSTESS scales that predict HD/HM at hospital discharge, as well as to validate these scales in our Ecuadorian patients.
All patients diagnosed with SE and treated during the aforementioned period were included. Convulsive SE was defined according to the most recent International League Against Epilepsy classifications (ILAE) [8] and non-convulsive SE according to the Salzburg criteria [9]. Clinical variables such as age, sex, clinical status at the beginning of the SE (according to the Glasgow Scale), [10] initial symptom of SE, as well as the STESS, mRSTESS, and EMSE variant scales were studied [4, 5] at the time of the diagnosis of SE. The etiology was evaluated according to the guidelines of the ILAE [11]. All patients were evaluated with the Rankin Scale [5] at hospital discharge, with grades 4 and 5 recorded as HD. Patients who died during their hospitalization were also registered (Rankin grade 6). Informed consent was requested of patients or their relatives in instances of altered judgment or impaired level of consciousness of the patient. The personal data of all patients was protected.
Analysis
The patients were divided into two groups: the first including patients with favorable outcome (Rankin grades 0–3) and the second including patients with HD at hospital discharge (Rankin grades 4–5) and HM (Rankin grade 6) during hospitalization. A univariate analysis was performed in which the Chi-squared and the Fisher’s test were used for qualitative variables and the Student’s t test for the quantitative variables. The receiver operating characteristic (ROC) curve was used to determine the sensitivity and specificity of the STESS, mRSTESS, and EMSE scales. The Youden’s index was used to identify the best cutoff point for optimized sensitivity and specificity of each scale, and the positive and negative predictive values for each one were calculated. Finally, a logistic regression was carried out to determine the predictive capacity of the cutoff points established for each scale.
Results
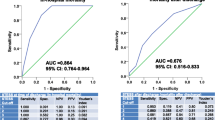
A total of 41 patients were evaluated, of which 21 (51.2%) had HD at hospital discharge (8, 19.5%) or died (13, 31.7%) during their care. In the univariate analysis (Table 1), patients with HD/HM at discharge had STESS, EMSE, and mRSTESS scores significantly higher compared to the rest. The area under the ROC curve to predict HD/HM was 0.71 (95% confidence interval (CI) 0.55–0.87), 0.81 (95% CI 0.67–0.94), 0.89 (95% CI 0.79–0.99), 0.90 (95% CI 0.80–1.0), 0.89 (95% CI 0.78–0.99) for the STESS, mRSTESS, EMSE-EAC (etiology, age, comorbidities), EMSE-EACEG (etiology, age, comorbidities, electroencephalography), and EMSE-ECLEG (etiology, age, level of consciousness at pre-treatment, electroencephalography), respectively (Figs. 1, 2). The results demonstrated good performance for all scales; however, EMSE demonstrated relatively better accuracy. The cutoff point that showed the best efficacy (Table 2) was 3 for STESS (sensitivity 0.76, specificity 0.60, positive predictive value 0.71, negative predictive value 0.67), 4 for mRSTESS (sensitivity 0.81, specificity 0.65, positive predictive value 0.77, negative predictive value 0.71), 40 for the EMSE-EAC (sensitivity 0.91, specificity 0.75, positive predictive value 0.87, negative predictive value 0.76), 72 for EMSE-ECLEG (sensitivity 0.86, specificity 0.70, positive predictive value 0.82, negative predictive value 0.75), and 74 for EMSE-EACEG (sensitivity 0.86, specificity 0.75, positive predictive value 0.83, negative predictive value 0.78). The binary logistic regression (Table 3) showed how the established cutoff points were found for STESS odds ratio (OR) 4.80 (95% CI 1.25–18.42, p = 0.02), for mRSTESS OR 7.89 (95% CI 1.89–32.81, p = 0.00), while for the different EMSE variants were as follows: EAC OR 22.16 (95% CI 3.88–126.65, p = 0.00), ECLEG OR 18.00 (95% CI − 3.68–87.99, p = 0.00) and EACEG OR 14 (95% CI 2.96–66.08, p = 0.00).
Discussion
SE is a neurological emergency with high morbidity and mortality. In the present study, mortality reached 31.7%, a result consistent with previous findings [1, 7]. However, the group with HD/HM represented 51.2% of all patients, highlighting the clinical severity of these cases. Few studies exist that address the residual sequelae following SE. Of the studies that do exist, predominantly motor and functional sequelae for activities of daily life are evaluated, excluding cognitive sequelae, which persist as an unclear aspect of SE that has been seldom studied. Previous research has found that between 11 and 23% of patients who survive a SE present some residual disability, similar to these results in which 19.5% had subsequent sequelae [12]. Other authors have found that almost half of patients have some type of disability at hospital discharge [6, 13]. The discrepancy in these findings is suspected to be a result of variations of the definition ‘disability,’ an issue in which other authors have already acknowledged themselves [12, 13]. There is no standard that clearly defines disability following SE and distinguishes between motor, cognitive, and impairments in performing daily activities so that the term may be uniformly understood. Therefore, a consensus as to how to evaluate disability, both motor and functional in daily and cognitive life, should be established. Designing a tool that allows this to be carried out in a uniform manner would be an important objective for future studies.
Clinical status at the beginning of the SE was another factor that was associated with HD/HM. Initial clinical status was measured using the Glasgow Scale. Patients that demonstrated alteration in level of consciousness or epileptic seizure associated with subsequent deterioration of the state of consciousness (low scores on the Glasgow Scale) had significantly worse outcome than the rest of the patients in the univariate analysis. Similar results initially described by Rossetti and other studies also observed this outcome [14, 15].
The scores of the different scales were also significantly higher for patients with HD and who died during their hospitalization. The sensitivity analysis according to the ROC curve showed that all the scales had good sensitivity to predict HD/HM. For the STESS, the area under the curve was 0.71, with a cutoff point of 3, a sensitivity of 0.76 and a specificity of 0.60. Results were consistent with the initial evaluations of this scale [2, 16]; however, other studies found better efficacy with STESS to predict HM in patients with scores greater than 4 points [6, 7, 17]. It has been suggested that the prognostic assessment of STESS for patients over 65 years old with prior epilepsy is overestimated, while patients with impaired level of consciousness without non-convulsive epileptic status (focal epileptic motor status in coma) may be underestimated [3, 18]. This study was characterized by the average age being > 65 years old and with the majority of SE diagnoses ensue from complications of other brain conditions. Additionally, this study evaluated the predictive capacity of both HD/HM, not exclusively HM. These differences are suspected to explain the differences in cutoff points between this study and other studies performed.
mRSTESS, a recently introduced prognostic scale, includes modifications such as increasing the age cutoff to 70 and the addition of the Rankin Scale. This scale has only been evaluated in one previous report and was compared with STESS, showing superiority in the prognosis of HM. In the present study, similar results were obtained, but as a predictor of HD/HM. The cutoff point with the highest sensitivity–specificity efficiency was 4, in concordance to the Gonzalez-Cuevas et al. [4]. In this scale, a preponderant value is attributed to the state of the patient at the beginning of the diagnosis of SE; patients are evaluated at two separate points of the scale, once during the evaluation of the level of consciousness and thereafter when evaluated using the Rankin Scale (functional evaluation), which at the author’s discretion better represents the clinical state of the patients.
Regarding the EMSE scale, the variants (EMSE-EAC, EMSE-ECLEG, EMSE-EACEG) predicted, with better efficiency, HD/HM in our patients. Sensitivity values found were analogous to those found in the initial description of this scale [4], and subsequent research was carried out with the objective of determining the ability of the EMSE-EACEG ≥ 64 to predict mortality and HD at 30 days. The sensitivity was greater than 80%, [19] being superior to the STESS with this objective. Moreover, the sensitivity and specificity values of this study were higher than those of other studies (AUROC 70–80%) [6, 7]. Undoubtedly, good specificity holds higher importance during prognosis and when predicting poor outcome, further supporting the superiority of the EMSE over STESS.
In this study, it was also observed that the cutoff points identified as most optimal were higher than in previous studies [6, 7], which is suspected to be related to the etiology of the SE in these patients; most of them experienced SE as a consequence of cerebrovascular diseases, metabolic, or septic alterations. Multiple comorbidities were also presented, the most common being septic. Other evidence of the comparably higher cutoff points was the high score for EMSE-EAC when compared with previous works. It was shown that scores above 40 were the best predictors of disability and mortality. Previous studies placed this value at 27 and 37 [3, 6, 7]. In Argentina, a country of our same geographic area, scores higher than 37 for the EMSE-EAC and 64 for the EMSE-EACEG had a higher specificity of 90% [7].
Undoubtedly, etiology and comorbidity have a significant impact on the final outcome of the patients treated in this study. In general, all the variants of the EMSE scale showed good efficacy, with relatively equivalent parameters. Notably, the cutoff point determined in this study, (74 for EMSE-EACEG) was higher than previously reported studies (64 and 62) [3, 6]. This is suspected to be a result of the aforementioned characteristics of the study.
The EMSE scale has been shown to provide superior results in predicting the outcome of patients with SE due to the inclusion of additional variables that have offered a more holistic evaluation of the patients at the time of diagnosis. The authors recognize that overlap exists among the CIs between the scales, primarily a result of the small sample size. Another factor that may have contributed to this overlap was the cutoff point, obtained by the ROC curve, that was optimized for the application of the logistic regression curves.
Although the EMSE scale has advantages over the other scales, due to the additional variables, the evaluation process requires more analysis in comparison with STESS and mRSTESS. Both the STESS and the mRSTESS only require clinical evaluation of the patient, whereas the EMSE scale requires additional complimentary tests. However, overall, the application of all scales is not complicated and offers valuable insight in the prediction of patient outcome. There are few studies that have evaluated the prognostic scales in patients with SE; therefore, new studies would contribute greatly in the determination of the best combination of factors used for evaluation. Unfortunately for the region of Latin and South America, there are few studies that have described the effectiveness of these tools.
Nevertheless, the application of these scales serves as a valuable tool to evaluate prognosis of SE given circumstances of insufficient resources, such as limited access to neuromonitoring or prolonged transport time. The scales are useful in guiding medical professionals to identify optimal intensity of treatment and furthermore, avoid over- or under-treatment, ultimately to prevent unnecessary stay in the ICU.
Conclusions
All scales evaluated, STESS, mRSTESS, and EMSE, were shown to be useful in predicting HD and in-HM. EMSE was superior to the rest of the scales, with relative similarity between its variants for scores higher than 40, 72, and 74 in EMSE-EAC, EMSE-ECLEG, and EMSE-EACEG, respectively, in Ecuadorian patients from Eugenio Espejo Hospital.
For future studies, it would be interesting to analyze the effectiveness of the scales to evaluate good outcome in patients with the given circumstances in order to have a more holistic evaluation of the scales.
Limitations
The main limitation of this study was the small sample size analyzed. The evaluation was limited to the prognostic scales, but factors such as treatment, refractoriness, and duration of the SE were not taken into account. Additionally, most of our patients had acute symptomatic causes, which could favor the EMSE scale because it is the only one that includes this variable.
References
Neligan A, Shorvon SD. Frequency and prognosis of convulsive status epilepticus of different causes: a systematic review. Arch Neurol. 2010;67:931–40.
Rossetti AO, Logroscino G, Bromfield EB. A clinical score for prognosis of status epilepticus. Neurology. 2006;66:1736–8.
Leitinger M, Holler Y, Kalss G, Rohracher A, Novak HF, Hofler J, et al. Epidemiology-based mortality score in status epilepticus (EMSE). Neurocrit Care. 2015;22:273–82.
González-Cuevas M, Santamarina E, Toledo M, Quintana M, Sala J, Sueiras M, et al. A new clinical score for the prognosis of status epilepticus in adults. Eur J Neurol. 2016;23(10):1534–40.
Rankin J. Cerebral vascular accidents in patients over the age of 60. II. Prognosis. Scott Med J. 1957;2(5):200–15.
Kang BS, Kim DW, Kim KK, Moon HJ, Kim YS, Kim HK, et al. Prediction of mortality and functional outcome from status epilepticus and independent external validation of STESS and EMSE scores. Crit Care. 2016;20:25.
Pacha MS, Orellana L, Silva E, Ernst G, Pantiu F, Quiroga Narvaez J, et al. Role of EMSE and STESS scores in the outcome evaluation of status epilepticus. Epilepsy Behav. 2016;64(Pt A):140–2.
Trinka E, Cock H, Hesdorffer D, Rossetti AO, Scheffer IE, Shinnar S, et al. A definition and classification of status epilepticus—report of the ILAE Task Force on Classification of Status Epilepticus. Epilepsia. 2015;56(10):1515–23.
Leitinger M, Beniczky S, Rohracher A, Gardella E, Kalss G, Qerama E, et al. Salzburg consensus criteria for non-convulsive status epilepticus—approach to clinical application. Epilepsy Behav. 2015;49:158–63.
Teasdale G, Jennett B. Assessment of impaired consciousness and coma: a practical scale. Lancet. 1974;13–2(7872):81–4.
Commission on Epidemiology and Prognosis, International League Against Epilepsy. Guidelines for epidemiologic studies on epilepsy. Epilepsia. 1993;34:592–6.
Claassen J, Lokin JK, Fitzsimmons BF, Mendelsohn FA, Mayer SA. Predictors of functional disability and mortality after status epilepticus. Neurology. 2002;58(1):139–42.
Belluzzo M, Furlanis G, Stragapede L. Predictors of functional disability at hospital discharge after status epilepticus. Epilepsy Res. 2015;110:179–82.
Rossetti AO, Hurwitz S, Logroscino G, Bromfield EB. Prognosis of status epilepticus: role of aetiology, age, and consciousness impairment at presentation. J Neurol Neurosurg Psychiatry. 2006;77(5):611–5.
Chin RF, Neville BG, Scott RC. A systematic review of the epidemiology of status epilepticus. Eur J Neurol. 2004;11(12):800–10.
Rossetti AO, Logroscino G, Milligan TA, Michaelides C, Ruffieux C, Bromfield EB. Status Epilepticus Severity Score (STESS): a tool to orient early treatment strategy. J Neurol. 2008;255(10):1561–6.
Sutter R, Kaplan PW, Rüegg S. Independent external validation of the status epilepticus severity score. Crit Care Med. 2013;41(12):e475–9.
Leitinger M, Kalss G, Rohracher A, Pilz G, Novak H, Höfler J, Deak I, et al. Predicting outcome of status epilepticus. Epilepsy Behav. 2015;49:126–30.
Giovannini G, Monti G, Tondelli M, Marudi A, Valzania F, Leitinger M, et al. Mortality, morbidity and refractoriness prediction in status epilepticus: comparison of STESS and EMSE scores. Seizure. 2017;46:31–7.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
DRR designed the study, collected and processed the data, performed the statistical analyses, and drafted the manuscript. CSM participated in treatment of the patients, collected the data, and reviewed the final manuscript. KS drafted the manuscript and performed the analysis of the results. DDS participated in treatment of the patients, collected the data, and reviewed the final manuscript. NMS obtained institutional permissions to carry out the study, participated in treatment of the patients, and reviewed the final manuscript. YP performed the statistical analyses.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare there were no conflicts of interest.
Ethical Approval
The execution and publication of this study was approved by the ethical committee of the institution.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Rivero Rodríguez, D., Scherle Matamoros, C., Sam, K. et al. Evaluation of STESS, mRSTESS, and EMSE to Predict High Disability and Mortality at Hospital Discharge in Ecuadorian Patients with Status Epilepticus. Neurocrit Care 29, 413–418 (2018). https://doi.org/10.1007/s12028-018-0549-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-018-0549-1