Abstract
Background
Chikungunya fever is a globally spreading mosquito-borne disease that shows an unexpected neurovirulence. Even though the neurological complications have been a major cause of intensive care unit admission and death, to date, there is no systematic analysis of their spectrum available.
Objective
To review evidence of neurological manifestations in Chikungunya fever and map their epidemiology, clinical spectrum, pathomechanisms, diagnostics, therapies and outcomes.
Methods
Case report and systematic review of the literature followed established guidelines. All cases found were assessed using a 5-step clinical diagnostic algorithm assigning categories A–C, category A representing the highest level of quality. Only A and B cases were considered for further analysis. After general analysis, cases were clustered according to geospatial criteria for subgroup analysis.
Results
Thirty-six of 1196 studies were included, yielding 130 cases. Nine were ranked as category A (diagnosis of Neuro-Chikungunya probable), 55 as B (plausible), and 51 as C (disputable). In 15 cases, alternative diagnoses were more likely. Patient age distribution was bimodal with a mean of 49 years and a second peak in infants. Fifty percent of the cases occurred in patients <45 years with no reported comorbidity. Frequent diagnoses were encephalitis, optic neuropathy, neuroretinitis, and Guillain–Barré syndrome. Neurologic conditions showing characteristics of a direct viral pathomechanism showed a peak in infants and a second one in elder patients, and complications and neurologic sequelae were more frequent in these groups. Autoimmune-mediated conditions appeared mainly in patients over 20 years and tended to show longer latencies and better outcomes. Geospatial subgrouping of case reports from either India or Réunion revealed diverging phenotypic trends (Réunion: 88% direct viral vs. India: 81% autoimmune).
Conclusions
Direct viral forms of Neuro-Chikungunya seem to occur particularly in infants and elderly patients, while autoimmune forms have to be also considered in middle-aged, previously healthy patients, especially after an asymptomatic interval. This knowledge will help to identify future Neuro-Chikungunya cases and to improve outcome especially in autoimmune-mediated conditions. The genetics of Chikungunya virus might play a key role in determining the course of neuropathogenesis. With further research, this could prove diagnostically significant.
Similar content being viewed by others
Introduction
Chikungunya fever (CHIKF) is a mosquito-borne disease caused by the Chikungunya virus (CHIKV), a RNA virus first described in 1952 in today’s Tanzania [1]. Until recently, CHIKF was regarded as a non-fatal disease restricted to Africa and Asia, marked by fever, polyarthralgia and rash [2,3,4]. However, the last decade brought forth a “new face” of CHIKF due to: (1) The “Asian tiger mosquito” Aedes (Ae.) albopictus spreading to the Indian Ocean, South America, Europe and the USA [5]. (2) The spread of a new CHIKV strain, probably from Kenya in the early 2000s, to the Indian Ocean [6]. There it met up with Ae. Albopictus and underwent an adapting mutation that boosted the transmission by the new vector [7, 8], causing major epidemics with thousands of cases [9]. (3) Increased air travel exporting CHIKV to other countries and possibly provoking autochthonous transmission by local Aedes populations [10, 11]. This has happened to a limited extent in Italy, France and the USA, while CHIKV has spread to 45 countries in Central/South America since 2013, resulting in another 1.7 million suspected cases [12,13,14,15]. The resulting upsurge of cases is likely the reason for an accumulation of life-threatening complications, suggesting CHIKF as a potentially fatal disease that may cause broad systemic involvement (Fig. 1).
Possible disease courses of CHIKF. According to Economopoulou et al. [16], severe atypical CHIKF is defined as the patient needing support of at least 1 vital function (such as mechanical ventilation). Further sources are manifestation rate [3, 4, 9], chronic arthralgia [28–32], atypical and severe cases, and death [16, 17, 33–37]
Thereby, neurological complications take center stage. Accounting for up to 25% of atypical cases and up to 60% of severe atypical cases, they are a major cause of intensive care unit admission and death in CHIKF [16, 17]. Reports range from encephalitis, optic neuritis, myeloradiculitis to Guillain–Barré syndrome (GBS), causing drastic sequelae such as mental disability, blindness and persisting paralysis—also in young and previously healthy persons [18,19,20,21,22,23,24,25,26]. In many cases, neurological signs start after a symptom-free interval of 1–3 weeks, pointing to an autoimmune process [21,22,23,24,25,26]. Given the challenge of this variety and the forecast that CHIKF will continue its spread to more temperate regions such as the USA and Europe in the future [27], neurologists should be aware of the typical aspects of Neuro-Chikungunya.
To our knowledge, no systematic analysis of neurological complications in CHIKF has been published to date. Nor is there a critical appraisal of the evidence in individual case reports. Therefore, we performed a systematic review of all published cases, combined with a case report assessment. The aim was to assess the possible clinical spectrum of neurological involvement regarding patient age and origin, comorbidity and time from disease onset, and to review the diagnostics, therapies, pathomechanisms, encountered complications and outcomes of Neuro-Chikungunya.
.
Case Report
A 74-year-old man with hypertension, dyslipidemia and suspended nicotine abuse experienced fever, arthralgia and rash while on holiday in Tahiti. Symptoms disappeared within 48 h. On 7th day of illness (DOI), he noticed hypoesthesia of the hands and gait difficulties. The following morning, he could not walk and suffered from hoarseness, dyspnoea and, finally, loss of consciousness. Paramedics discovered ventricular tachycardia, which was reversed by defibrillation. After hospital transfer, he was intubated and ventilated due to respiratory insufficiency. Cranio-thoracic computed tomography yielded no findings. Laboratory findings were unspecific. Electrocardiography abnormalities called for a coronary angiography and stenting of the left anterior descending artery. Magnetic resonance imaging (MRI) scan showed diffusion-weighted imaging (DWI) restrictions in the pons, and the electroencephalography (EEG) revealed an “alpha coma.” After sedation was discontinued, the patient remained unresponsive and brainstem reflexes were absent. Severe hypoxic encephalopathy due to cardiac arrest was suspected and palliative strategy recommended. However, perceiving him as being responsive, the patient’s wife insisted on full life-sustaining measures and repatriation.
Upon admission to the Neurocritical Care Unit, University Hospital Zurich, on 21st DOI, the patient presented with multiple cranial nerve palsies (complete ophthalmoplegia, facial diplegia, absence of corneal/gag reflex, swallowing and tongue movements), flaccid tetraplegia and areflexia. However, basic communication was possible through head movements. MRI reevaluation suggested rhombencephalitis. Cerebrospinal fluid (CSF) examination revealed cytoalbuminologic dissociation and intrathecal synthesis of IgM/IgA with oligoclonal bands in CSF and serum. CSF glucose and lactate levels were normal, and microbiology CSF microbiology was negative, as was PCR for herpes simplex 1/2 and varicella zoster viruses. Serum tested negative for T. pallidum, B. burgdorferi, human immunodeficiency virus, hepatitis B/C, tick-borne encephalitis and human herpes viruses 1–5. Serum tested positive for anti-CHIKV-IgM and IgG and for anti-dengue IgG. Search for paraneoplastic, anti-ganglioside and anti-myelin associated glycoprotein antibodies was negative. EEG showed minor generalized alterations without epileptiform potentials. An electroneuromyography (ENMG) objectified severe distally accentuated axonal polyneuropathy. Taken together, the diagnosis of a Bickerstaff’s brainstem encephalitis (BBE)-Miller Fisher syndrome (MFS)-GBS-overlap was retained. After a 1-week plateau, the patient deteriorated prompting therapy with IV immunoglobulins on 33rd DOI. The patient regained control over swallowing and eye movements but non-verbal communication did not return to previous levels. Follow-up MRI revealed progressive rhombencephalitis (Fig. 2a–c). Negative CHIKV rtPCR from serum and CSF reinforced the assumption of an autoimmune pathomechanism, prompting therapy with IV methylprednisolone on 51st DOI, leading to a gradual improvement of alertness and patient transfer to a neurorehabilitation center. After 4 months, motor function of proximal limbs improved to muscle grade 2/5. One year after onset ventilation could be switched to non-invasive ventilator support. The latest follow-up—1.5 years after onset—showed normal mental status and cranial nerve function, but persisting, distally accentuated hypaesthesia and paresis of limbs with near complete palsy of hands and feet. For detailed case information see appendix 1.
MRI on 38th DOI showing progress of rhombencephalitis from pons up to the left thalamus and internal capsule. a Axial fluid-attenuated inversion recovery (FLAIR) MRI showing hyperintensities in predominantly left pontomesencephalic junction, b sagittal FLAIR showing hyperintensities in lower thalamus, mesencephalon, pons and cerebellar peduncle, c Axial T2W-tse MRI showing hyperintensities in left thalamus
Systematic Review
Methods
A systematic review was performed, following the “preferred reporting items for systematic reviews and meta-analyses” (PRISMA) guidelines [38]. Appendix 2 contains the review protocol. Publications had to meet all following criteria: (1) patients with confirmed CHIKV infection showing neurological symptoms; (2) CHIKV infection confirmed by presence of viral RNA, specific IgM or fourfold increase in IgG titers in serum or CSF [9]; (3) peer-reviewed case report/series, observational study or scientific letter; (4) data provided for each patient, enabling verification of diagnosis; and (5) case occurred after 2000. Cases were excluded if any of the following applied: (1) confirmed concurrent infection such as malaria, dengue or zika fever; (2) vaccination one month prior to symptom onset; (3) isolated paresthesias of hands (CHIKV-mediated carpal tunnel syndrome); and/or (4) children with simple febrile seizure only.
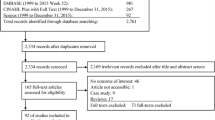
We searched MEDLINE (through PUBMED and OVID), EMBASE, WEB OF SCIENCE and SCOPUS from January 1, 2000, to December 1, 2015, combining “Chikungunya” and a broad list of neurological conditions, using both index terms and free text, proximity operators, and truncation symbols. No further limits were applied. For complete search strategy, see appendix 2. Applying the predefined eligibility criteria, the records were screened by TC as shown in the PRISMA scheme in appendix 3.
Data extraction into a pilot tested data file was performed twice (by TC), with an interval of two months. For coding rules, see appendix 2. Authors were contacted if case similarity suggested double counting, or if data were missing or ambiguously stated (both coded as missing). The quality of the included cases was assessed by a clinical diagnostic decision tree (see appendix 4) using extracted data items and two new criteria assessed for each case report: A) are clinical signs consistent with the diagnosis? B) are other etiologies sufficiently excluded? To answer these questions consistently, a list of relevant neurological diagnoses was defined using the National Library of Medicine’s Medical Subject Headings-Thesaurus, UpToDate and relevant literature (appendix 2). The answers were added to the general data extraction sheet. This allowed the entire decision tree to be programmed as an algorithm, which assigned the cases to the quality categories A, B and C (see appendix 4). After assignment, each case was reviewed manually for algorithm adherence. Statistical analysis was performed using IBM©-SPSS©-software (version 22).
Results
Description of Studies and Case Report Assessment
A total of 1196 records were screened (see appendix 3). Thirty-six articles were included in the systematic review, comprising 131 patients (nine redundant cases were excluded). All authors were contacted for missing data. Twenty-one replied, supplying data for 51 cases and prompting the exclusion of two further cases. After adding the abovementioned case report, the total case number was 130.
All were assessed for quality using the algorithm in appendix 4. In 15 cases, clinical signs were inconsistent with the obtained diagnosis or alternative diagnoses were more likely. Of the remaining 115 cases, nine qualified as category A (probable Neuro-Chikungunya case), 55 as B (plausible) and 51 as C (disputable). Due to weak evidence level of category C, only A and B cases were used for further analysis (Tab. 1). The A cases are described in appendix 5.
Patient Characteristics
Patient age distribution of the 64 A and B cases approached a bell-shaped curve spanning from 20 to 80 years, with a second peak in infants/children. In adults, mean age was 49 years (median 48, SD = 17). The sex ratio was 41% females to 59% males. Patient comorbidity was 25%, most frequently due to cardiovascular problems (32%) and diabetes (25%). 50% (32/64) of cases occurred in younger patients (<45 years) with no reported comorbidity.
Clinical Presentation of Neuro-Chikungunya
Neurological symptoms were preceded by classical CHIKF symptoms: fever in 98%, arthralgia in 71% and rash in 45%; complete triad was present in 36%. Neurological symptoms started on average 10 days (d) after initial symptom onset (median 7, range 1–53). However, the corresponding histogram revealed a two peaks trend in latency; encephalitis accounting for the first peak (mean 3.5 days), neuro-ophthalmological diagnoses accounting for the second (mean 23.2 days). Time between initial symptoms and GBS onset varied from very short (2 days), through short (7, 8 days) to long (14, 19 days). Nineteen percent (12/64) of the patients were asymptomatic between initial symptoms and neurological complaints.
Frequent diagnoses were encephalitis, optic neuropathy, neuroretinitis, and GBS (Table 1). Encephalitis (N = 27) was marked by altered mental status (100%) and fever (96%), accompanied by seizures (52%) and focal neurological deficits (56%), e.g., paresis of limbs, asymmetrical hypertonia, pyramidal signs, or myoclonus. Two cases showed marked brainstem involvement (appendix 6). Optic neuropathy (N = 18) presented with defective vision and relative afferent pupillary defect. Sixteen cases were subdiagnosed as papillitis: three showing involvement of other cranial nerves, two as retrobulbar neuritis, and one showing bilateral external ophthalmoplegia, facial palsy, hemiparesis, and unconsciousness (appendix 7). GBS (N = 5) presented with distally accentuated quadriparesis and hypo-/areflexia, more pronounced in lower limbs, accompanied by facial palsy in all five cases (3/5 bilateral).
Diagnostics
Serum tested positive for CHIKV infection in all 64 cases, and CSF tested positive in 31/33 cases. In encephalitis, serum rtPCR was positive in 65% (13/20) and IgM in 77% (17/22), while in CSF, rtPCR was positive in 62% (13/21) and IgM in 80% (12/15). In GBS, rtPCR was typically negative and IgM positive (serum and CSF). In acute disseminated encephalomyelopathy, optic neuropathy, and neuroretinitis, serum IgM was positive and rtPCR negative, where tested. CSF basic biochemistry was pathological in 77% (N = 35); in encephalitis it frequently showed transudative (39%, 9/23) or exsudative CSF syndrome (26%, 6/23). The typical CSF syndrome in GBS was cytoalbuminological dissociation (80%, 4/5; for definitions see appendix 5). MRI was performed in 42/64 cases; in encephalitis it was pathologic in 83% (10/12). ENMG was performed in all GBS-MFS cases and showed a demyelinating (2/6) or combined axonal/demyelinating pattern (4/6).
Suspected Pathomechanism, Therapy, Complications and Outcome
Depending on the treating physicians’ assumption of the underlying pathomechanism (direct viral vs. autoimmune), therapies were either purely symptomatic (40%) or also immunosuppressive (60%). Figure 3 summarizes the epidemiological and clinical aspects of the two groups. While assumingly direct viral forms showed a peak in infants (and a second one in elder patients), autoimmune forms occurred almost exclusively in patients over 20 years, with a peak in the middle-aged. Encephalitis therapy was mainly symptomatic (23/27), whereas all cases of optic neuropathy, neuroretinitis and ADEM were treated with steroids with good (66%) or partial response (33%). GBS spectrum cases were treated with steroids, ivIG or both, with varying responses.
Suspected pathomechanisms according to the physicians’ treatment. ADEM Acute disseminated encephalomyelitis, BBE Bickerstaff’s brainstem encephalitis, GBS Guillain–Barré syndrome, MFS Miller Fisher syndrome, mRS modified Rankin scale, SD Standard deviation. ªTreatment known in 60 cases. °Data available for 15 viral cases and 21 autoimmune cases. Moderate complications: altered level of consciousness, seizure, need for intubation. Severe complications: respiratory failure, cardiovascular instability, sepsis, intracranial hypertension
Fifty-eight percent (37/64) of cases developed complications, mainly altered level of consciousness (49%), seizure (18%), need for intubation (18%). In 20%, they were severe, e.g., respiratory failure (N = 10), cardiovascular instability (N = 5), sepsis (N = 3) or intracranial hypertension (N = 2). Cumulation of complications was observed in the very young and the elderly and in central nervous system (CNS) affections. Outcome at last follow-up was full recovery in 29%, partial recovery in 50%, no recovery in 10%, and death in 11%. According to the modified Rankin scale (mRS), results were: the modified Rankin scale (mRS): no significant disability (mRS 0–1) in 43%, slight to moderate disability (mRS 2–3) in 29%, and moderately severe to severe disability (mRS 4–5) in 15%. Death occurred in seven cases due to neurological damage (N = 4) or other organ decompensation (N = 2, cause unclear in 1 case). A cumulation of severe outcomes was observed in children and elderly (mRS ≥4 in 83% of patients <12 years and in 58% of patients >65 years vs. 0–11% in other age groups) and in CNS affections (mRS ≥4 in 46% vs. 4% in peripheral forms). Cases with suspected autoimmune pathomechanism showed better outcome than cases with suspected direct viral pathomechanism (Fig. 3).
Phenotypic Trends in Outbreak-Specific Subgroups
We categorized the case reports into six outbreak subgroups: Réunion (2005–2006), India (2006-present), Italy (2007), Thailand (2009), the Caribbean (2013–2014), and Pacific Islands (2011–2015). Showing the largest number of case reports (see map in appendix 8) and a more or less even representation of all age groups, Réunion and India were chosen for further analysis. Comparison of CHIKV action in these subgroups revealed a stark distinction: while 88% of the Réunion cases suffered from an assumingly direct viral pathomechanism, the majority from India (82%) suffered from possibly autoimmune-mediated conditions. This correlated with the neurological site affected (Réunion: 78% central nervous system (CNS) affection vs. India: 69% peripheral nervous system (PNS) affection). Concerning patient outcome, no disability (mRS = 0) was the most frequent outcome in Réunion (42%) and India (50%); however, second commonest outcome in India was slight disability (mRS = 2, 25%) versus death in Réunion (mRS = 6, 21%).
Discussion
This review confirms Neuro-Chikungunya as a severe form of CHIKF. Age distribution was bimodal with a mean at 49 years and a second peak in infants. Fifty percent of cases occurred in younger patients (<45 years) with no reported comorbidity. Neurological symptoms were usually preceded by fever and arthralgia, with two latency peaks. Frequent diagnoses were encephalitis, optic neuropathy, neuroretinitis and GBS, less frequent ADEM and combined encephalomyeloradiculopathies. Autoimmune-connoted diagnoses were seen mainly in patients over 20 years and tended to show longer latencies and better outcomes. Complications and adverse outcomes were more frequent in children and elderly and in CNS affections.
The strength of this study is its systematic analysis of Neuro-Chikungunya cases published between 2000 and 2015, including an in-depth assessment of each reported diagnosis. Thus, 51% (66/130) of cases were excluded due to weak evidence for a causality between CHIKV infection and neurological symptoms (category C, see appendix 9 for frequent pitfalls). Nevertheless, this retrospective review has its limitations, as the case mix is probably distorted by publication bias, thus requiring comparison with larger-scale observational field studies.
While hospital-based studies of neurological complications during epidemics (Réunion 2005/06, India 2006) suggest a preponderance of (mostly encephalitic) CNS affections in elderly with comorbidities (44–57%) [17, 39, 40], we found a bimodal age distribution with a peak in the middle-aged and a second one in the very young. There are two possible explanations. First, our study may show an overrepresentation of autoimmune-connoted diagnoses such as GBS and optic neuropathies; these patients tended to be younger and healthier. Likewise, a recent series on CHIKV-associated GBS found a mean of 48 years and 33% comorbidity [41]. Secondly, our study contains some pediatric cases, which account for the peak in the very young. Indeed, a large study on CHIKV encephalitis during the Réunion outbreak found the highest incidence rates among the youngest and oldest (38% <1 years and 38% >65 years) [18]. Neonates constitute a major risk group for Neuro-Chikungunya: in perinatally infected women, vertical transmission rates of up to 50% were observed, leading to neurological symptoms and neurodevelopmental delay in up to 50% of infected neonates [42,43,44]. In short, the epidemiology of Neuro-Chikungunya might be summarized by three overlapping paradigms:
-
1.
Peak of CNS affections in neonates and infants
-
2.
Peak of autoimmune, often PNS affections in middle-aged
-
3.
Peak of CNS affections in elderly with comorbidities.
Regarding clinical aspects of Neuro-Chikungunya, field studies report similar findings: fever (91–100%) and arthralgia (83–100%) are frequent precursors, while rash is rarer (25–44%) [18, 39, 40]. Encephalitis generally starts in this acute phase of CHIKF, while GBS tends to occur subacutely, after a symptom-free interval [18, 39,40,41]. Either way, fever and arthralgia followed by neurological symptoms may indicate Neuro-Chikungunya in (travelers from) endemic areas. Concerning detection of CHIKV in Neuro-Chikungunya, our findings are in line with the “rule of thumb” for general CHIKF: serum rtPCR sensitive up to 7 DOI, IgM ELISA starting from 3 to 4 DOI [3]. Reported CSF changes in 61–85% (77% in our review) suggest that CSF biochemistry is useful, although CSF changes seem to be less frequent in children [18]. The need for early (<7 days) DWI-weighted MRI is stressed, as other modalities lack sufficient sensitivity [18, 39, 40]. Nerve conduction studies are decisive in recognizing peripheral nerve affection, especially if cranial neuropathies mimic central damage [45]. The average rate of severe complications in Neuro-Chikungunya is confirmed to be ~20%; the need for intensive care support in encephalitis is reportedly higher (42%, N = 24) [18]. This corresponds to our finding; complications were more frequent in the youngest and elderly, the main encephalitis targets. Figures on outcome in Neuro-Chikungunya report no sequelae in ~45%, persisting disability in ~35% and death in ~20% [17, 18, 39]. In our review, we saw more disability (44% mRS 2–5) and less mortality (11%), possibly due to the overrepresentation of autoimmune-mediated conditions.
For clinical practice, it is key to consider the pathomechanism involved in Neuro-Chikungunya cases. Basic research points toward at least two paradigms: a direct viral and an autoimmune one. A direct viral CNS infection is increasingly demonstrated. In mice with deficient interferon (IFN) signaling, CHIKV crosses the choroid plexus and infects the meninges and ependyma, thereby possibly affecting underlying neuronal cells or even the stem cell niche [46,47,48]. In vitro, CHIKV infects mouse brain neurons, astrocytes and oligodendrocytes, causing apoptosis in the first two [49]. Additionally, astrocytes produce IFN and proapoptotic factors, possibly causing further bystander damage and disrupting the blood–brain-barrier [49, 50]. These findings are assigned to human neonates and elderly people due to their weaker innate and adaptive immune response [46, 48]. This is supported by a high rate (92%) of CHIKV rtPCR positivity in infected neonates’ CSF and short latency between initial CHIKF signs and encephalitic symptoms [39, 40, 44]. The direct viral mechanism suggests the clinical use of neutralizing antibodies in neonates born to CHIK-viremic mothers and development of vaccines and antiviral drugs on astrocyte level [50].
An autoimmune response triggered by CHIKV seems probable, as numerous cases show longer latency between initial signs and neurological symptoms and respond to immunosuppressants. Furthermore, the autoimmune nature of some diseases observed in CHIKF is increasingly recognized. GBS, MFS and BBE have been proposed recently to form one broad spectrum with a common autoimmune pathomechanism. After infection with certain pathogens, autoantibodies are formed due to molecular mimicry between the pathogen and nerve tracts [51]. These antibodies are either directed against the myelin sheath of Schwann-cells (antigen unknown), causing demyelination and slowing of nerve conduction, or against gangliosides located in the node of Ranvier, causing intermittent conduction blocks and, with time, persistent axonal damage [52]. This can be linked to CHIKV by two arguments: 1) there has been a rise in GBS incidence during CHIKV epidemics in La Réunion and French Polynesia [41, 53]; 2) anti-ganglioside antibodies were found in CHIKV-associated GBS cases [41]. However, Neuro-Chikungunya cases with documented anti-ganglioside antibody screening remain scarce, while the screening itself is subject to some uncertainties [52]. Besides, proving molecular mimicry would require deciphering the CHIKV structure mimicking neural structures [54]. Nevertheless, we suggest considering CHIKV as a possible trigger for autoimmune-mediated neurological conditions, especially for all GBS-MFS-subtypes as classified by Wakerley et al. [51]. Thus, even less familiar forms might be recognized and treated in time.
Proposing two paradigms of Neuro-Chikungunya pathogenesis (direct viral CNS infection with short latency vs. autoimmune PNS affection with longer latency), two caveats are necessary. First, short latency can be autoimmune, although autoimmune-connoted cases tended to have longer latencies, one GBS case showed a latency of only two days [26]. This might be due to reactivation, as recurring GBS tends toward shorter latency [55]. Therefore, short latency does not rule out an autoimmune-mediated disease. Second, central can be autoimmune, although autoimmune-connoted cases tended to show peripheral nerve affection, there were three cases of suspected autoimmune brainstem encephalitis responding to immunosuppressants (case report, appendix 6) and three ADEM cases, an illness generally considered autoimmune-mediated [56]. Thus, central affections in CHIKF should also be matched against possible autoimmune-mediated conditions.
By analyzing the geographic and temporal origins of the case reports, we wanted to determine whether the genetic and antigenic landscapes of CHIKV play a role in its neuropathogenesis. Phylogenetic analysis of CHIKV indicates three distinct genotype groups: West African, ECSA (East, Central and South African) and Asian [2, 57]. Indeed, sequence analysis of the envelope glycoprotein 1 (E1) region of the CHIKV genome revealed a sequence similarity of only 78% between isolates of the West African and the ECSA and Asian genotypes [2]. CHIKV not only exhibits genetic heterogeneity, but studies reported that isolates also have distinct antigenic phenotypes [2, 57].
Interestingly, further analysis of Réunion and India cases revealed diverging clinical and pathogenetic phenotypes. Most patients from Réunion showed signs of a likely direct neurotoxic pathomechanism, while patients from India those of an autoimmune one. This is mirrored by predominantly CNS affection in Réunion cases compared to mainly PNS affection in India cases. Hypothetically, this might be due to adaptive mutations being accumulated by the virus during outbreak, pushing it (incidentally) in a direct neurotoxic or neuroautoimmune direction. Indeed, an analysis of the microevolution of CHIKV during the Réunion outbreak showed that the virus—though most closely related to the ECSA genotype—underwent nucleotide and amino acid changes, resulting in an epidemic strain genetically different from the initial strain. Most prominently, a mutation (A226V) in the E1 glycoprotein occurred, probably as a result of CHIKV adaptation to its new vector, Ae. Albopictus [7, 20, 58]. This microevolution could account for the abundance of atypical and neuropathogenic cases emerging during the outbreak.
Another study used in vivo infection of mice with the ECSA versus Asian strain comparing their neurovirulence. While the strains were similarly neuroinfectious, the Asian group showed higher mortality rates and higher apoptosis gene expression, while the ECSA group showed upregulation of genes involved in CNS protection [59].
Overall, the genetics of CHIKV could be of clinical relevance once the genetic elements that contribute to neurovirulence are understood. The abovementioned comparisons suggest the possibility to characterize CHIKV neuropathogenesis based on strain specificity, which could help to choose among treatment options in cases of Neuro-Chikungunya.
To this end, mapping mutations during outbreaks and their effect on CHIKF manifestation as well as improving our knowledge on CHIKV genetics in general is imperative.
Conclusions
Neuro-Chikungunya is a severe form of CHIKF with a broad spectrum. Fever and arthralgia followed by neurological symptoms may indicate Neuro-Chikungunya in travelers from endemic areas. Direct viral CNS infections with short latencies are seen in infants and in elderly with comorbidities, while autoimmune-mediated conditions have also to be considered in middle-aged, previously healthy patients, especially after an asymptomatic interval. Careful attention is required to discern direct viral from autoimmune conditions: while short latency and CNS affection suggest a direct viral pathomechanism, autoimmune conditions have been observed in these situations, too. Adverse outcomes occur especially in infants and elderly with direct viral CNS affection. By contrast, outcome seems better in cases with suspected autoimmune pathomechanism and use of immunosuppressants. Geospatial and temporal clustering of case reports revealed diverging phenotypic patterns, suggesting that strain-specific genetics may play a diagnostically relevant role in disease pathomechanism and course. To confirm these emerging trends and provide better evidence for causality between CHIKV infection and neurotoxicity/-autoimmunity, it is time to move from case reports/series and epidemiological correlations to case–control studies and randomized control trials.
Abbreviations
- Ae:
-
Aedes (a genus of mosquitoes)
- ADEM:
-
Acute disseminated encephalomyelopathy
- BBE:
-
Bickerstaff’s brainstem encephalitis
- CHIKF:
-
Chikungunya fever
- CHIKV:
-
Chikungunya virus
- d:
-
Days
- DOI:
-
Day of illness
- DWI:
-
Diffusion-weighted imaging
- ECSA:
-
East, Central, and South African
- ENMG:
-
Electroneuromyography
- GBS:
-
Guillain–Barré syndrome
- IFN:
-
Interferon
- MFS:
-
Miller Fisher syndrome
- mRS:
-
Modified Rankin scale
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- rtPCR:
-
Reverse transcription Polymerase chain reaction
- y:
-
Years
References
Robinson MC. An epidemic of virus disease in Southern Province, Tanganyika Territory, in 1952-53. I. Clinical features. Trans R Soc Trop Med Hyg. 1955;49:28–32.
Powers AM, Brault AC, Tesh RB, Weaver SC. Re-emergence of Chikungunya and O’nyong-nyong viruses: evidence for distinct geographical lineages and distant evolutionary relationships. J Gen Virol. 2000;81:471–9.
Weaver SC, Lecuit M. Chikungunya virus and the global spread of a mosquito-borne disease. N Engl J Med. 2015;372:1231–9.
Thiberville S-D, Moyen N, Dupuis-Maguiraga L, et al. Chikungunya fever: epidemiology, clinical syndrome, pathogenesis and therapy. Antiviral Res. 2013;99:345–70.
Enserink M. Entomology. A mosquito goes global. Science. 2008;320:864–6.
Lo Presti A, Ciccozzi M, Cella E, et al. Origin, evolution, and phylogeography of recent epidemic CHIKV strains. Infect Genet Evol J Mole Epidemiol Evol Genet Infect Dis. 2012;12:392–8.
Schuffenecker I, Iteman I, Michault A, et al. Genome microevolution of chikungunya viruses causing the Indian Ocean outbreak. PLoS Med. 2006;3:1058–70.
Tsetsarkin KA, Vanlandingham DL, McGee CE, Higgs S. A single mutation in chikungunya virus affects vector specificity and epidemic potential. PLoS Pathog. 2007;3:e201.
Burt FJ, Rolph MS, Rulli NE, Mahalingam S, Heise MT. Chikungunya: a re-emerging virus. Lancet. 2012;379:662–71.
Panning M, Grywna K, van Esbroeck M, Emmerich P, Drosten C. Chikungunya fever in travelers returning to Europe from the Indian Ocean region, 2006. Emerg Infect Dis. 2008;14:416–22.
Lanciotti RS, Kosoy OL, Laven JJ, et al. Chikungunya virus in US travelers returning from India, 2006. Emerg Infect Dis. 2007;13:764–7.
Rezza G, Nicoletti L, Angelini R, et al. Infection with chikungunya virus in Italy: an outbreak in a temperate region. Lancet. 2007;370:1840–6.
Delisle E, Rousseau C, Broche B, et al. Chikungunya outbreak in Montpellier, France, September to October 2014. Euro Surveill. 2015;20:21108.
Centers for Disease Control and Prevention (2015) Chikungunya Virus: Geographic Distribution. http://www.cdc.gov/chikungunya/geo/index.html. Accessed 15 Feb 2016.
Centers for Disease Control and Prevention (2014) Chikungunya virus in the United States: 2014 final data for the United States. http://www.cdc.gov/chikungunya/geo/united-states-2014.html. Accessed 15 Feb 2016.
Economopoulou A, Dominguez M, Helynck B, et al. Atypical Chikungunya virus infections: clinical manifestations, mortality and risk factors for severe disease during the 2005–2006 outbreak on Reunion. Epidemiol Infect. 2009;137:534–41.
Tandale BV, Sathe PS, Arankalle VA, et al. Systemic involvements and fatalities during Chikungunya epidemic in India, 2006. J Clin Virol. 2009;46:145–9.
Gerardin P, Couderc T, Bintner M, et al. Chikungunya virus–associated encephalitis: a cohort study on La Reunion Island, 2005–2009. Neurology. 2016;86:94–102.
Nelson J, Waggoner JJ, Sahoo MK, Grant PM, Pinsky BA. Encephalitis caused by Chikungunya virus in a traveler from the Kingdom of Tonga. J Clin Microbiol. 2014;52:3459–61.
Chusri S, Siripaitoon P, Hirunpat S, Silpapojakul K. Short report: case reports of neuro-chikungunya in southern Thailand. Am J Trop Med Hyg. 2011;85:386–9.
Gauri LA, Ranwa BL, Nagar K, Vyas A, Fatima Q. Post chikungunya Brain stem encephalitis. J Assoc Phys India. 2012;60:68–9.
Das S, Sarkar N, Majumder J, Chatterjee K, Aich B. Acute disseminated encephalomyelitis in a child with chikungunya virus infection. J Pediatr Infect Dis. 2014;9:37–41.
Mohite AA, Agius-Fernandez A. Chikungunya fever presenting with acute optic neuropathy. BMJ Case Rep 2015;2015.
Mittal A, Mittal S, Bharati J, Ramakrishnan R, Saravanan S, Sathe PS. Optic neuritis associated with chikungunya virus infection in South India. Arch Ophthalmol. 2007;125:1381–6.
Bank AM, Batra A, Colorado RA, Lyons JL. Myeloradiculopathy associated with chikungunya virus infection. J Neurovirol. 2016;22:125–8.
Wielanek AC, Monredon JD, Amrani ME, Roger JC, Serveaux JP. Guillain–Barré syndrome complicating a Chikungunya virus infection. Neurology. 2007;69:2105–7.
Fischer D, Thomas SM, Suk JE, et al. Climate change effects on Chikungunya transmission in Europe: geospatial analysis of vector’s climatic suitability and virus’ temperature requirements. Int J Health Geogr. 2013;12:51.
Borgherini G, Poubeau P, Jossaume A, et al. Persistent arthralgia associated with chikungunya virus: a study of 88 adult patients on reunion island. Clin Infect Dis Off Public Infect Dis Soc Am. 2008;47:469–75.
Nkoghe D, Kassa RF, Caron M, et al. Clinical forms of chikungunya in Gabon, 2010. PLoS Negl Trop Dis. 2012;6:e1517.
Ramachandran V, Kaur P, Kanagasabai K, Vadivoo S, Murhekar M. Persistent arthralgia among Chikungunya patients and associated risk factors in Chennai, South India. J Postgrad Med. 2014;60:3–6.
Schilte C, Staikovsky F, Couderc T, et al. Chikungunya virus-associated long-term arthralgia: a 36-month prospective longitudinal study. PLoS Negl Trop Dis. 2013;7:e2137. doi:10.1371/journal.pntd.0002137.
Sissoko D, Malvy D, Ezzedine K, et al. Post-epidemic Chikungunya disease on Reunion Island: course of rheumatic manifestations and associated factors over a 15-month period. PLoS Negl Trop Dis. 2009;3:e389.
Rajapakse S, Rodrigo C, Rajapakse A. Atypical manifestations of chikungunya infection. Trans R Soc Trop Med Hyg. 2010;104:89–96.
Mahendradas P, Avadhani K, Shetty R. Chikungunya and the eye: a review. J Ophthal Inflam Infect. 2013;3:1–9.
Inamadar AC, Palit A, Sampagavi VV, Raghunath S, Deshmukh NS. Cutaneous manifestations of chikungunya fever: observations made during a recent outbreak in south India. Int J Dermatol. 2008;47:154–9.
Manimunda SP, Mavalankar D, Bandyopadhyay T, Sugunan AP. Chikungunya epidemic-related mortality. Epidemiol Infect. 2011;139:1410–2.
Josseran L, Paquet C, Zehgnoun A, et al. Chikungunya disease outbreak Reunion Island. Emerg Infect Dis. 2006;12:1994–5.
Moher D, Liberati A, Tetzlaff J, Altman DG. Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Tournebize P, Charlin C, Lagrange M. Neurological manifestations in Chikungunya: about 23 cases collected in Reunion Island. Revue Neurologique. 2009;165:48–51.
Rampal, Sharda M, Meena H. Neurological complications in chikungunya fever. J Assoc Phys India. 2007;55:765–9.
Oehler E, Fournier E, Leparc-Goffart I, et al. Increase in cases of Guillain–Barre syndrome during a Chikungunya outbreak, French Polynesia, 2014–2015. Euro Surveill. 2015;20:30079.
Gérardin P, Sampériz S, Ramful D, et al. Neurocognitive outcome of children exposed to perinatal mother-to-child Chikungunya virus infection: the CHIMERE cohort study on Reunion Island. PLoS Negl Trop Dis. 2014;8:e2996. doi:10.1371/journal.pntd.0002996.
Gérardin P, Barau G, Michault A, et al. Multidisciplinary prospective study of mother-to-child chikungunya virus infections on the island of La Réunion. PLoS Med. 2008;5:0413–23.
Ramful D, Carbonnier M, Pasquet M, et al. Mother-to-child transmission of chikungunya virus infection. Pediatr Infect Dis J. 2007;26:811–5.
Wakerley BR, Yuki N. Mimics and chameleons in Guillain–Barre and Miller Fisher syndromes. Pract Neurol. 2015;15:90–9.
Couderc T, Lecuit M. Chikungunya virus pathogenesis: from bedside to bench. Antivir Res. 2015;121:120–31.
Couderc T, Chrétien F, Schilte C, et al. A mouse model for Chikungunya: young age and inefficient type-I interferon signaling are risk factors for severe disease. PLoS Pathog. 2008;4:e29. doi:10.1371/journal.ppat.0040029.
Gasque P (2013) Chikungunya virus infection. In: Jackson AC (ed) Viral Infections of the Human Nervous System. vol (Gasque P., gasque@univ-reunion.fr) GRI EA4517, CPER/FEDER and ICRES PCRD7 Immunopathology and Infectious Disease Research Grouping, University of la Reunion CHU and CYROI, St. Denis, Reunion 97400, France. Springer, Basel, pp 295–315.
Das T, Hoarau JJ, Bandjee MCJ, Marianne M, Gasque P. Multifaceted innate immune responses engaged by astrocytes, microglia and resident dendritic cells against Chikungunya neuroinfection. J Gen Virol. 2015;96:294–310.
Inglis FM, Lee KM, Chiu KB, et al. Neuropathogenesis of Chikungunya infection: astrogliosis and innate immune activation. J Neurovirol. 2016;22:140–8.
Wakerley BR, Uncini A, Yuki N, Group GBSC, Group GBSC. Guillain–Barre and Miller Fisher syndromes—new diagnostic classification. Nat Rev Neurol. 2014;10:537–44.
Bourque PR, Chardon JW, Massie R. Autoimmune peripheral neuropathies. Clin Chim Acta Int J Clin Chem. 2015;449:37–42.
Lebrun G, Chadda K, Reboux AH, Martinet O, Gaüzère BA. Guillain–barré syndrome after chikungunya infection. Emerg Infect Dis. 2009;15:495–6.
Ang CW, Jacobs BC, Laman JD. The Guillain–Barre syndrome: a true case of molecular mimicry. Trends Immunol. 2004;25:61–6.
Mossberg N, Nordin M, Movitz C, et al. The recurrent Guillain–Barre syndrome: a long-term population-based study. Acta Neurol Scand. 2012;126:154–61.
Steiner I, Kennedy PG. Acute disseminated encephalomyelitis: current knowledge and open questions. J Neurovirol. 2015;21:473–9.
Das T, Jaffar-Bandjee MC, Hoarau JJ, et al. Chikungunya fever: CNS infection and pathologies of a re-emerging arbovirus. Prog Neurobiol. 2010;91:121–9.
Lewthwaite P, Vasanthapuram R, Osborne JC, et al. Chikungunya virus and central nervous system infections in children India. Emerg Infect Dis. 2009;15:329–31.
Chiam CW, Chan YF, Ong KC, Wong KT, Sam IC. Neurovirulence comparison of chikungunya virus isolates of the Asian and East/Central/South African genotypes from Malaysia. J Gen Virol. 2015;96:3243–54.
Acknowledgements
The following authors of case reports included in this study supplied supplementary data: Dr. Mahesh Gopalakrishnan (India), Dr. Prashanth Prabhu (India), Dr. Sher Bahadur Pun (Nepal), Dr. Suman Das (India), Dr. Anna Bank (USA), Prof. Uday Shankar Ghosh (India), Prof. Dulari Gupta (India), Dr. Penny Lewthwaite (UK), Dr. Bernard-Alex Gaüzère (France), Dr. Anne-Cécile Wielanek-Bachelet (France), Dr. Abhijit Mohite (UK), Dr. Jesse Waggoner and Dr. Benjamin Pinsky (USA), Prof. Alfonso J. Rodriguez-Morales (Colombia), Dr. Adrian C. L. Kee and Dr. Paul A. Tambyah (Singapore), Dr. Steven A. Sparr (USA), Prof. Lalitha Krishnan (India), Dr. Shimin Jasmine Chung (Singapore), Prof. Meenaxi Sharda (India), Dr. S. M. Katrak (India). We are very grateful to these authors for readily offering their time and data to the research community. Special thanks to Dr. Susanne Friedl, Ms. Margaritha Winter, Mr. Kirill Karlin and Ms. Anna Wang (Switzerland), for their support and critical lecture.
Author information
Authors and Affiliations
Contributions
TC was involved in methods, systematic review, data extraction, statistical analysis, results, and discussion. MS was involved in methods, data extraction, statistical analysis, results, and discussion. US was involved in methods, critical review for consistency, errors, and intellectual content. JL was involved in provision of extensive data, critical review for consistency, errors, and intellectual content. PG was involved in provision of extensive data, critical review for consistency, errors, and intellectual content; EK was involved in methods, critical review for consistency, errors and intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Standards
As a retrospective study, this article does not contain any studies with human participants or animals performed by any of the authors. The use of the patient’s data for the case report was approved by the ethical commission of the Canton of Zurich, Switzerland.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cerny, T., Schwarz, M., Schwarz, U. et al. The Range of Neurological Complications in Chikungunya Fever. Neurocrit Care 27, 447–457 (2017). https://doi.org/10.1007/s12028-017-0413-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-017-0413-8