Abstract
Objective
To determine the clinical characteristics and outcomes of patients with neurogenic stress cardiomyopathy (NSC) among patients admitted to our neuroscience intensive care unit (NICU).
Methods
Following institutional review board approval, consecutive adult patients admitted to the NICU between 2009 and 2013 with definite and possible NSC were included. Data on patient demographics, baseline clinical information, cardiac function, and laboratory values were collected. Outcomes included length of stay, modified Rankin Scale (mRS) at discharge and long-term follow-up. Continuous variables were compared using a student’s t test, and categorical variables were compared using a Chi-square test.
Results
Among 34 patients included in the study, the most common presenting symptom was dyspnea (17 patients, 50%). Subarachnoid hemorrhage (SAH) was the most common neurological inciting event (11 patients, 32.4%), but two-thirds of this cohort had other neurological triggers. The most common electrocardiogram changes were QT-interval prolongation (30 patients, 88.2%) and T-wave inversion (22 patients, 64.7%). The most common echocardiographic pattern was the apical variant (14 patients, 41.2%), and 26% of patients had right ventricular involvement (P = 0.03) which was a predictor of poor outcome along with inotropic support (P = 0.006). Functional outcome was poor (mRS > 3) in 53% of patients at discharge, but function improved over time in most survivors.
Conclusions
NSC is most common after SAH, but can result from a wide spectrum of acute brain insults. Requirement of inotropic support was the strongest indicator of prognosis at last follow-up. Patients with NSC often have poor function at discharge but many improve over time.
Similar content being viewed by others
Introduction
Stress cardiomyopathy is defined by the Mayo Clinic criteria as transient ventricular dysfunction, typically in a multivascular distribution, associated with either electrocardiogram (ECG) changes and/or cardiac biomarker evidence of myocardial injury/ischemia in the absence of significant obstructive coronary artery disease (CAD) [1]. There is no uniformly accepted terminology for this complex disease entity, which has also been described in the literature as apical ballooning syndrome (ABS), takotsubo cardiomyopathy (TC)/syndrome, and broken heart syndrome [2,3,4]. Stress cardiomyopathy can be secondary to a wide variety of physiologic, pathologic, and psychological events. Over the past several years, there has been increased awareness of the neurological causes of stress cardiomyopathy.
The most commonly recognized cause of neurogenic stress cardiomyopathy (NSC) is subarachnoid hemorrhage (SAH). However, relatively little is known regarding which other neurological conditions can induce the syndrome. Thus, the purpose of our study is to describe the range of neurological events that can incite the disorder, as well as to describe long-term clinical outcomes of a consecutive series of patients admitted to a neuroscience intensive care unit (NICU).
Methods
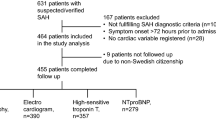
Patient Population
Institutional review board approval was obtained for conducting this retrospective study. Inclusion criteria were patients >18 years of age, admitted to the NICU between 2009 and 2013 with a primary neurological illnesses who developed one or more of the following according to retrospective review of physician notes and nursing flow sheets: cardiac symptoms (i.e., chest pain, dyspnea), hypotension requiring pressor or inotropic support, or ECG abnormalities (i.e., ST-segment elevation, inverted T-waves, QTc prolongation defined as >450 ms in males, and >470 ms in females). Patients with “definite” and “possible” NSC were included. Following identification of patients based on these criteria, troponin values and echocardiographic findings were used to identify NSC. Those who met a modified version of the Mayo Clinic criteria for stress cardiomyopathy were defined as “definite” (Table 1) [1], and those who had a similar presentation but did not have echocardiographic confirmation of reversal of the cardiomyopathy were defined as “possible.”
Data Collection
Baseline demographic data were collected from the medical records. Comorbidities studied included body mass index (BMI), hypertension, diabetes mellitus, current or prior tobacco use, CAD, baseline APACHE III score, and nadir Glasgow Coma Scale (GCS). Underlying neurological diagnoses were categorized as acute ischemic stroke, SAH, intraparenchymal hemorrhage (IPH), meningitis, seizure/epilepsy, tumor, posterior reversible leukoencephalopathy (PRES), and traumatic brain injury. We also reported the location of the lesion (left, right, bilateral) and the number of days from the neurological event to onset of stress cardiomyopathy.
Clinical symptoms at presentation of stress cardiomyopathy were categorized as dyspnea, chest pain, syncope, and shock. Left ventricular wall motion pattern was categorized as apical, non-apical (mid-ventricular, basal or global). The presence of right ventricular dysfunction on echocardiography was documented. Data were collected regarding the primary imaging modality used to document ventricular regional wall motion abnormality (i.e., transthoracic echocardiography, transesophageal echocardiography or angiography). Data were collected on ECG findings, cardiac troponin levels, complications, pharmacological agents used (antithrombotic agents, anti-hypertensives, and inotropes), and intubation and duration of ventilator support. Significant change in troponins was defined as an increase of ≥0.03 ng/mL at 3 and 6 h time points from initial value of <0.02 ng/mL, or increase of ≥20% between time points if initial value was ≥0.20 ng/mL. These are thresholds set by our local laboratory when a cardiac biomarker is ordered. Delta gap in troponin was calculated at 6 h.
Outcomes studied included NICU length of stay, hospital length of stay, outcome at discharge, and outcome at long-term follow-up. Discharge and long-term neurological outcomes were evaluated using the modified Rankin Score (mRS) with a good outcome being defined as a mRS ≤ 3. Outcomes were adjudicated by a vascular neurologist. The association between neurological outcome at last follow-up and several clinical characteristics at admission (age, gender, BMI, smoking history, CAD, diabetes mellitus, hypertension, baseline APACHE III, nadir GCS, renal impairment (based on RIFLE criteria [5]), sepsis [6], neurological state in intensive care unit at time of NSC presentation, length of hospital stay, lesion location, presence of seizure, SAH, type of stress cardiomyopathy, right ventricular involvement, troponin level, presence of arrhythmia, lowest ejection fraction (EF), and need for intubation and inotropic support) was investigated.
Statistical Analysis
Continuous variables are reported as mean ± SD or median with interquartile range in cases of non-normal distribution. Categorical variables are reported as N (%). Continuous variables were compared using a student’s t test, and categorical variables were compared using a Chi-square test. For the purposes of statistical analysis, the definite and possible groups were combined as one group as there were no significant differences in baseline characteristics, clinical characteristics, and outcomes between the two groups. All analyses were performed using JMP10.0 (www.jmp.com, Cary, NC).
Results
Patient Population
Thirty-four patients were included in this study. Eighteen patients had definite and 16 patients had possible NSC. The mean age was 61.8 ± 17.6 years. Twelve patients (35.3%) were male, and 22 patients (64.7%) were female. All patients were Caucasian with the exception of one for whom the race was not documented. These data are summarized in Table 2.
Clinical Presentation
Data on baseline clinical presentation are summarized in Supplementary Table 1. Of the 34 patients, 10 (29.4%) were awake at the time of NSC diagnosis, 14 (41.2%) were sedated, and 10 (29.4%) were comatose. The most common (32.4%) inciting neurological event was aneurysmal SAH. Additional triggers included ischemic stroke (11.8%), IPH (11.8%), and PRES (14.7%). Thirteen patients (38.2%) had seizures during hospitalization. A total of 8 patients (23.5%) had status epilepticus. The most common clinical presentation of NSC was dyspnea (50.0%), and the least common was chest pain (3 patients, 8.8%).
Cardiac Function
The most common pattern of NSC was the typical apical variant (14 patients, 41.2%). Right ventricular (RV) involvement occurred in 9 patients (26.5%) (Supplementary Table 2). The mean lowest EF was 40.9%. Nine (26.5%) patients had EF <30%. Pulmonary edema was evident on chest X-ray in 16 (47.1%) patients. The most common ECG changes were QTc interval prolongation (30, 88.2%). ST-segment elevation was present in 15 patients (44.1%). Twelve (35.3%) patients had cardiac arrhythmias. Elevated troponin T levels were present in the majority of patients (31 patients, 93.9%). Seventeen (54.8%) patients had a significant change in troponin levels on serial measurements. The median percent change in delta gap in troponin was −18.5% at 6 h. Of the 31 patients with elevated troponins, 21 patients had significant decreasing levels by 6 h, 6 patients had increasing troponins and 2 patients were not changed significantly over 6 h, and two did not have serial measurements. These data are summarized in Supplementary Table 2.
Cardiac and Respiratory Support
These data are summarized in Supplementary Table 2. Twenty-four (66.7%) patients required intubation. Sixteen (47.1%) patients required inotropic/vasopressor support. No patients required an intra-aortic balloon pump or extracorporeal membrane oxygenation. Twenty patients (58.8%) were placed on antithrombotic agents.
Outcomes
Three patients died in hospital. Three patients were lost to follow-up. At discharge, 18 patients (52.9%) had poor neurological outcome (mRS > 3), and 16 patients (47.1%) with good outcome. At median follow up of 4.9 months, 12 (38.7%) patients had poor outcome leaving 19 patients with good outcome (61.3%), 13 (42%) of which regained either full function or had minimal residual symptoms. No patients died purely of cardiac complications. Mean hospital length of stay was 20.5 days, and mean NICU length of stay was 10 days. These data are summarized in Table 3.
Univariate predictors of poor neurological functional outcome at last follow-up were the need for inotropic support (OR 7.00, 95% CI 1.69–30.85, P = 0.006) and RV involvement (OR 6.08, 95% CI 1.19–31.75, P = 0.03) (Table 4). The association with higher APACHE III score (P = 0.09) and a lower GCS (P = 0.11) was of borderline significance.
Discussion
Our study of consecutive patients with stress cardiomyopathy from an acute neurological cause demonstrated a number of interesting findings. First, we report that a wide range of neurogenic etiologies can trigger stress cardiomyopathy, including SAH and IPH, acute ischemic stroke, and PRES. Second, patients with NSC frequently have a poor early recovery, with half of patients having poor neurological function at discharge; however, meaningful functional recovery was commonly seen at follow-up. Predictors of poor neurological outcome in our study included the need for inotropic support and RV involvement.
Our study is unique in that we demonstrate that a wide variety of neurological disease triggers encountered in our center could result in NSC. The literature on NSC has focused on its association with aneurysmal SAH [7,8,9,10,11] and intracranial hemorrhage [12, 13]. While a number of case reports and a few small case series have suggested that other neurological insults can result in NSC, our series found that over two-thirds of NSC cases presenting to a NICU setting result from etiologies other than aneurysmal SAH [14,15,16,17].
The clinical presentation of those with stress cardiomyopathy from acute neurological disease may differ in some ways from traditional stress cardiomyopathy. It is common for stress cardiomyopathy to present with chest pain; however, as demonstrated in our case series and others, those with neurological triggers appear to present most commonly with dyspnea relating to signs of heart failure as opposed to chest pain [18, 19]. This may reflect the fact that patients with acute major neurological conditions may not be able to express or verbally report symptoms due to aphasia or altered mental status (66.7% of our patient cohort was sedated and/or comatose). These findings are important as they suggest that in the setting of an acute neurological injury and dyspnea, neurologists should have a high index of suspicion for NSC.
A recent case series by Ancona et al. [19] has compared traditional TC to NSC. The authors report that none of the 22 patients with NSC had ST-segment elevation, and 93% had mid-ventricular or basal variants with respect to regional wall abnormalities with only 21% wall abnormalities extending to or solely affecting the apex of the left ventricle. However, our study does not support these conclusions and to the contrary shows that 44% of patients had ST-segment elevation, and the vast majority had involvement of the apex with only 23% having mid-ventricular and/or basal involvement. One explanation for the discrepancy between the two studies may be that in the Ancona et al. study the majority of patients had NSC secondary to SAH. In contrast, a consistent finding between the studies is the higher proportion of males (35% on our study) in NSC compared to stress cardiomyopathy in general. This is consistent with our previous observation that men appear to develop TC as a consequence of physical triggers [20].
A modest elevation in troponin and QTc prolongation was present in the majority of our patient population. Although troponin levels and EF should not be used to differentiate stress cardiomyopathy from acute coronary syndrome, we note that 20 of the 27 patients with elevated troponins had significantly down trending troponin levels by 6 h, while only 5 patients had up trending levels. This finding suggests that there is an inherent latency in the process of reaching a diagnosis of NSC since troponin levels typically peak at around 12–24 h in stress cardiomyopathy, similar to an acute myocardial infarction [1].
A significant proportion of patients (30%) had poor long-term outcomes at follow-up. The only predictors of poor outcome in our study were right ventricular dysfunction and the need for inotropic support. The association between right ventricular dysfunction and poor outcome has been described in other series of stress cardiomyopathy literature [21,22,23,24] but not demonstrated to date in cases induced by acute neurological illness [25]. The fact that poor RV function and especially the need for inotropic support were predictors of poor functional outcome suggests that either severe forms of NSC might substantially impact patient prognosis or that the occurrence of clinically manifest NSC is a marker of a major neurological injury.
Limitations
This study has the limitations inherent to a retrospective design. Our patients did not uniformly undergo echocardiography and testing for cardiac injury biomarkers at specific time points. This may have resulted in under-detection of stress cardiomyopathy and a selection bias toward more severe cases. Lack of consistent echocardiographic follow-up and infrequent use of coronary angiography resulted in the need to use a modified definition of stress cardiomyopathy. We attempted to minimize bias selection by excluding patients with known CAD. However, these possible cases were otherwise comparable to those with a definite stress cardiomyopathy. The strength of the statistical associations is tempered by the very wide confidence intervals, which is inherent in a small study of a rare condition such as this. Finally, our statistical analysis may have been underpowered for the detection of more modest associations with factors that may predict functional outcome and the size of our cohort also prevented us from being able to perform a multivariable analysis.
Conclusions
NSC is a complex entity that can result from a wide variety of neurological insults. Clinical and laboratory clues that can aid in the diagnosis of NSC include dyspnea, QTc prolongation, and elevated troponin levels. Poor neurological outcome appears to correlate with the presence of more severe cardiac injury. Neurocritical patients with this cardiac complication often have impaired neurological function upon discharge, but they have potential for recovery.
References
Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J. 2008;155:408–17.
Roshanzamir S, Showkathali R. Takotsubo cardiomyopathy a short review. Curr Cardiol Rev. 2013;9:191–6.
Yoshikawa T. Takotsubo cardiomyopathy, a new concept of cardiomyopathy: clinical features and pathophysiology. Int J Cardiol. 2015;182:297–303.
Sharkey SW, Lesser JR, Maron MS, Maron BJ. Why not just call it tako-tsubo cardiomyopathy: a discussion of nomenclature. J Am Coll Cardiol. 2011;57:1496–7.
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P, Acute Dialysis Quality Initiative W. Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the second international consensus conference of the acute dialysis quality initiative (ADQI) group. Crit Care. 2004;8:R204–12.
Dellinger RP, Levy MM, Carlet JM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36:296–327.
Kilbourn KJ, Levy S, Staff I, Kureshi I, McCullough L. Clinical characteristics and outcomes of neurogenic stress cadiomyopathy in aneurysmal subarachnoid hemorrhage. Clin Neurol Neurosurg. 2013;115:909–14.
Malik AN, Gross BA, Rosalind Lai PM, Moses ZB, Du R. Neurogenic stress cardiomyopathy after aneurysmal subarachnoid hemorrhage. World Neurosurg. 2015;83:880–5.
Liang CW, Chen R, Macri E, Naval N. Preadmission beta-blockers are associated with decreased incidence of neurogenic stunned myocardium in aneurysmal subarachnoid hemorrhage. J Stroke Cerebrovasc Dis. 2013;22:601–7.
Lee VH, Connolly HM, Fulgham JR, Manno EM, Brown RD Jr, Wijdicks EF. Tako-tsubo cardiomyopathy in aneurysmal subarachnoid hemorrhage: an underappreciated ventricular dysfunction. J Neurosurg. 2006;105:264–70.
Abd TT, Hayek S, Cheng JW, Samuels OB, Wittstein IS, Lerakis S. Incidence and clinical characteristics of takotsubo cardiomyopathy post-aneurysmal subarachnoid hemorrhage. Int J Cardiol. 2014;176:1362–4.
Putaala J, Lehto M, Meretoja A, et al. In-hospital cardiac complications after intracerebral hemorrhage. Int J Stroke. 2014;9:741–6.
Inamasu J, Ito K, Sugimoto K, Watanabe E, Kato Y, Hirose Y. Cardiac wall motion abnormality associated with spontaneous intracerebral hemorrhage. Int J Cardiol. 2013;168:1667–9.
Yoshimura S, Toyoda K, Ohara T, et al. Takotsubo cardiomyopathy in acute ischaemic stroke. Ann Neurol. 2008;64:547–54.
Schneider F, Kadel C, Pagitz M, Sen S. Takotsubo cardiomyopathy and elevated troponin levels following cerebral seizure. Int J Cardiol. 2010;145:586–7.
Finsterer J, Wahbi K. CNS disease triggering Takotsubo stress cardiomyopathy. Int J Cardiol. 2014;177:322–9.
Summers MR, Madhavan M, Chokka RG, Rabinstein AA, Prasad A. Coincidence of apical ballooning syndrome (tako-tsubo/stress cardiomyopathy) and posterior reversible encephalopathy syndrome: potential common substrate and pathophysiology? J Card Fail. 2012;18:120–5.
Templin C, Ghadri JR, Diekmann J, et al. Clinical features and outcomes of takotsubo (stress) cardiomyopathy. N Engl J Med. 2015;373:929–38.
Ancona F, Bertoldi LF, Ruggieri F, et al. Takotsubo cardiomyopathy and neurogenic stunned myocardium: similar albeit different. Eur Heart J. 2016;37:2830–32.
Patel SM, Chokka RG, Prasad K, Prasad A. Distinctive clinical characteristics according to age and gender in apical ballooning syndrome (takotsubo/stress cardiomyopathy): an analysis focusing on men and young women. J Card Fail. 2013;19:306–10.
Finocchiaro G, Kobayashi Y, Magavern E, et al. Prevalence and prognostic role of right ventricular involvement in stress-induced cardiomyopathy. J Card Fail. 2015;21:419–25.
Rodrigues AC, Guimaraes L, Lira E, et al. Right ventricular abnormalities in takotsubo cardiomyopathy. Echocardiography. 2013;30:1015–21.
Eitel I, von Knobelsdorff-Brenkenhoff F, Bernhardt P, et al. Clinical characteristics and cardiovascular magnetic resonance findings in stress (takotsubo) cardiomyopathy. JAMA. 2011;306:277–86.
Haghi D, Athanasiadis A, Papavassiliu T, et al. Right ventricular involvement in takotsubo cardiomyopathy. Eur Heart J. 2006;27:2433–9.
Kilbourn KJ, Ching G, Silverman DI, McCullough L, Brown RJ. Clinical outcomes after neurogenic stress induced cardiomyopathy in aneurysmal sub-arachnoid hemorrhage: a prospective cohort study. Clin Neurol Neurosurg. 2015;128:4–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nasr, D.M., Tomasini, S., Prasad, A. et al. Acute Brain Diseases as Triggers for Stress Cardiomyopathy: Clinical Characteristics and Outcomes. Neurocrit Care 27, 356–361 (2017). https://doi.org/10.1007/s12028-017-0412-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-017-0412-9