Abstract
Background
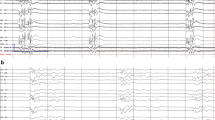
Existing studies of quantitative electroencephalography (qEEG) as a prognostic tool after cardiac arrest (CA) use methods that ignore the longitudinal pattern of qEEG data, resulting in significant information loss and precluding analysis of clinically important temporal trends. We tested the utility of group-based trajectory modeling (GBTM) for qEEG classification, focusing on the specific example of suppression ratio (SR).
Methods
We included comatose CA patients hospitalized from April 2010 to October 2014, excluding CA from trauma or neurological catastrophe. We used Persyst®v12 to generate SR trends and used semi-quantitative methods to choose appropriate sampling and averaging strategies. We used GBTM to partition SR data into different trajectories and regression associate trajectories with outcome. We derived a multivariate logistic model using clinical variables without qEEG to predict survival, then added trajectories and/or non-longitudinal SR estimates, and assessed changes in model performance.
Results
Overall, 289 CA patients had ≥36 h of EEG yielding 10,404 h of data (mean age 57 years, 81 % arrested out-of-hospital, 33 % shockable rhythms, 31 % overall survival, 17 % discharged to home or acute rehabilitation). We identified 4 distinct SR trajectories associated with survival (62, 26, 12, and 0 %, P < 0.0001 across groups) and CPC (35, 10, 4, and 0 %, P < 0.0001 across groups). Adding trajectories significantly improved model performance compared to adding non-longitudinal data.
Conclusions
Longitudinal analysis of continuous qEEG data using GBTM provides more predictive information than analysis of qEEG at single time-points after CA.


Similar content being viewed by others
References
Coppler PJ, Elmer J, Calderon L, Sabedra A, Doshi AA, Callaway CW, et al. Validation of the Pittsburgh Cardiac Arrest Category illness severity score. Resuscitation. 2015. doi:10.1016/j.resuscitation.2015.01.020.
Laver S, Farrow C, Turner D, Nolan J. Mode of death after admission to an intensive care unit following cardiac arrest. Intensive Care Med. 2004;30(11):2126–8. doi:10.1007/s00134-004-2425-z.
Rittenberger JC, Popescu A, Brenner RP, Guyette FX, Callaway CW. Frequency and timing of nonconvulsive status epilepticus in comatose post-cardiac arrest subjects treated with hypothermia. Neurocrit Care. 2012;16(1):114–22. doi:10.1007/s12028-011-9565-0.
Rossetti AO, Carrera E, Oddo M. Early EEG correlates of neuronal injury after brain anoxia. Neurology. 2012;78(11):796–802. doi:10.1212/WNL.0b013e318249f6bb.
Cloostermans MC, van Meulen FB, Eertman CJ, Hom HW, van Putten MJ. Continuous electroencephalography monitoring for early prediction of neurological outcome in postanoxic patients after cardiac arrest: a prospective cohort study. Crit Care Med. 2012;40(10):2867–75. doi:10.1097/CCM.0b013e31825b94f0.
Crepeau AZ, Rabinstein AA, Fugate JE, Mandrekar J, Wijdicks EF, White RD, et al. Continuous EEG in therapeutic hypothermia after cardiac arrest: prognostic and clinical value. Neurology. 2013;80(4):339–44. doi:10.1212/WNL.0b013e31827f089d.
Mani R, Schmitt SE, Mazer M, Putt ME, Gaieski DF. The frequency and timing of epileptiform activity on continuous electroencephalogram in comatose post-cardiac arrest syndrome patients treated with therapeutic hypothermia. Resuscitation. 2012;83(7):840–7. doi:10.1016/j.resuscitation.2012.02.015.
Rossetti AO, Urbano LA, Delodder F, Kaplan PW, Oddo M. Prognostic value of continuous EEG monitoring during therapeutic hypothermia after cardiac arrest. Crit Care. 2010;14(5):R173. doi:10.1186/cc9276.
Foreman B, Claassen J. Quantitative EEG for the detection of brain ischemia. Crit Care. 2012;16(2):216. doi:10.1186/cc11230.
Rundgren M, Westhall E, Cronberg T, Rosen I, Friberg H. Continuous amplitude-integrated electroencephalogram predicts outcome in hypothermia-treated cardiac arrest patients. Crit Care Med. 2010;38(9):1838–44. doi:10.1097/CCM.0b013e3181eaa1e7.
Oh SH, Park KN, Kim YM, Kim HJ, Youn CS, Kim SH, et al. The prognostic value of continuous amplitude-integrated electroencephalogram applied immediately after return of spontaneous circulation in therapeutic hypothermia-treated cardiac arrest patients. Resuscitation. 2013;84(2):200–5. doi:10.1016/j.resuscitation.2012.09.031.
Wennervirta JE, Ermes MJ, Tiainen SM, Salmi TK, Hynninen MS, Sarkela MO, et al. Hypothermia-treated cardiac arrest patients with good neurological outcome differ early in quantitative variables of EEG suppression and epileptiform activity. Crit Care Med. 2009;37(8):2427–35. doi:10.1097/CCM.0b013e3181a0ff84.
Seder DB, Fraser GL, Robbins T, Libby L, Riker RR. The bispectral index and suppression ratio are very early predictors of neurological outcome during therapeutic hypothermia after cardiac arrest. Intensiv Care Med. 2010;36(2):281–8. doi:10.1007/s00134-009-1691-1.
Selig C, Riegger C, Dirks B, Pawlik M, Seyfried T, Klingler W. Bispectral index (BIS) and suppression ratio (SR) as an early predictor of unfavourable neurological outcome after cardiac arrest. Resuscitation. 2014;85(2):221–6. doi:10.1016/j.resuscitation.2013.11.008.
Tjepkema-Cloostermans MC, van Meulen FB, Meinsma G, van Putten MJ. A Cerebral Recovery Index (CRI) for early prognosis in patients after cardiac arrest. Crit Care. 2013;17(5):R252. doi:10.1186/cc13078.
Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109–38. doi:10.1146/annurev.clinpsy.121208.131413.
Rittenberger JC, Guyette FX, Tisherman SA, DeVita MA, Alvarez RJ, Callaway CW. Outcomes of a hospital-wide plan to improve care of comatose survivors of cardiac arrest. Resuscitation. 2008;79(2):198–204. doi:10.1016/j.resuscitation.2008.08.014.
Rittenberger JC, Tisherman SA, Holm MB, Guyette FX, Callaway CW. An early, novel illness severity score to predict outcome after cardiac arrest. Resuscitation. 2011;82(11):1399–404. doi:10.1016/j.resuscitation.2011.06.024.
Frisch A, Reynolds JC, Condle J, Gruen D, Callaway CW. Documentation discrepancies of time-dependent critical events in out of hospital cardiac arrest. Resuscitation. 2014;85(8):1111–4. doi:10.1016/j.resuscitation.2014.05.002.
Rittenberger JC, Martin JR, Kelly LJ, Roth RN, Hostler D, Callaway CW. Inter-rater reliability for witnessed collapse and presence of bystander CPR. Resuscitation. 2006;70(3):410–5. doi:10.1016/j.resuscitation.2005.12.015.
Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27(2):157–72. doi:10.1002/sim.2929 discussion 207–12.
Oh SH, Park KN, Shon YM, Kim YM, Kim HJ, Youn CS, et al. Continuous amplitude-integrated electroencephalographic monitoring is a useful prognostic tool for hypothermia-treated cardiac arrest patients. Circulation. 2015. doi:10.1161/CIRCULATIONAHA.115.015754.
Friberg H, Westhall E, Rosen I, Rundgren M, Nielsen N, Cronberg T. Clinical review: continuous and simplified electroencephalography to monitor brain recovery after cardiac arrest. Crit Care. 2013;17(4):233. doi:10.1186/cc12699.
Chennu S, O’Connor S, Adapa R, Menon DK, Bekinschtein TA. brain connectivity dissociates responsiveness from drug exposure during propofol-induced transitions of consciousness. PLoS Comput Biol. 2016;12(1):e1004669. doi:10.1371/journal.pcbi.1004669.
Kamps MJ, Horn J, Oddo M, Fugate JE, Storm C, Cronberg T, et al. Prognostication of neurologic outcome in cardiac arrest patients after mild therapeutic hypothermia: a meta-analysis of the current literature. Intensiv Care Med. 2013;39(10):1671–82. doi:10.1007/s00134-013-3004-y.
Bouwes A, Binnekade JM, Kuiper MA, Bosch FH, Zandstra DF, Toornvliet AC, et al. Prognosis of coma after therapeutic hypothermia: a prospective cohort study. Ann Neurol. 2012;71(2):206–12. doi:10.1002/ana.22632.
Rossetti AO, Koenig MA. Prognostication after cardiac arrest: a tale of timing, confounders, and self-fulfillment. Neurology. 2011;77(14):1324–5. doi:10.1212/WNL.0b013e318231533b.
Cronberg T, Horn J, Kuiper MA, Friberg H, Nielsen N. A structured approach to neurologic prognostication in clinical cardiac arrest trials. Scand J Trauma Resusc Emerg Med. 2013;21:45. doi:10.1186/1757-7241-21-45.
Cronberg T, Brizzi M, Liedholm LJ, Rosen I, Rubertsson S, Rylander C, et al. Neurological prognostication after cardiac arrest–recommendations from the Swedish Resuscitation Council. Resuscitation. 2013;84(7):867–72. doi:10.1016/j.resuscitation.2013.01.019.
Wijdicks EF, Hijdra A, Young GB, Bassetti CL, Wiebe S. Quality Standards Subcommittee of the American Academy of N. Practice parameter: prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2006;67(2):203–10. doi:10.1212/01.wnl.0000227183.21314.cd.
Sandroni C, Cariou A, Cavallaro F, Cronberg T, Friberg H, Hoedemaekers C, et al. Prognostication in comatose survivors of cardiac arrest: an advisory statement from the European Resuscitation Council and the European Society of Intensive Care Medicine. Resuscitation. 2014;85(12):1779–89. doi:10.1016/j.resuscitation.2014.08.011.
Golan E, Barrett K, Alali AS, Duggal A, Jichici D, Pinto R, et al. Predicting neurologic outcome after targeted temperature management for cardiac arrest: systematic review and meta-analysis. Crit Care Med. 2014;42(8):1919–30. doi:10.1097/CCM.0000000000000335.
Hofmeijer J, Tjepkema-Cloostermans MC, van Putten MJ. Burst-suppression with identical bursts: a distinct EEG pattern with poor outcome in postanoxic coma. Clin Neurophysiol. 2014;125(5):947–54. doi:10.1016/j.clinph.2013.10.017.
Niedermeyer E, Sherman DL, Geocadin RJ, Hansen HC, Hanley DF. The burst-suppression electroencephalogram. Clin Electroencephalogr. 1999;30(3):99–105.
Thomke F, Brand A, Weilemann SL. The temporal dynamics of postanoxic burst-suppression EEG. J Clin Neurophysiol. 2002;19(1):24–31.
Acknowledgments
Dr. Elmer’s research time was supported by NIH Grant 5K12HL109068.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to report.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Elmer, J., Gianakas, J.J., Rittenberger, J.C. et al. Group-Based Trajectory Modeling of Suppression Ratio After Cardiac Arrest. Neurocrit Care 25, 415–423 (2016). https://doi.org/10.1007/s12028-016-0263-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-016-0263-9