Abstract
Background
The treatment of refractory status epilepticus (RSE) remains largely empirical. Lacosamide (LCM) is a new anticonvulsant available in intravenous (IV) form, but its optimal dosing regimen for the treatment of RSE is unknown. We compared safety and efficacy of two loading doses: 200 and 400 mg.
Methods
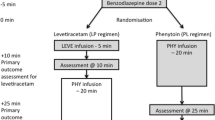
Prospective observational study of all patients who received IV LCM for RSE or seizure clusters between October 2010 and December 2012. A first group received an IV load of 200 mg of LCM. After the initial part of the study, and due to poor results with this dosage, a second group received a loading dose of 400 mg. Outcome measures included response rate, time to response, and adverse events.
Results
There was a trend in favor of a higher response rate to LCM in the 400 mg group [7/14 (50 %) vs. 2/11 (18 %), respectively; p = 0.2]. Early responses (occurring within 3 h of initiation of LCM) were significantly more frequent in the 400 mg group [4/14 (28 %) vs. 0/11 (0 %); p = 0.026]. Overall, 9/25 patients (36 %) responded to LCM and seizures were terminated in eight more patients (32 %), by adding other anticonvulsants. The following adverse events were attributed to LCM: myoclonus and confusion, increase in seizure frequency, vertigo, ataxia, and an asymptomatic increase in liver enzymes level. All occurred in the 200 mg group. No skin rash, renal, cardiac, or hemodynamic side effects were observed in any group.
Conclusions
In this small prospective observational study, an initial dose of 400 mg of IV LCM was associated with a higher proportion of early termination of RSE and with a trend toward a higher response rate.
Similar content being viewed by others
References
Meierkord H, Boon P, Engelsen B, et al. EFNS guideline on the management of status epilepticus in adults. Eur J Neurol. 2010;17:348–55.
Brophy GM, Bell R, Claassen J, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17(1):3–23.
Hocker SE, Britton JW, Mandrekar JN, Wijdicks EFM, Rabinstein AA. Predictors of outcome in refractory status epilepticus. Arch Neurol. 2012;8:1–6.
Kowalski RG, Ziai WC, Rees RN, et al. Third-line antiepileptic therapy and outcome in status epilepticus: the impact of vasopressor use and prolonged mechanical ventilation. Crit Care Med. 2012;40(9):2677–84.
Alvarez V, Januel JM, Burnand B, Rossetti AO. Second-line status epilepticus treatment: comparison of phenytoin, valproate, and levetiracetam. Epilepsia. 2011;52(7):1292–6.
Albers JM, Moddel G, Dittrich R, et al. Intravenous lacosamide—an effective add-on treatment of refractory status epilepticus. Seizure. 2011;20(5):428–30.
Rantsch K, Walter U, Wittstock M, Benecke R, Rosche J. Efficacy of intravenous lacosamide in refractory nonconvulsive status epilepticus and simple partial status epilepticus. Seizure. 2011;20(7):529–32.
Parkerson KA, Reinsberger C, Chou SH, Dworetzky BA, Lee JW. Lacosamide in the treatment of acute recurrent seizures and periodic epileptiform patterns in critically ill patients. Epilepsy Behav. 2011;20(1):48–51.
Koubeissi MZ, Mayor CL, Estephan B, Rashid S, Azar NJ. Efficacy and safety of intravenous lacosamide in refractory nonconvulsive status epilepticus. Acta Neurol Scand. 2011;123(2):142–6.
Kellinghaus C, Berning S, Immisch I, et al. Intravenous lacosamide for treatment of status epilepticus. Acta Neurol Scand. 2011;123(2):137–41.
Hofler J, Unterberger I, Dobesberger J, Kuchukhidze G, Walser G, Trinka E. Intravenous lacosamide in status epilepticus and seizure clusters. Epilepsia. 2011;52(10):e148–52.
Goodwin H, Hinson HE, Shermock KM, Karanjia N, Lewin JJ III. The use of lacosamide in refractory status epilepticus. Neurocrit Care. 2011;14(3):348–53.
Jain V, Harvey AS. Treatment of refractory tonic status epilepticus with intravenous lacosamide. Epilepsia. 2012;53(4):761–2.
Mnatsakanyan L, Chung JM, Tsimerinov EI, Eliashiv DS. Intravenous lacosamide in refractory nonconvulsive status epilepticus. Seizure. 2012;21(3):198–201.
Cherry S, Judd L, Muniz JC, Elzawahry H, LaRoche S. Safety and efficacy of lacosamide in the intensive care unit. Neurocrit Care. 2012;16(2):294–8.
Höfler J, Trinka E. Lacosamide as a new treatment option in status epilepticus. Epilepsia. 2013;54(3):393–404.
Young GB, Jordan KG, Doig GS. An assessment of nonconvulsive seizures in the intensive care unit using continuous EEG monitoring: an investigation of variables associated with mortality. Neurology. 1996;47(1):83–9.
Belcastro V, Arnaboldi M, Taborelli A, Prontera P. Induction of epileptic negative myoclonus by addition of lacosamide to carbamazepine. YEBEH. 2011;20(3):2.
Disclosures
This study was not initiated, and not sponsored by UCB. Marcel Levy-Nogueira, Noémie Ligot, Gilles Naeije have no conflict of interest. Nicolas Mavroudakis received travel grant from Pfizer. Chantal Depondt received research grant and travel grant from UCB. Those grants were unrelated to this study. Benjamin Legros received research grant from UCB, speaker honorarium from UCB, Pfizer, GSK, and Sanofi, consulting honorarium from UCB, GSK, Pfizer, travel grants from UCB, Pfizer, GSK, Janssens Cilag, Novartis, Sanofi and Cyberonics. The research grant was unrelated to this study. Two travel grants were used to present partial data of this study. Nicolas Gaspard is the recipient of a Postdoctoral Research Fellowship from the Epilepsy Foundation of America, was the recipient of a Postdoctoral Research Fellowship from the Belgian American Education Foundation, and received research grant from the Commission for Educational Exchange between the USA and Belgium and the Belgian Neurological Society.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Legros, B., Depondt, C., Levy-Nogueira, M. et al. Intravenous Lacosamide in Refractory Seizure Clusters and Status Epilepticus: Comparison of 200 and 400 mg Loading Doses. Neurocrit Care 20, 484–488 (2014). https://doi.org/10.1007/s12028-013-9882-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-013-9882-6