Abstract
Background
Effectiveness of cooling and adverse events (AEs) involving skin have not been intensively evaluated in cardiac arrest survivors treated with therapeutic hypothermia (TH) when induced and maintained with a servomechanism-regulated surface cooling system.
Methods
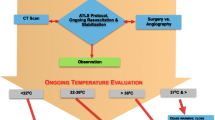
Retrospective review of sixty-nine cardiac arrest survivor-events admitted from April 2006–September 2008 who underwent TH using the Medivance Arctic Sun Temperature Management System. A TH database and medical records were reviewed, and nursing interviews conducted. Primary endpoint was time from initiation to target temperature (TT; 32–34°C). Secondary endpoints were cooling rate, percentage of hypothermia maintenance phase at TT, effect of body-mass index (BMI) on rate of cooling, and AEs.
Results
Mean time to the target temperature (TT) was 2.78 h; 80% of patients achieved TT within 4 h; all did within 8 h. Patients were at TT for 96.7% of hypothermia maintenance; 17% of patients had >1 hourly temperature measurement outside TT range. Mean cooling rate during induction phase was 1.1°C/h, and was not associated with BMI. Minor skin injury occurred in 14 (20%) patients; 4 (6%) were device-related. Skin injuries were associated with shock (P = 0.04), and decubitus ulcers were associated with left ventricular ejection fraction <45% (P = 0.004). AEs included shivering (94%), hypokalemia (81%), hyperglycemia (57%), pneumonia (23%), bleeding (22%), post-cooling fever (17%), and bacteremia (9%).
Conclusions
The Arctic Sun Temperature Management System was an effective means of performing therapeutic hypothermia after cardiac arrest. Infrequent skin injuries were associated with vasopressor use and low ejection fraction.


Similar content being viewed by others
References
Neumar RW, Nolan JP, Adrie C, et al. Postcardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. Circulation. 2008;118:2452–83.
Holzer M. Targeted temperature management for comatose survivors of cardiac arrest. N Engl J Med. 2010;363:1256–64.
Peberdy MA, Callaway CW, Neumar RW, et al. Part 9: post-cardiac arrest care: 2010 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122:S768–86.
Bernard S, Buist M, Monteiro O, Smith K. Induced hypothermia using large volume, ice-cold intravenous fluid in comatose survivors of out-of-hospital cardiac arrest: a preliminary report. Resuscitation. 2003;56:9–13.
Holzer M. Devices for rapid induction of hypothermia. Eur J Anaesthesiol Suppl. 2008;42:31–8.
The Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346:549–56.
Hachimi-Idrissi S, Corne L, Ebinger G, Michotte Y, Huyghens L. Mild hypothermia induced by a helmet device: a clinical feasibility study. Resuscitation. 2001;51:275–81.
Busch HJ, Eichwede F, Födisch M, et al. Safety and feasibility of nasopharyngeal evaporative cooling in the emergency department setting in survivors of cardiac arrest. Resuscitation. 2010;81:943–9.
Boller M, Lampe JW, Katz JM, Barbut D, Becker LB. Feasibility of intra-arrest hypothermia induction: a novel nasopharyngeal approach achieves preferential brain cooling. Resuscitation. 2010;81:1025–30.
Castrén M, Nordberg P, Svensson L, et al. Intra-arrest transnasal evaporative cooling: a randomized, prehospital, multicenter study (PRINCE: Pre-ROSC IntraNasal Cooling Effectiveness). Circulation. 2010;122:729–36.
Kory P, Weiner J, Mathew JP, et al. A rapid, safe, and low-cost technique for the induction of mild therapeutic hypothermia in post-cardiac arrest patients. Resuscitation. 2010. [Epub ahead of print] PMID: 21050652.
Mayer SA, Kowalski RG, Presciutti M, et al. Clinical trial of a novel surface cooling system for fever control in neurocritical care patients. Crit Care Med. 2004;32:2508–15.
Merchant RM, Abella BS, Peberdy MA, et al. Therapeutic hypothermia after cardiac arrest: unintentional overcooling is common using ice packs and conventional cooling blankets. Crit Care Med. 2006;34:S490–4.
Gillies MA, Pratt R, Whiteley C, Borg J, Beale RJ, Tibby SM. Therapeutic hypothermia after cardiac arrest: a retrospective comparison of surface and endovascular cooling techniques. Resuscitation. 2010;81:1117–22.
Holzer M, Müllner M, Sterz F, et al. Efficacy and safety of endovascular cooling after cardiac arrest: cohort study and Bayesian approach. Stroke. 2006;37:1792–7.
Hoedemaekers CW, Ezzahti M, Gerritsen A, van der Hoeven JG. Comparison of cooling methods to induce and maintain normo- and hypothermia in intensive care unit patients: a prospective intervention study. Crit Care. 2007;11:R91.
Varon J, Acosta P, Wintz R, Mendoza N. Unusual side effect from hydrogel pads during therapeutic hypothermia. Resuscitation. 2008;78:248–9.
Polderman KH, Herold I. Therapeutic hypothermia and controlled normothermia in the intensive care unit: practical considerations, side effects, and cooling methods. Crit Care Med. 2009;37(3):1101–20.
Seder DB, Van der Kloot TE. Methods of cooling: practical aspects of therapeutic temperature management. Crit Care Med. 2009;37:S211–22.
Seder DB, Fraser GL, Robbins T, Libby L, Riker RR. The bispectral index and suppression ratio are very early predictors of neurological outcome during therapeutic hypothermia after cardiac arrest. Intensive Care Med. 2010;36:281–8.
Badjatia N, Strongilis E, Prescutti M, et al. Metabolic benefits of surface counter warming during therapeutic temperature modulation. Crit Care Med. 2009;37:1893–7.
Sirvent JM, Torres A, El-Ebiary M, Castro P, de Batlle J, Bonet A. Protective effect of intravenously administered cefuroxime against nosocomial pneumonia in patients with structural coma. Am J Respir Crit Care Med. 1997;155:1729–34.
Acquarolo A, Urli T, Perone G, Giannotti C, Candiani A, Latronico N. Antibiotic prophylaxis of early onset pneumonia in critically ill comatose patients. A randomized study. Intensive Care Med. 2005;31:510–6.
American Thoracic Society; Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388–416.
Fàbregas N, Ewig S, Torres A, et al. Clinical diagnosis of ventilator associated pneumonia revisited: comparative validation using immediate post-mortem lung biopsies. Thorax. 1999;54:867–73.
Jacobshagen C, Pax A, Unsöld BW, Seidler T, Schmidt-Schweda S, Hasenfuss G, Maier LS. Effects of large volume, ice-cold intravenous fluid infusion on respiratory function in cardiac arrest survivors. Resuscitation. 2009;80:1223–8.
Polderman KH, Rijnsburger ER, Peerdeman SM, Girbes AR. Induction of hypothermia in patients with various types of neurological injury with use of large volumes of ice-cold intravenous fluid. Crit Care Med. 2005;33:2744–51.
Kliegel A, Janata A, Wandaller C, et al. Cold infusions alone are effective for induction of therapeutic hypothermia but do not keep patients cool after cardiac arrest. Resuscitation. 2007;73:46–53.
Kim F, Olsufka M, Carlbom D, et al. Pilot study of rapid infusion of 2 L of 4°C normal saline for induction of mild hypothermia in hospitalized, comatose survivors of out-of-hospital cardiac arrest. Circulation. 2005;112:715–9.
Oddo M, Schaller MD, Feihl F, Ribordy V, Liaudet L. From evidence to clinical practice: effective implementation of therapeutic hypothermia to improve patient outcome after cardiac arrest. Crit Care Med. 2006;34:1865–73.
Nielsen N, Sunde K, Hovdenes J, et al. Adverse events and their relation to mortality in out-of-hospital cardiac arrest patients treated with therapeutic hypothermia. Crit Care Med. 2010. [Epub ahead of print] PMID: 20959789.
Acknowledgments
The authors wish to acknowledge the outstanding contributions of research coordinators Tracy Robbins and Laurel Libby to this study.
Conflict of interest
The authors of this study report no financial conflict of interest with any commercial interest related to therapeutic hypothermia.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jarrah, S., Dziodzio, J., Lord, C. et al. Surface Cooling after Cardiac Arrest: Effectiveness, Skin Safety, and Adverse Events in Routine Clinical Practice. Neurocrit Care 14, 382–388 (2011). https://doi.org/10.1007/s12028-011-9506-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-011-9506-y