Abstract
Background
Brain energy metabolic crisis (MC) and lactate–pyruvate ratio (LPR) elevations have been linked to poor outcome in comatose patients. We sought to determine if MC and LPR elevations after subarachnoid hemorrhage (SAH) are associated with acute reductions in serum glucose.
Methods
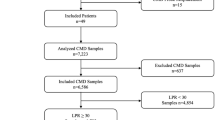
Twenty-eight consecutive comatose SAH patients that underwent multimodality monitoring with intracranial pressure and microdialysis were studied. MC was defined as lactate/pyruvate ratio (LPR) ≥ 40 and brain glucose < 0.7 mmol/l. Time-series data were analyzed using a multivariable general linear model with a logistic link function for dichotomized outcomes.
Results
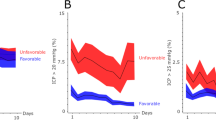
Multimodality monitoring included 3,178 h of observation (mean 114 ± 65 h per patient). In exploratory analysis, serum glucose significantly decreased from 8.2 ± 1.8 mmol/l (148 mg/dl) 2 h before to 6.9 ± 1.9 mmol/l (124 mg/dl) at the onset of MC (P < 0.001). Reductions in serum glucose of 25% or more were significantly associated with new onset MC (adjusted odds ratio [OR] 3.6, 95% confidence interval [CI] 2.2–6.0). Acute reductions in serum glucose of 25% or more were also significantly associated with an LPR rise of 25% or more (adjusted OR 1.6, 95% CI 1.1–2.4). All analyses were adjusted for significant covariates including Glasgow Coma Scale and cerebral perfusion pressure.
Conclusions
Acute reductions in serum glucose, even to levels within the normal range, may be associated with brain energy metabolic crisis and LPR elevation in poor-grade SAH patients.

Similar content being viewed by others
References
Komotar RJ, et al. Resuscitation and critical care of poor-grade subarachnoid hemorrhage. Neurosurgery. 2009;64(3):397–410. discussion 410–1.
Sarrafzadeh A, et al. Poor-grade aneurysmal subarachnoid hemorrhage: relationship of cerebral metabolism to outcome. J Neurosurg. 2004;100(3):400–6.
Vespa P, et al. Metabolic crisis without brain ischemia is common after traumatic brain injury: a combined microdialysis and positron emission tomography study. J Cereb Blood Flow Metab. 2005;25(6):763–74.
Hillered L, Vespa PM, Hovda DA. Translational neurochemical research in acute human brain injury: the current status and potential future for cerebral microdialysis. J Neurotrauma. 2005;22(1):3–41.
Bellander BM, et al. Consensus meeting on microdialysis in neurointensive care. Intensive Care Med. 2004;30(12):2166–9.
Hlatky R, et al. Patterns of energy substrates during ischemia measured in the brain by microdialysis. J Neurotrauma. 2004;21(7):894–906.
Schulz MK, et al. Cerebral microdialysis monitoring: determination of normal and ischemic cerebral metabolisms in patients with aneurysmal subarachnoid hemorrhage. J Neurosurg. 2000;93(5):808–14.
Johnston AJ, et al. Effect of cerebral perfusion pressure augmentation on regional oxygenation and metabolism after head injury. Crit Care Med. 2005;33(1):189–95. discussion 255–7.
Samuelsson C, et al. Cerebral glutamine and glutamate levels in relation to compromised energy metabolism: a microdialysis study in subarachnoid hemorrhage patients. J Cereb Blood Flow Metab. 2007;27(7):1309–17.
Strong AJ. The management of plasma glucose in acute cerebral ischaemia and traumatic brain injury: more research needed. Intensive Care Med. 2008;34(7):1169–72.
van den Berghe G, et al. Intensive insulin therapy in the critically ill patients. N Engl J Med. 2001;345(19):1359–67.
Brunkhorst FM, et al. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358(2):125–39.
Oddo M, et al. Impact of tight glycemic control on cerebral glucose metabolism after severe brain injury: a microdialysis study. Crit Care Med. 2008;36(12):3233–8.
Abi-Saab WM, et al. Striking differences in glucose and lactate levels between brain extracellular fluid and plasma in conscious human subjects: effects of hyperglycemia and hypoglycemia. J Cereb Blood Flow Metab. 2002;22(3):271–9.
Zazulia AR, Videen TO, Powers WJ. Transient focal increase in perihematomal glucose metabolism after acute human intracerebral hemorrhage. Stroke. 2009;40(5):1638–43.
Kurtz P, et al. Serum glucose variability and brain-serum glucose ratio predict metabolic distress and mortality after severe brain injury. Crit Care. 2009;13(Suppl 3).
Bederson JB, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke. 2009;40(3):994–1025.
Broderick J, et al. Guidelines for the management of spontaneous intracerebral hemorrhage in adults: 2007 update: a guideline from the American Heart Association/American Stroke Association Stroke Council, High Blood Pressure Research Council, and the Quality of Care and Outcomes in Research Interdisciplinary Working Group. Circulation. 2007; 116(16): e391–413.
Mayberg MR, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage. A statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke. 1994;25(11):2315–28.
Badjatia N, et al. Metabolic benefits of surface counter warming during therapeutic temperature modulation. Crit Care Med. 2009;37(6):1893–7.
Prentice RL, Zhao LP. Estimating equations for parameters in means and covariances of multivariate discrete and continuous responses. Biometrics. 1991;47(3):825–39.
Vespa PM, et al. Persistently low extracellular glucose correlates with poor outcome 6 months after human traumatic brain injury despite a lack of increased lactate: a microdialysis study. J Cereb Blood Flow Metab. 2003;23(7):865–77.
Krinsley JS, Preiser JC. Moving beyond tight glucose control to safe effective glucose control. Crit Care. 2008;12(3):149.
Preiser JC, Devos P. Current status of tight blood sugar control. Curr Infect Dis Rep. 2008;10(5):377–82.
Schlenk F, Vajkoczy P, Sarrafzadeh A. Inpatient hyperglycemia following aneurysmal subarachnoid hemorrhage: relation to cerebral metabolism and outcome. Neurocrit Care. 2009.
Schlenk F, Sarrafzadeh AS. Is continuous insulin treatment safe in aneurysmal subarachnoid hemorrhage? Vasc Health Risk Manag. 2008;4(4):885–91.
Latorre JG, et al. Effective glycemic control with aggressive hyperglycemia management is associated with improved outcome in aneurysmal subarachnoid hemorrhage. Stroke. 2009;40(5):1644–52.
Fabricius M, et al. Cortical spreading depression and peri-infarct depolarization in acutely injured human cerebral cortex. Brain. 2006;129(Pt 3):778–90.
Strong AJ, et al. Spreading and synchronous depressions of cortical activity in acutely injured human brain. Stroke. 2002;33(12):2738–43.
Dreier JP, et al. Delayed ischaemic neurological deficits after subarachnoid haemorrhage are associated with clusters of spreading depolarizations. Brain. 2006;129(Pt 12):3224–37.
Hopwood SE, et al. Transient changes in cortical glucose and lactate levels associated with peri-infarct depolarisations, studied with rapid-sampling microdialysis. J Cereb Blood Flow Metab. 2005;25(3):391–401.
Acknowledgments
We thank the attendings, fellows and nurses of the Neuroscience ICU for their overall support of this project. We thank Martina Pavlicova, PhD, Department of Biostatistics Columbia University for statistical review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Helbok, R., Schmidt, J.M., Kurtz, P. et al. Systemic Glucose and Brain Energy Metabolism after Subarachnoid Hemorrhage. Neurocrit Care 12, 317–323 (2010). https://doi.org/10.1007/s12028-009-9327-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-009-9327-4