Abstract
Background
In past research, procalcitonin (PCT) and glial fibrillary acidic protein (GFAP) have been reported to be useful biomarkers in predicting neurological outcome after the return of spontaneous circulation (ROSC) following out-of-hospital cardiac arrest (CA), although they have only been studied separately. In this study, we compared the usefulness of PCT and GFAP in predicting neurological outcome.
Methods
This study was a retrospective, single-center analysis, conducted in the intensive-care unit of a university hospital. Twenty-one sequential post-CA patients were included. Serum samples were collected from patients at 12 and 24 h after ROSC. Serum PCT and GFAP were measured and compared in patients with favorable and unfavorable neurological outcomes, evaluated at 6 months using the Glasgow–Pittsburgh Cerebral Performance Categories.
Results
Serum PCT was significantly higher at 12 and 24 h in patients with unfavorable outcomes (P = 0.004 and 0.002, respectively). Serum GFAP was not significantly higher at 12 and 24 h in patients with unfavorable outcomes (P = 0.118 and 0.079, respectively). The combination of PCT and GFAP showed high predictive value for unfavorable outcomes (86.7% sensitivity and 100% specificity at 12 h; 100% sensitivity and 83.3% specificity at 24 h).
Conclusion
Serum PCT is a marker of unfavorable neurological outcome in post-CA patients, and is superior to serum GFAP in the early phase.
Similar content being viewed by others
Introduction
Although no predictive markers of neurological outcome in patients with postresuscitation encephalopathy have been unanimously established in routine clinical practice, serum procalcitonin (PCT) and glial fibrillary acidic protein (GFAP) have been separately reported to be new prognostic biomarkers of neurological outcome [1, 2]. PCT is a serum inflammatory marker in patients with sepsis, whereas the post-cardiac-arrest (CA) status is designated “sepsis-like” syndrome [3, 4]. GFAP is a specific marker in traumatic brain injury patients, and is reported to be an exclusively brain-derived protein [5, 6]. In the clinical context, an outcome-predictive marker must have high specificity in the early phase. In this regard, previous reports have shown that both PCT and GFAP have predictive value within 24 h [1, 2]. Therefore, both markers could be candidate prognostic markers.
In this pilot study, we measured the serum levels of PCT and GFAP in the same sample of patients who had received cardiopulmonary resuscitation (CPR), to investigate their predictive capacities for neurological outcome and their clinical utility.
Methods
Patients and Treatment Protocols
The protocol used in this clinical study was approved by the Institutional Review Board of Yamaguchi university hospital. The study was designed as a retrospective study. The group of patients with out-of-hospital cardiac arrest (CA) were selected by remaining stocked serum samples from previous study [2], and 21 patients were finally enrolled in the study.
Participation in the clinical study did not alter any aspect of the management of the patients. The PCA patients were sedated (midazolam 0.1–0.2 mg/kg/h and butorphanol tartrate 0.01–0.02 mg/kg/h or fentanyl 1 μg/kg/h) for at least 48 h and mechanically ventilated with a muscle relaxant (vecuronium 0.05 mg/kg/h). Their blood pressure was maintained (systolic blood pressure >90 mmHg and mean arterial pressure >70 mmHg). Core body temperature was measured using a bladder probe and hypothermia treatment was applied with a cooling blanket (Blanketrol, Cincinnati Sub-Zero, Cincinnati, OH, USA) or an intravascular cooling device (Coolgard, Alsius Inc., Irvine, CA, USA). If cerebral herniation was diagnosed by pupil assessment, electroencephalogram, auditory brainstem response, or head computed tomography (CT), we stopped the management protocol and tested for brain death according to the Japanese criteria (whole-brain death).
Sample Collection and Assays
Clinical data were recorded, including the time course from CPA to ROSC, the etiology, and the initial rhythm. The neurological outcome at 6 months after ROSC was assessed using the Glasgow–Pittsburgh Cerebral Performance Categories (CPC), which includes five categories [7]. Detailed information on the neurological outcome was given by the patient’s present attending physician or our staff, who were blind to the PCT and GFAP data, and the CPC was determined. A favorable neurological outcome was defined as CPC 1 (good recovery) or CPC 2 (moderate disability), whereas an unfavorable outcome was defined as CPC 3 (severe disability), CPC 4 (persistent vegetative state), or CPC 5 (death). Patients with CPC 1–2 had sufficient cerebral function to live independently and work at least part-time.
Blood samples were collected from an arterial line in the course of routine intensive care at 12 and 24 h after ROSC, and were allowed to clot for 30 min at 4°C. The blood was centrifuged at 3,000 rpm for 10 min at 4°C and the supernatant was stored at −80°C until analysis. Serum levels of PCT were measured with a chemiluminescent enzyme immunoassay with the SphereLight-Brahms PCT (Wako Pure Chemical Industries, Osaka, Japan). The assay detection limit of this kit was 0.10 ng/ml; all values below this limit were defined as 0.10 ng/ml. Serum levels of GFAP were analyzed with an enzyme-linked immunosorbent assay (ELISA) (BioVendor, Candler, Texas, USA) with a detection limit of 0.10 ng/ml; values below 0.10 ng/ml were expressed as 0.10 ng/ml. Although we gathered blood samples according to the protocol for this study, measurements could not be made in some cases because of a lack of sample volume. It has been reported that the upper normal limit for PCT is 0.50 ng/ml; that for GFAP is 0.10 ng/ml [2, 8].
Statistical Analysis
Statistical analysis was performed using the statistical software program SPSS, version 16.0 (SPSS Inc., Chicago, IL, USA). Continuous variables are expressed as medians and interquartile ranges, and categorical variables are expressed as counts and percentages. Statistical comparisons of continuous variables were analyzed using the Mann–Whitney U test, as appropriate. Statistical comparisons of categorical variables were analyzed using the Fisher exact test or the χ2 test, as appropriate. Sensitivity and specificity were calculated from receiver operating characteristic (ROC) curves. The cutoff value was defined as the upper normal limit for each marker (PCT, 0.50 ng/ml; GFAP, 0.10 ng/ml). A value of P < 0.05 was considered statistically significant. Combination of PCT and GFAP were also analyzed to investigate the predictability with no false positives.
Results
The patients were admitted to our emergency medical center, between September 2001 and August 2006, is shown in Fig. 1. Among 503 patients, 129 achieved a return of spontaneous circulation (ROSC). When the exclusion criteria (shown in Fig. 1) were applied, 39 patients were eligible patients in this term.
Patient enrolment. Between September 2001 and August 2006, 503 patients with out-of-hospital cardiac arrest were admitted to our emergency center. One hundred and 29 patients achieved a return of spontaneous circulation, and 19 patients of them were eligible after the exclusion criteria were applied (such as trauma, extracorporeal CPR, severe stroke on initial head CT). However, 18 patients were not obtained informed consent or were not collected complete serum samples. Thus, 21 patients were ultimately enrolled in the study
The patients were divided into two groups: favorable outcome (CPC 1–2) and unfavorable outcome (CPC 3–5). The characteristics of each group are listed in Table 1. There were 6 patients in CPC 1, 1 in CPC 3, 12 in CPC 4, and 2 in CPC5. Significant difference between the two groups was observed in the period from the start of CPR to ROSC (P = 0.005) and the initial electrocardiographic rhythm (P = 0.025).
Figure 2 shows a scatter diagram of the individual serum levels of PCT and GFAP in the favorable and unfavorable outcome groups, 12 and 24 h after ROSC. Serum PCT was significantly higher in the unfavorable outcome group than in the favorable outcome group at both time points (P = 0.004 and 0.002, respectively). There were no significant differences between the two groups in the levels of GFAP (at 12 h, P = 0.118; at 24 h, P = 0.079).
a Scatter chart of the serum concentrations of PCT in the favorable and unfavorable outcome groups. The limit of detection for serum PCT in this study was 0.1 ng ml−1; values below this limit are expressed as 0.1 ng ml−1 in the chart. There were significant differences between the two groups at 12 and 24 h after ROSC (P = 0.004 and 0.002, respectively). b Scatter chart of the serum concentrations of GFAP in the favorable and unfavorable outcome groups. The limit of detection for serum GFAP in this study was 0.1 ng ml−1; values below this limit are expressed as 0.1 ng ml−1 in the chart. There were no significant differences between the two groups at 12 and 24 h after ROSC (P = 0.118 and 0.079, respectively)
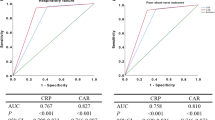
Figure 3 and Table 2 show the ROC analyses of PCT and GFAP for an unfavorable outcome at 12 and 24 h. PCT had significant areas under the ROC curve (AUC) of 0.911 and 0.939 at 12 and 24 h, respectively, after ROSC (P = 0.004 and 0.002, respectively), and both the sensitivity and specificity exceeded 70% with a cutoff value of 0.50 ng/ml. The AUCs for GFAP were 0.667 and 0.700 at 12 and 24 h, respectively, but were not significantly different. GFAP showed 100% specificity at 12 and 24 h with a cutoff value of 0.10 ng/ml.
Receiver operating characteristic (ROC) curves for serum PCT at 12 h (solid line) and 24 h (dotted line), and for GFAP at 12 h (short-dashed line) and at 24 h (long-dashed line) for unfavorable outcome. The areas under the ROC curves, and their sensitivity and specificity are listed in Table 2
Table 3A and B lists a classification according to positive/negative PCT and GFAP of patients with favorable and unfavorable outcomes. At 12 h after ROSC, all patients with favorable outcomes were negative for PCT and GFAP, and two patients with unfavorable outcome were negative for PCT and GFAP. At 24 h after ROSC, all patients with unfavorable outcome were positive for PCT and/or GFAP. One patient with a favorable outcome was positive for PCT at 24 h, but negative for GFAP. Either positive PCT or positive GFAP predicted an unfavorable outcome with 86.7% sensitivity and 100% specificity at 12 h, and 100% sensitivity and 83.3% specificity at 24 h.
Discussion
In the present study, inflammatory and astrocyte-derived markers, respectively, PCT and GFAP in the blood were investigated as useful predictive biomarkers for neurological outcome in post-CA patients. Serum PCT was significant higher in the unfavorable outcome group than in the favorable outcome group (P = 0.004 at 12 h, P = 0.002 at 24 h; Fig. 2a). Patients with an apparently infectious focus were not enrolled; therefore, PCT might be a useful biomarker for the early detection of unfavorable neurological outcome. Serum GFAP was not significantly different between the two groups (P = 0.118 at 12 h, P = 0.079 at 24 h), but GFAP was not elevated at all in patients with favorable outcomes (Fig. 2b). Therefore, GFAP might be a specific predictor of an unfavorable outcome. The elevation of each marker (positive values: PCT >0.5 ng/ml, GFAP >0.1 ng/ml) indicated different populations of patients with unfavorable outcomes, when the classification was considered (Table 3).
In the ROC analysis, the area under the ROC curve and its sensitivity showed that PCT was superior to GFAP in predicting an unfavorable neurological outcome (Table 2; Fig. 3). However, one patient in the favorable outcome group was positive for PCT at 24 h (Table 3; Fig. 2), and this patient had acute respiratory distress syndrome (ARDS) at that time. PCT was originally used as a marker to predict the patient’s inflammatory status during sepsis [9]. Therefore, PCT at 24 h might be modified by the patient’s inflammatory status, caused by “sepsis-like” syndrome [4]. It is also possible that ventilator-associated pneumonia in PCA patients after ROSC or accidental aspiration in the resuscitation period could increase PCT in the early phase [10]. The present data, combined with these earlier reports, suggest that the predictive value of PCT might not be as effective at 24 h after ROSC as at 12 h. Although PCT is a sensitive representative early-phase inflammatory marker, the value of PCT 24 h after ROSC in predicting neurological outcome could be affected by systemic inflammation.
In this study, serum GFAP did not show sufficient sensitivity in predicting an unfavorable neurological outcome (Fig. 3). The representative brain-specific markers are neuron-specific enolase (NSE) and S-100B protein [11–13]. Several animal experimental models have shown that serum NSE and S-100B are also increased without brain injury after hemorrhagic shock, femur fracture, and local ischemia and reperfusion of the liver, kidney, and gut [14, 15]. This means that NSE and S-100B have significant limitations in terms of brain specificity in the evaluation of neurological outcome in patients with these pathophysiological states. Conversely, it has been reported that the brain specificity of GFAP is very high [5, 16], meaning that GFAP could be an eligible brain-specific biomarker predicting neurological outcome. In fact, increased GFAP had 100% specificity for brain damage in the present study (Table 2).
The predictive marker used to decide the withdrawal of therapy must be sufficiently specific. In this study, we demonstrated that serum PCT and GFAP could detect different populations in the unfavorable outcome group (Table 2). It has been reported that a combination of a serum marker and the Glasgow Coma Scale improved the reliability of neurological outcome prediction [11]. In our study, when serum markers with different underlying mechanisms were combined, the reliability of the prediction was improved, with 100% specificity 12 h after ROSC. When both predictive markers were combined, either the PCT- or GFAP-positive subgroup reached 86.7% sensitivity and 100% specificity 12 h after ROSC, and 100% sensitivity and 83.3% specificity at 24 h. Although the combination of PCT and GFAP had high sensitivity (86.7%) and 100% specificity, two patients with unfavorable outcomes were both negative for PCT and GFAP (Table 3). These two patients had cardiogenic cardiac arrest, with a period of 10 min from collapse to the start of CPR. The neurological outcomes of these patients, who received ideal resuscitation, could not be predicted by a combination of PCT and GFAP.
This study has a number of limitations. First, the number of patients was small. However, our data showed high sensitivity and specificity, especially those for serum PCT. Second, the blood sampling points were not optimal for a diagnosis in the clinical context. In this study, the diagnostic value of PCT and GFAP was evaluated at 12 and 24 h, but a more appropriate time point may exist. Third, seven patients (33%) were treated with therapeutic hypothermia. Given that NSE and S-100B are affected by therapeutic hypothermia [9], PCT and GFAP might also be affected by this treatment. This possibility should be investigated in a future study.
Conclusion
Serum PCT and GFAP were elevated in patients with unfavorable neurological outcomes after CA. Serum PCT (>0.5 ng/ml) was better than serum GFAP (>0.1 ng/ml) in predicting an unfavorable neurological outcome in post-CA patients.
References
Fries M, Kunz D, Gressner AM, Rossaint R, Kuhlen R. Procalcitonin serum levels after out-of-hospital cardiac arrest. Resuscitation. 2003;59:105–9.
Kaneko T, Kasaoka S, Miyauchi T, et al. Serum glial fibrillary acidic protein as a predictive biomarker of neurological outcome after cardiac arrest. Resuscitation. 2009;80:790–4.
Tang BM, Eslick GD, Craig JC, McLean AS. Accuracy of procalcitonin for sepsis diagnosis in critically ill patients: systematic review and meta-analysis. Lancet Infect Dis. 2007;7:210–7.
Adrie C, Adib-Conquy M, Laurent I, et al. Successful cardiopulmonary resuscitation after cardiac arrest as a “sepsis-like” syndrome. Circulation. 2002;106:562–8.
Pelinka LE, Kroepfl A, Schmidhammer R, et al. Glial fibrillary acidic protein in serum after traumatic brain injury and multiple trauma. J Trauma. 2004;57:1006–12.
Pelinka LE, Kroepfl A, Leixnering M, Buchinqer W, Raabe A, Redl H. GFAP versus S100B in serum after traumatic brain injury: relationship to brain damage and outcome. J Neurotrauma. 2004;21:1553–61.
Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1:480–4.
Brunkhorst FM, Wegscheider K, Forycki ZF, Brunkhorst R. Procalcitonin for early diagnosis and differentiation of SIRS, sepsis, severe sepsis, and septic shock. Intensive Care Med. 2000;26:S148–52.
Tiainen M, Roine RO, Pettilä V, Takkunen O. Serum neuron-specific enolase and S-100B protein in cardiac arrest patients treated with hypothermia. Stroke. 2003;34:2881–6.
Oppert M, Reinicke A, Müller C, Barckow D, Frei U, Eckardt KU. Elevations in procalcitonin but not C-reactive protein are associated with pneumonia after cardiopulmonary resuscitation. Resuscitation. 2002;53:167–70.
Pfeifer R, Börner A, Krack A, Siqusch HH, Suber R, Fiqulla HR. Outcome after cardiac arrest: predictive value and limitations of the neuroproteins neuron-specific enolase and protein S-100 and the Glasgow coma scale. Resuscitation. 2005;65:49–55.
Böttiger BW, Möbes S, Glätzer R, et al. Astroglial protein S-100 is an early and sensitive marker of hypoxic brain damage and outcome after cardiac arrest in humans. Circulation. 2001;103:2694–8.
Hachimi-Idrissi S, Van derAuwera M, Schiettecatte J, Ebinger G, Michotte Y, Huyghens L. S-100 protein as early predictor of regaining consciousness after out of hospital cardiac arrest. Resuscitation. 2002;53:251–7.
Pelinka LE, Hertz H, Mauritz W, et al. Nonspecific increase of systemic neuron-specific enolase after trauma: clinical and experimental findings. Shock. 2005;24:119–23.
Pelinka LE, Harada N, Szalay L, Jafarmadar M, Redl H, Bahrami S. Release of S100B differs during ischemia and reperfusion of the liver, the gut, and the kidney in rats. Shock. 2004;21:72–6.
Kaneko T, Yagi T, Todani M, et al. Serum glial fibrillary acidic protein has remarkable diagnostic value on traumatic brain injury in multiple trauma patients. Crit Care Med. 2008;36:47.
Acknowledgments
This clinical study was supported by a research project grant from the Japanese Ministry of Health, Labor, and Welfare (number 19791329). We are grateful to Hitomi Ikemoto for her valuable technical assistance in all measurements. We also express our thanks to Masako Ueda for assistance in completing the grant-related paperwork.
Conflict of Interest Statement
This study was conducted independently of the funding bodies, except for a governmental grant. This grant had no influence on the decisions relating to the study design or publication.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hayashida, H., Kaneko, T., Kasaoka, S. et al. Comparison of the Predictability of Neurological Outcome by Serum Procalcitonin and Glial Fibrillary Acidic Protein in Postcardiac-Arrest Patients. Neurocrit Care 12, 252–257 (2010). https://doi.org/10.1007/s12028-009-9318-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-009-9318-5