Abstract
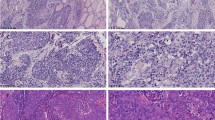
Intrathyroid thymic carcinoma (ITTC) is a rare malignant neoplasm considered to be a eutopic thymic carcinoma (TC) arising ectopically in the thyroid. Histopathologically, ITTC resembles squamous cell carcinoma of the thymus with positive TC markers such as CD5 and c-KIT. Despite these similar histological findings, ITTC is clinically less aggressive than TC. In this study, we compared clinical, histological, and genetic characteristics of ITTCs and TCs. We collected 9 ITTCs and 8 TCs with their clinicopathological profiles. Immunohistochemistry for CD5, p63, CD117/c-KIT, Ki-67, p53, TTF-1, thyroglobulin, PAX8, EGFR, and PD-L1/CD274 plus in situ hybridization for EBER was performed. We further investigated mutation status of KIT, EGFR, BRAF, and TERT promoter using Sanger sequencing. In our study, ITTCs affected significantly younger patients than TCs. After a mean follow-up of 86 months, all patients with ITTC were alive, while two patients with TC had died. Immunohistochemistry showed ITTCs and TCs had a similar immunophenotype except for EGFR and p53. Genetic analysis did not identify KIT or BRAF mutations in any ITTCs or TCs. EGFR mutations were positive in 11% (1/9) of ITTCs and 25% (2/8) of TCs. Notably, TERT promoter C228T mutation was identified in 22% (2/9) of ITTCs but none of the TCs. There were no significant differences in age, tumor size, or sex between TERT-mutated and TERT-wild-type ITTCs. Collectively, ITTC and TC have similar histopathologic and immunophenotypic features but different clinical outcomes. Recurrent TERT promoter mutation may be a key event related to cancer progression in ITTCs and warrants further investigation.



Similar content being viewed by others
Data Availability
All data generated or analyzed during this study are included in this article and its supplementary information files.
References
Dong W, Zhang P, Li J, et al (2018) Outcome of Thyroid Carcinoma Showing Thymus-Like Differentiation in Patients Undergoing Radical Resection. World J Surg 42:1754–1761. https://doi.org/10.1007/s00268-017-4339-2
Miyauchi A, Kuma K, Matsuzuka F, et al (1985) Intrathyroidal epithelial thymoma: An entity distinct from squamous cell carcinoma of the thyroid. World J Surg 9:128–134. https://doi.org/10.1007/BF01656263
Chan JKC RJ (1991) Tumors of the neck showing thymic or related branchial pouch differentiation: a unifying concept. Hum Pathol 22:349–367. https://doi.org/10.1016/j.jdcr.2019.02.021
Lloyd RV, Osamura RY, Klöppel G RJ (eds) (2017) World Health Organization Classification of Tumours of Endocrine Organs (4th). IARC, Lyon
Berezowski K, Grimes MM, Gal A, Kornstein MJ (1996) CD5 immunoreactivity of epithelial cells in thymic carcinoma and CASTLE using paraffin-embedded tissue. Am J Clin Pathol 106:483–486. https://doi.org/10.1093/ajcp/106.4.483
Dorfman, Shahsafaei, Miyauchi (1998) Intrathyroidal epithelial thymoma (ITET)/carcinoma showing thymus-like differentiation (CASTLE) exhibits CD5 immunoreactivity: new evidence for thymic differentiation. Histopathology 32:104–109. https://doi.org/10.1046/j.1365-2559.1998.00318.x
Roka S, Kornek G, Schüller J, et al (2004) Carcinoma showing thymic-like elements - A rare malignancy of the thyroid gland. Br J Surg 91:142–145. https://doi.org/10.1002/bjs.4510
Cappelli C, Tironi A, Marchetti G Pietro, et al (2008) Aggressive thyroid carcinoma showing thymic-like differentiation (CASTLE): case report and review of the literature. Endocr J 55:685–90. https://doi.org/10.1507/endocrj.K07E-147
Veits L, Mechtersheimer G, Steger C, et al (2011) Chromosomal imbalances in carcinoma showing thymus-like elements (CASTLE). Virchows Arch 459:221–226. https://doi.org/10.1007/s00428-011-1117-7
Hirokawa M, Miyauchi A, Minato H, et al (2013) Intrathyroidal epithelial thymoma/carcinoma showing thymus-like differentiation; comparison with thymic lymphoepithelioma-like carcinoma and a possibility of development from a multipotential stem cell. Apmis 121:523–530. https://doi.org/10.1111/apm.12017
Huang C, Wang L, Wang Y, et al (2013) Carcinoma showing thymus-like differentiation of the thyroid (CASTLE). Pathol Res Pract 209:662–665. https://doi.org/10.1016/j.prp.2013.06.021
Zhu L, Zhang J, Marx A, et al (2016) Clinicopathological analysis of 241 thymic epithelial tumors-Experience in the Shanghai Chest Hospital from 1997-2004. J Thorac Dis 8:718–726. https://doi.org/10.21037/jtd.2016.03.24
Ito Y, Miyauchi A, Nakamura Y, et al (2007) Clinicopathologic significance of intrathyroidal epithelial thymoma/carcinoma showing thymus-like differentiation: A collaborative study with member Institutes of the Japanese Society of Thyroid Surgery. Am J Clin Pathol 127:230–236. https://doi.org/10.1309/VM7E52B6U9Q729DQ
Yoh K, Nishiwaki Y, Ishii G, et al (2008) Mutational status of EGFR and KIT in thymoma and thymic carcinoma. Lung Cancer 62:316–320. https://doi.org/10.1016/j.lungcan.2008.03.013
Weissferdt A, Lin H, Woods D, et al (2012) HER family receptor and ligand status in thymic carcinoma. Lung Cancer 77:515–521. https://doi.org/10.1016/j.lungcan.2012.05.108
Weissferdt A, Wistuba II, Moran CA (2012) Molecular aspects of thymic carcinoma. Lung Cancer 78:127–132. https://doi.org/10.1016/j.lungcan.2012.08.002
Hagemann IS, Govindan R, Javidan-Nejad C, et al (2014) Stabilization of Disease after Targeted Therapy in a Thymic Carcinoma with KIT Mutation Detected by Clinical Next-Generation Sequencing. J Thorac Oncol 9:e12–e16. https://doi.org/10.1097/JTO.0b013e3182a7d22e
Shitara M, Okuda K, Suzuki A, et al (2014) Genetic profiling of thymic carcinoma using targeted next-generation sequencing. Lung Cancer 86:174–179. https://doi.org/10.1016/j.lungcan.2014.08.020
Saito M, Fujiwara Y, Asao T, et al (2017) The genomic and epigenomic landscape in thymic carcinoma. Carcinogenesis 38:1084–1091. https://doi.org/10.1093/carcin/bgx094
Radovich M, Pickering CR, Felau I, et al (2018) The Integrated Genomic Landscape of Thymic Epithelial Tumors. Cancer Cell 33:244-258.e10. https://doi.org/10.1016/j.ccell.2018.01.003
Yuan X, Larsson C, Xu D (2019) Mechanisms underlying the activation of TERT transcription and telomerase activity in human cancer: old actors and new players. Oncogene. https://doi.org/10.1038/s41388-019-0872-9
Huang DS, Wang Z, He XJ, et al (2015) Recurrent TERT promoter mutations identified in a large-scale study of multiple tumour types are associated with increased TERT expression and telomerase activation. Eur J Cancer 51:969–976. https://doi.org/10.1016/j.ejca.2015.03.010
Veits L, Schupfner R, Hufnagel P, et al (2014) KRAS, EGFR, PDGFR-α, KIT and COX-2 status in carcinoma showing thymus-like elements (CASTLE). Disgnostic Pathol 9:. https://doi.org/10.1186/1746-1596-9-116
Rajeshwari M, Singh V, Nambirajan A, et al (2018) Carcinoma showing thymus like elements: report of a case with EGFR T790M mutation. Diagn Cytopathol 46:413–418. https://doi.org/10.1002/dc.23859
Travis, W.D., Brambilla, E., Burke, A.P., Marx, A., Nicholson AG (eds) (2015) World Health Organization Classification of Tumors of the Lung, Pleura, Thymus, and Heart (4th). IARC, Lyon
Kakudo K, Bai Y, Ozaki T, et al (2013) Intrathyroid epithelial thymoma (ITET) and carcinoma showing thymus-like differentiation (CASTLE). CD5-positive neoplasms mimicking squamous cell carcinoma of the thyroid. Histol Histopathol 28:543–556. https://doi.org/10.14670/HH-28.543
Moreira AL, Won HH, Mcmillan R, et al (2015) Massively parallel sequencing identifies recurrent mutations in TP53 in thymic carcinoma associated with poor prognosis. J Thorac Oncol 10:373–380. https://doi.org/10.1097/JTO.0000000000000397
Katsuya Y, Fujita Y, Horinouchi H, et al (2015) Immunohistochemical status of PD-L1 in thymoma and thymic carcinoma. Lung Cancer 88:154–159. https://doi.org/10.1016/j.lungcan.2015.03.003
Oishi N, Kondo T, Mochizuki K, et al (2014) Localized Langerhans cell histiocytosis of the thymus with BRAF V600E mutation: A case report with immunohistochemical and genetic analyses. Hum Pathol 45:1302–1305. https://doi.org/10.1016/j.humpath.2013.12.018
Yano M, Sasaki H, Yokoyama T, et al (2008) Thymic carcinoma: 30 Cases at a single institution. J Thorac Oncol 3:265–269. https://doi.org/10.1097/JTO.0b013e3181653c71
Buti S, Donini M, Sergio P, Garagnani L, Schirosi L, Passalacqua R RG (2011) Impressive response with imatinib in a heavily pretreated patient with metastatic c-KIT mutated thymic carcinoma. JClinOncol 29:803–805. https://doi.org/10.1200/JCO.2012.45.7739
Weksler B, Dhupar R, Parikh V, et al (2013) Thymic carcinoma: A multivariate analysis of factors predictive of survival in 290 patients. Ann Thorac Surg 95:299–303. https://doi.org/10.1016/j.athoracsur.2012.09.006
Ruffini E, Detterbeck F, van Raemdonck D, et al (2014) Thymic carcinoma: A cohort study of patients from the European society of thoracic surgeons database. J Thorac Oncol 9:541–548. https://doi.org/10.1097/JTO.0000000000000128
Gao R, Jia X, Ji T, et al (2018) Management and Prognostic Factors for Thyroid Carcinoma Showing Thymus-Like Elements (CASTLE): A Case Series Study. Front Oncol 8:1–9. https://doi.org/10.3389/fonc.2018.00477
Litvak AM, , Kaitlin Woo, Sara Hayes, James Huang, Andreas Rimner, Camelia S Sima, Andre L Moreira, Maria Tsukazan GJR (2014) Clinical Characteristics and Outcomes for Patients With Thymic Carcinoma: Evaluation of Masaoka Staging. J Thorac Oncol 9:1810–1815. https://doi.org/10.1097/JTO.0000000000000363
Wang YF, Liu B, Fan XS, et al (2015) Thyroid carcinoma showing thymus-like elements: A clinicopathologic, immunohistochemical, ultrastructural, and molecular analysis. Am J Clin Pathol 143:223–233. https://doi.org/10.1309/AJCPB7PS6QHWEFRK
Penzel R, Sers C, Chen Y, et al (2011) EGFR mutation detection in NSCLC-assessment of diagnostic application and recommendations of the German Panel for Mutation Testing in NSCLC. Virchows Arch 458:95–98. https://doi.org/10.1007/s00428-010-1000-y
Ito T, Matoba R, Maekawa H, et al (2019) Detection of gene mutations in gastric cancer tissues using a commercial sequencing panel. Mol Clin Oncol 11:455–460. https://doi.org/10.3892/mco.2019.1926
Murray S, Timotheadou E, Linardou H, et al (2006) Mutations of the epidermal growth factor receptor tyrosine kinase domain and associations with clinicopathological features in non-small cell lung cancer patients. Lung Cancer 52:225–233. https://doi.org/10.1016/j.lungcan.2005.12.015
Diah A Douglas, Hong Zhong, Jae Y Ro, Carole Oddoux, Aaron D Berger, Matthew R Pincus, Jaya M Satagopan, William L Gerald, Howard I Scher, Peng Lee IO (2006) Novel Mutations of Epidermal Growth Factor Receptor in Localized Prostate Cancer. Front Biosci 11:2518–2525. https://doi.org/10.5964/ejop.v13i4.1198
Heidenreich B, Kumar R (2017) TERT promoter mutations in telomere biology. Mutat Res - Rev Mutat Res 771:15–31. https://doi.org/10.1016/j.mrrev.2016.11.002
Xiaoli Liu, Justin Bishop, Yuan Shan, Sara Pai DL (2013) Higyly prevalent TERT promotor mutations in aggressive thyoid cancers. Endocr Relat Cancer 20:603–610. https://doi.org/10.1016/j.biotechadv.2011.08.021.Secreted
Oishi N, Kondo T, Ebina A, et al (2017) Molecular alterations of coexisting thyroid papillary carcinoma and anaplastic carcinoma: Identification of TERT mutation as an independent risk factor for transformation. Mod Pathol 30:1527–1537. https://doi.org/10.1038/modpathol.2017.75
Hysek M, Paulsson JO, Jatta K, et al (2019) Clinical routine tert promoter mutational screening of follicular thyroid tumors of uncertain malignant potential (Ft-umps): A useful predictor of metastatic disease. Cancers (Basel) 11:1–10. https://doi.org/10.3390/cancers11101443
Censi S, Barollo S, Grespan E, et al (2019) Prognostic significance of TERT promoter and BRAF mutations in TIR-4 and TIR-5 thyroid cytology. Eur J Endocrinol 181:1–11. https://doi.org/10.1530/EJE-19-0073
Acknowledgments
We wish to thank Pam Zaber of Editdoc English Editing for her help with English editing of this article. We appreciate Ms. Wakaba Iha, Mr. Yoshihito Koshimizu, and Ms. Kayoko Kono for their technical assistance.
Code Availability
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethics Approval
This study was conducted under the approval of the Institutional Ethical Review Board of University of Yamanashi (approval code: 1723).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tahara, I., Oishi, N., Mochizuki, K. et al. Identification of Recurrent TERT Promoter Mutations in Intrathyroid Thymic Carcinomas. Endocr Pathol 31, 274–282 (2020). https://doi.org/10.1007/s12022-020-09635-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12022-020-09635-0