Abstract
Invasion of the cavernous sinus by pituitary adenomas impedes complete surgical resection, compromises biochemical remission, and increases the risk of further tumor recurrence. Accurate preoperative MRI-based diagnosis or intraoperative direct inspection of cavernous sinus invasion are essential for optimal surgical planning and for tailoring postoperative therapeutic strategies, depending on whether a total resection has been achieved, or tumoral tissue has been left in surgically inaccessible locations. The molecular mechanisms underlying the invasive behavior of pituitary adenomas remain poorly understood, hindering the development of targeted therapies. Some studies have identified genes overexpressed in pituitary adenomas invading the cavernous sinus, offering insights into the acquisition of invasive behavior. Their main limitation however lies in comparing purely intrasellar specimens obtained from invasive and non-invasive adenomas. Further, precise anatomical knowledge of the medial wall of the cavernous sinus is crucial for grasping the mechanisms of invasion. Recently, alongside the standard intrasellar surgery, extended endoscopic intracavernous surgical procedures with systematic selective resection of the medial wall of the cavernous sinus have shown promising results for invasive secreting pituitary adenomas. The first- and second-generation somatostatin agonist ligands and cabergoline are used with variable efficacy to control secretory activity and/or growth of intracavernous remnants. Tumor regrowth usually requires surgical reintervention, sometimes combined with radiotherapy or radiosurgery which is applied despite their benign nature. Unraveling the molecular pathways driving invasive behavior of pituitary adenomas and their tropism to the cavernous sinuses is the key for developing efficient innovative treatment modalities that could reduce the need for repeated surgery or radiotherapy.


Similar content being viewed by others
References
A.S.G. Micko, A. Wöhrer, S. Wolfsberger, E. Knosp, Invasion of the cavernous sinus space in pituitary adenomas: endoscopic verification and its correlation with an MRI-based classification. J. Neurosurg. 122(4), 803–811 (2015). https://doi.org/10.3171/2014.12.JNS141083
K. Juraschka, O.H. Khan, B.L. Godoy et al., Endoscopic endonasal transsphenoidal approach to large and giant pituitary adenomas: institutional experience and predictors of extent of resection. J. Neurosurg. 121(1), 75–83 (2014). https://doi.org/10.3171/2014.3.JNS131679
S. Brochier, F. Galland, M. Kujas et al., Factors predicting relapse of nonfunctioning pituitary macroadenomas after neurosurgery: a study of 142 patients. Eur. J. Endocrinol. 163(2), 193–200 (2010). https://doi.org/10.1530/EJE-10-0255
G. Raverot, E. Dantony, J. Beauvy et al., Risk of recurrence in pituitary neuroendocrine tumors: a prospective study using a five-tiered classification. J. Clin. Endocrinol. Metab. 102(9), 3368–3374 (2017). https://doi.org/10.1210/jc.2017-00773
M. Rutkowski, G. Zada, Management of pituitary adenomas invading the cavernous sinus. Neurosurg. Clin. 30(4), 445–455 (2019). https://doi.org/10.1016/j.nec.2019.05.005
M. Araujo-Castro, A. Acitores Cancela, C. Vior, E. Pascual-Corrales, V. Rodríguez Berrocal, Radiological Knosp, revised-Knosp, and Hardy–Wilson classifications for the prediction of surgical outcomes in the endoscopic endonasal surgery of pituitary adenomas: study of 228 cases. Front. Oncol. 11 (2022). https://www.frontiersin.org/articles/10.3389/fonc.2021.807040
E. Knosp, E. Steiner, K. Kitz, C. Matula, Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery 33(4), 610–617 (1993). https://doi.org/10.1227/00006123-199310000-00008.
H. Nishioka, N. Fukuhara, K. Horiguchi, S. Yamada, Aggressive transsphenoidal resection of tumors invading the cavernous sinus in patients with acromegaly: predictive factors, strategies, and outcomes. J. Neurosurg. 121(3), 505–510 (2014). https://doi.org/10.3171/2014.3.JNS132214
A. Micko, J. Oberndorfer, W.J. Weninger et al., Challenging Knosp high-grade pituitary adenomas. J. Neurosurg. 132(6), 1739–1746 (2019). https://doi.org/10.3171/2019.3.JNS19367
F. Eisenhut, M.A. Schmidt, M. Buchfelder, A. Doerfler, S.M. Schlaffer, Improved detection of cavernous sinus invasion of pituitary macroadenomas with ultra-high-field 7 T MRI. Life13(1), 49 (2022). https://doi.org/10.3390/life13010049
H.Q. Truong, S. Lieber, E. Najera, J.T. Alves-Belo, P.A. Gardner, J.C. Fernandez-Miranda, The medial wall of the cavernous sinus. Part 1: surgical anatomy, ligaments, and surgical technique for its mobilization and/or resection. J. Neurosurg. 131(1), 122–130 (2018). https://doi.org/10.3171/2018.3.JNS18596
S. Cohen-Cohen, P.A. Gardner, J.T. Alves-Belo et al., The medial wall of the cavernous sinus. Part 2: selective medial wall resection in 50 pituitary adenoma patients. J. Neurosurg. 131(1), 131–140 (2018). https://doi.org/10.3171/2018.5.JNS18595
A. Mohyeldin, L.J. Katznelson, A.R. Hoffman et al., Prospective intraoperative and histologic evaluation of cavernous sinus medial wall invasion by pituitary adenomas and its implications for acromegaly remission outcomes. Sci. Rep. 12(1), 9919 (2022). https://doi.org/10.1038/s41598-022-12980-1
S. Dhandapani, H. Singh, H.M. Negm, S. Cohen, V.K. Anand, T.H. Schwartz, Cavernous sinus invasion in pituitary adenomas: systematic review and pooled data meta-analysis of radiologic criteria and comparison of endoscopic and microscopic surgery. World Neurosurg. 96, 36–46 (2016). https://doi.org/10.1016/j.wneu.2016.08.088
G.F. Woodworth, K.S. Patel, B. Shin et al., Surgical outcomes using a medial-to-lateral endonasal endoscopic approach to pituitary adenomas invading the cavernous sinus. J. Neurosurg. 120(5), 1086–1094 (2014). https://doi.org/10.3171/2014.1.JNS131228
A. Paluzzi, J.C. Fernandez-Miranda, S. Tonya Stefko, S. Challinor, C.H. Snyderman, P.A. Gardner, Endoscopic endonasal approach for pituitary adenomas: a series of 555 patients. Pituitary 17(4), 307–319 (2014). https://doi.org/10.1007/s11102-013-0502-4
C.P. Hofstetter, M.J. Nanaszko, L.L. Mubita, J. Tsiouris, V.K. Anand, T.H. Schwartz, Volumetric classification of pituitary macroadenomas predicts outcome and morbidity following endoscopic endonasal transsphenoidal surgery. Pituitary 15(3), 450–463 (2012). https://doi.org/10.1007/s11102-011-0350-z
M. Messerer, J.C. De Battista, G. Raverot et al., Evidence of improved surgical outcome following endoscopy for nonfunctioning pituitary adenoma removal. Neurosurg. Focus 30(4), E11 (2011). https://doi.org/10.3171/2011.1.FOCUS10308
K. Asmaro, M. Zhang, A.J. Rodrigues et al., Cytodifferentiation of pituitary tumors influences pathogenesis and cavernous sinus invasion. J. Neurosurg. 1, 1–9 (2023). https://doi.org/10.3171/2023.3.JNS221949
R. Fahlbusch, M. Buchfelder, Current management of invasive pituitary adenomas. Contemp. Neurosurg. 11(17), 1 (1989)
H.Y. Liu, W.J. Gu, C.Z. Wang, X.J. Ji, Y.M. Mu, Matrix metalloproteinase-9 and -2 and tissue inhibitor of matrix metalloproteinase-2 in invasive pituitary adenomas. Medicine 95(24), e3904 (2016). https://doi.org/10.1097/MD.0000000000003904
J. Gong, Y. Zhao, R. Abdel-Fattah et al., Matrix metalloproteinase-9, a potential biological marker in invasive pituitary adenomas. Pituitary 11(1), 37–48 (2008). https://doi.org/10.1007/s11102-007-0066-2
H. Kawamoto, T. Uozumi, K. Kawamoto, K. Arita, T. Yano, T. Hirohata, Type IV collagenase activity and cavernous sinus invasion in human pituitary adenomas. Acta Neurochir. 138(4), 390–395 (1996). https://doi.org/10.1007/BF01420300
M.D. Ilie, A. Vasiljevic, P. Bertolino, G. Raverot, Biological and therapeutic implications of the tumor microenvironment in pituitary adenomas. Endocr. Rev. 44(2), 297–311 (2023). https://doi.org/10.1210/endrev/bnac024
M.D. Ilie, A. Vasiljevic, G. Raverot, P. Bertolino, The microenvironment of pituitary tumors—biological and therapeutic implications. Cancers 11(10), 1605 (2019). https://doi.org/10.3390/cancers11101605
U.J. Knappe, C. Hagel, B.W. Lisboa, W. Wilczak, D.K. Lüdecke, W. Saeger, Expression of serine proteases and metalloproteinases in human pituitary adenomas and anterior pituitary lobe tissue. Acta Neuropathol. 106(5), 471–478 (2003). https://doi.org/10.1007/s00401-003-0747-5
F. Galland, L. Lacroix, P. Saulnier et al., Differential gene expression profiles of invasive and non-invasive non-functioning pituitary adenomas based on microarray analysis. Endocr. Relat. Cancer 17(2), 361–371 (2010). https://doi.org/10.1677/ERC-10-0018
M. Sato, R. Tamura, H. Tamura et al., Analysis of tumor angiogenesis and immune microenvironment in non-functional pituitary endocrine tumors. J. Clin. Med. 8(5), 695 (2019). https://doi.org/10.3390/jcm8050695
C. Shi, Z. Ye, J. Han et al., BRD4 as a therapeutic target for nonfunctioning and growth hormone pituitary adenoma. Neuro Oncol. 22(8), 1114–1125 (2020). https://doi.org/10.1093/neuonc/noaa084
M. Hage, S. Viengchareun, E. Brunet et al., Genomic alterations and complex subclonal architecture in sporadic GH-secreting pituitary adenomas. J. Clin. Endocrinol. Metab. 103(5), 1929–1939 (2018). https://doi.org/10.1210/jc.2017-02287
R.A. Burrell, N. McGranahan, J. Bartek, C. Swanton, The causes and consequences of genetic heterogeneity in cancer evolution. Nature 501(7467), 338–345 (2013). https://doi.org/10.1038/nature12625
G. Raverot, M.D. Ilie, H. Lasolle et al., Aggressive pituitary tumours and pituitary carcinomas. Nat. Rev. Endocrinol. 17(11), 671–684 (2021). https://doi.org/10.1038/s41574-021-00550-w
P. Marques, S. Barry, E. Carlsen et al., The role of the tumour microenvironment in the angiogenesis of pituitary tumours. Endocrine 70(3) (2020). https://doi.org/10.1007/s12020-020-02478-z
P. Marques, S. Barry, E. Carlsen et al., Chemokines modulate the tumour microenvironment in pituitary neuroendocrine tumours. Acta Neuropathol. Commun. 7(1), 172 (2019). https://doi.org/10.1186/s40478-019-0830-3
S. Barry, E. Carlsen, P. Marques et al., Tumor microenvironment defines the invasive phenotype of AIP-mutation-positive pituitary tumors. Oncogene 38(27), 5381–5395 (2019). https://doi.org/10.1038/s41388-019-0779-5
M.D. Ilie, H. Lasolle, G. Raverot, Emerging and novel treatments for pituitary tumors. J. Clin. Med. 8(8), 1107 (2019). https://doi.org/10.3390/jcm8081107
K. Osterhage, R. Rotermund, M. Droste et al., Bevacizumab in aggressive pituitary adenomas – experience with 3 patients. Exp. Clin. Endocrinol. Diabetes 129(3), 178–185 (2021). https://doi.org/10.1055/a-1260-3975
O.M. Alshaikh, S.L. Asa, O. Mete, S. Ezzat, An institutional experience of tumor progression to pituitary carcinoma in a 15-year cohort of 1055 consecutive pituitary neuroendocrine tumors. Endocr. Pathol. 30(2), 118–127 (2019). https://doi.org/10.1007/s12022-019-9568-5
M.D. Ilie, A. Vasiljevic, E. Jouanneau, G. Raverot, Immunotherapy in aggressive pituitary tumors and carcinomas: a systematic review. Endocr. Relat. Cancer 29(7), 415–426 (2022). https://doi.org/10.1530/ERC-22-0037
M.D. Ilie, C. Villa, T. Cuny et al., Real-life efficacy and predictors of response to immunotherapy in pituitary tumors: a cohort study. Eur. J. Endocrinol. 187(5), 685–696 (2022). https://doi.org/10.1530/EJE-22-0647
S. Yokoyama, H. Hirano, K. Moroki, M. Goto, S. Imamura, J.I. Kuratsu, Are nonfunctioning pituitary adenomas extending into the cavernous sinus aggressive and/or invasive? Neurosurgery 49(4), 857–862 (2001). https://doi.org/10.1097/00006123-200110000-00014.
A. Yasuda, A. Campero, C. Martins, A.L.J. Rhoton, G.C. Ribas, The medial wall of the cavernous sinus: microsurgical anatomy. Neurosurgery 55(1), 179 (2004). https://doi.org/10.1227/01.NEU.0000126953.59406.77
M.B. Gonçalves, J.G. de Oliveira, H.A. Williams, R.M.P. Alvarenga, J.A. Landeiro, Cavernous sinus medial wall: dural or fibrous layer? Systematic review of the literature. Neurosurg. Rev. 35(2), 147–154 (2012). https://doi.org/10.1007/s10143-011-0360-3
J.P. Cottier, C. Destrieux, L. Brunereau, et al., Cavernous sinus invasion by pituitary adenoma: MR imaging. Radiology (2000). https://doi.org/10.1148/radiology.215.2.r00ap18463
Y. Diao, L. Liang, C. Yu, M. Zhang, Is there an identifiable intact medial wall of the cavernous sinus? Macro- and microscopic anatomical study using sheet plastination. Neurosurgery 73, ons106–ons109 (2013). https://doi.org/10.1227/NEU.0b013e3182889f2b.
K. Shi, Z. Li, X. Wu et al., The medial wall and medial compartment of the cavernous sinus: an anatomic study using plastinated histological sections. Neurosurg. Rev. 45(5), 3381–3391 (2022). https://doi.org/10.1007/s10143-022-01846-9
S. Yilmazlar, H. Kocaeli, F. Aydiner, E. Korfali, Medial portion of the cavernous sinus: quantitative analysis of the medial wall. Clin. Anat. 18(6), 416–422 (2005). https://doi.org/10.1002/ca.20160
V.V. Dolenc (ed.), Anatomy of the cavernous sinus. in Anatomy and Surgery of the Cavernous Sinus. (Springer; 1989), pp. 3–137. https://doi.org/10.1007/978-3-7091-6942-1_2
S.H. Kim, K.C. Lee, S.H. Kim, Cranial nerve palsies accompanying pituitary tumour. J. Clin. Neurosci. 14(12), 1158–1162 (2007). https://doi.org/10.1016/j.jocn.2006.07.016
N. Cinar, Y. Tekinel, S. Dagdelen, H. Oruckaptan, F. Soylemezoglu, T. Erbas, Cavernous sinus invasion might be a risk factor for apoplexy. Pituitary 16(4), 483–489 (2013). https://doi.org/10.1007/s11102-012-0444-2
A. Hosmann, A. Micko, J.M. Frischer et al., Multiple pituitary apoplexy-cavernous sinus invasion as major risk factor for recurrent hemorrhage. World Neurosurg. 126, e723–e730 (2019). https://doi.org/10.1016/j.wneu.2019.02.138
A. Dincer, V. Sharma, N. Madan, C. Heilman, Cavernous segment internal carotid artery stenosis specific to meningiomas compared to pituitary adenomas. J. Neuroimaging 33(1), 73–78 (2023). https://doi.org/10.1111/jon.13051
S. Melmed, Pituitary-tumor endocrinopathies. N. Engl. J. Med. 382(10), 937–950 (2020). https://doi.org/10.1056/NEJMra1810772
M. Buchfelder, S.M. Schlaffer, The surgical treatment of acromegaly. Pituitary 20(1), 76–83 (2017). https://doi.org/10.1007/s11102-016-0765-7
J. Wass, Debulking of pituitary adenomas improves hormonal control of acromegaly by somatostatin analogues. Eur. J. Endocrinol. 152(5), 693–694 (2005). https://doi.org/10.1530/eje.1.01896
A. Colao, R. Attanasio, R. Pivonello et al., Partial surgical removal of growth hormone-secreting pituitary tumors enhances the response to somatostatin analogs in acromegaly. J. Clin. Endocrinol. Metab. 91(1), 85–92 (2006). https://doi.org/10.1210/jc.2005-1208
R.S. Jallad, N.R. Musolino, S. Kodaira, V.A. Cescato, M.D. Bronstein, Does partial surgical tumour removal influence the response to octreotide-LAR in acromegalic patients previously resistant to the somatostatin analogue? Clin. Endocrinol. 67(2), 310–315 (2007). https://doi.org/10.1111/j.1365-2265.2007.02885.x
N. Karavitaki, H.E. Turner, C.B.T. Adams et al., Surgical debulking of pituitary macroadenomas causing acromegaly improves control by lanreotide. Clin. Endocrinol. 68(6), 970–975 (2008). https://doi.org/10.1111/j.1365-2265.2007.03139.x
P. Petrossians, L. Borges-Martins, C. Espinoza et al., Gross total resection or debulking of pituitary adenomas improves hormonal control of acromegaly by somatostatin analogs. Eur. J. Endocrinol. 152(1), 61–66 (2005). https://doi.org/10.1530/eje.1.01824
A. Giustina, N. Biermasz, F.F. Casanueva et al., Consensus on criteria for acromegaly diagnosis and remission. Pituitary 27(1), 7–22 (2024). https://doi.org/10.1007/s11102-023-01360-1
M. Fleseriu, R. Auchus, I. Bancos et al., Consensus on diagnosis and management of Cushing’s disease: a guideline update. Lancet Diabetes Endocrinol. 9(12), 847–875 (2021). https://doi.org/10.1016/S2213-8587(21)00235-7
Y. Greenman, G. Ouaknine, I. Veshchev, I.I. Reider-Groswasser, Y. Segev, N. Stern, Postoperative surveillance of clinically nonfunctioning pituitary macroadenomas: markers of tumour quiescence and regrowth. Clin. Endocrinol. 58(6), 763–769 (2003). https://doi.org/10.1046/j.1365-2265.2003.01784.x
E.P. O’Sullivan, C. Woods, N. Glynn et al., The natural history of surgically treated but radiotherapy-naïve nonfunctioning pituitary adenomas. Clin. Endocrinol. 71(5), 709–714 (2009). https://doi.org/10.1111/j.1365-2265.2009.03583.x
C.P. Hofstetter, B.J. Shin, L. Mubita et al., Endoscopic endonasal transsphenoidal surgery for functional pituitary adenomas. Neurosurg. Focus 30(4), E10 (2011). https://doi.org/10.3171/2011.1.FOCUS10317
A. Ajlan, A.S. Achrol, A. Albakr et al., Cavernous sinus involvement by pituitary adenomas: clinical implications and outcomes of endoscopic endonasal resection. J. Neurol. Surg. B Skull Base 78(3), 273–282 (2017). https://doi.org/10.1055/s-0036-1598022
H. Borghei-Razavi, B.A. Muhsen, K. Joshi, T. Woodard, V.R. Kshettry, Endoscopic extracapsular resection of an adrenocorticotropic hormone–secreting macroadenoma with selective resection of the medial cavernous sinus wall. World Neurosurg. 144, 199 (2020). https://doi.org/10.1016/j.wneu.2020.09.087
L.J.M. de Macêdo Filho, A.V.G. Diógenes, E.G. Barreto et al., Endoscopic endonasal resection of the medial wall of the cavernous sinus and its impact on outcomes of pituitary surgery: a systematic review and meta-analysis. Brain Sci. 12(10), 1354 (2022). https://doi.org/10.3390/brainsci12101354
A. Ishida, H. Shiramizu, H. Yoshimoto et al., Resection of the cavernous sinus medial wall improves remission rate in functioning pituitary tumors: retrospective analysis of 248 consecutive cases. Neurosurgery 91(5), 775–781 (2022). https://doi.org/10.1227/neu.0000000000002109
Y. Nagata, K. Takeuchi, T. Yamamoto et al., Removal of the medial wall of the cavernous sinus for functional pituitary adenomas: a technical report and pathologic significance. World Neurosurg. 126, 53–58 (2019). https://doi.org/10.1016/j.wneu.2019.02.134
E.H. Oldfield, Cushing’s disease: lessons learned from 1500 cases. Neurosurgery 64, 27–36 (2017). https://doi.org/10.1093/neuros/nyx378
A.T. Omar, D.G. Munoz, J. Goguen et al., Resection of the medial wall of the cavernous sinus in functioning pituitary adenomas: technical note and outcomes in a matched-cohort study. Clin. Neurol. Neurosurg. 200, 106306 (2021). https://doi.org/10.1016/j.clineuro.2020.106306
H.H. Park, E.H. Kim, C.R. Ku, E.J. Lee, S.H. Kim, Outcomes of aggressive surgical resection in growth hormone–secreting pituitary adenomas with cavernous sinus invasion. World Neurosurg. 117, e280–e289 (2018). https://doi.org/10.1016/j.wneu.2018.06.012
S. Berkmann, S. Schlaffer, C. Nimsky, R. Fahlbusch, M. Buchfelder, Intraoperative high-field MRI for transsphenoidal reoperations of nonfunctioning pituitary adenoma. J. Neurosurg. 121(5), 1166–1175 (2014). https://doi.org/10.3171/2014.6.JNS131994
P.T. Sylvester, J.A. Evans, G.J. Zipfel et al., Combined high-field intraoperative magnetic resonance imaging and endoscopy increase extent of resection and progression-free survival for pituitary adenomas. Pituitary 18(1), 72–85 (2015). https://doi.org/10.1007/s11102-014-0560-2
R. Fahlbusch, B.V. Keller, O. Ganslandt, J. Kreutzer, C. Nimsky, Transsphenoidal surgery in acromegaly investigated by intraoperative high-field magnetic resonance imaging. Eur. J. Endocrinol. 153(2), 239–248 (2005). https://doi.org/10.1530/eje.1.01970
P.S. Jones, B. Swearingen, Intraoperative MRI for pituitary adenomas. Neurosurg. Clin. N. Am. 30(4), 413–420 (2019). https://doi.org/10.1016/j.nec.2019.05.003
Y. Greenman, K. Tordjman, E. Osher et al., Postoperative treatment of clinically nonfunctioning pituitary adenomas with dopamine agonists decreases tumour remnant growth. Clin. Endocrinol. 63(1), 39–44 (2005). https://doi.org/10.1111/j.1365-2265.2005.02295.x
Y. Greenman, M.D. Bronstein, Cabergoline should be attempted in progressing non-functioning pituitary macroadenoma. Eur. J. Endocrinol. 185(4), D11–D20 (2021). https://doi.org/10.1530/EJE-21-0344
R.L. Batista, N.R.C. Musolino, V.A.S. Cescato et al., Cabergoline in the management of residual nonfunctioning pituitary adenoma: a single-center, open-label, 2-year randomized clinical trial. Am. J. Clin. Oncol. 42(2), 221–227 (2019). https://doi.org/10.1097/COC.0000000000000505
A. Colao, C. Di Somma, R. Pivonello, A. Faggiano, G. Lombardi, S. Savastano, Medical therapy for clinically non-functioning pituitary adenomas. Endocr. Relat. Cancer 15(4), 905–915 (2008). https://doi.org/10.1677/ERC-08-0181
P. Breen, J.C. Flickinger, D. Kondziolka, A.J. Martinez, Radiotherapy for nonfunctional pituitary adenoma: analysis of long-term tumor control. J. Neurosurg. 89(6), 933–938 (1998). https://doi.org/10.3171/jns.1998.89.6.0933
M.N. Hughes, K.J. Llamas, M.E. Yelland, L.B. Tripcony, Pituitary adenomas: long-term results for radiotherapy alone and post-operative radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 27(5), 1035–1043 (1993). https://doi.org/10.1016/0360-3016(93)90520-6
F. Castinetti, J. Régis, H. Dufour, T. Brue, Role of stereotactic radiosurgery in the management of pituitary adenomas. Nat. Rev. Endocrinol. 6(4), 214–223 (2010). https://doi.org/10.1038/nrendo.2010.4
P. Colin, N. Jovenin, B. Delemer et al., Treatment of pituitary adenomas by fractionated stereotactic radiotherapy: a prospective study of 110 patients. Int. J. Radiat. Oncol. Biol. Phys. 62(2), 333–341 (2005). https://doi.org/10.1016/j.ijrobp.2004.09.058
J. Estrada, M. Boronat, M. Mielgo et al., The long-term outcome of pituitary irradiation after unsuccessful transsphenoidal surgery in Cushing’s disease. N. Engl. J. Med. 336(3), 172–177 (1997). https://doi.org/10.1056/NEJM199701163360303
Acknowledgements
With financial support from the French National Research Agency (ANR) and ITMO Cancer of Aviesan within the framework of the 2021–2030 Cancer Control Strategy, on funds administred by Inserm.
Author information
Authors and Affiliations
Contributions
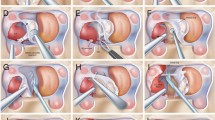
E.L., F.C., and P.K. wrote the main manuscript. M.B. prépare Fig. 1 and E.L. prepared Fig. 2. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lefevre, E., Chasseloup, F., Hage, M. et al. Clinical and therapeutic implications of cavernous sinus invasion in pituitary adenomas. Endocrine (2024). https://doi.org/10.1007/s12020-024-03877-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12020-024-03877-2