Abstract
Objective
Aldosterone-producing adenoma (APA) and bilateral idiopathic hyperaldosteronism (IHA) are the most common subtypes of primary aldosteronism (PA), and the PA subtype dictates the treatment options. This study aimed to identify predictors of declined estimated glomerular filtration rate (eGFR) following each treatment in patients with APA and IHA.
Methods
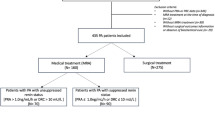
We retrospectively investigated 45 patients with APA who had undergone adrenalectomy (ADX) and 37 patients with IHA who had received treatment with a mineralocorticoid receptor antagonist (MRA) to identify pre-treatment risk factors for eGFR decline during the post-treatment follow-up period.
Results
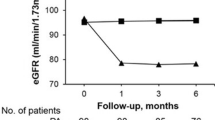
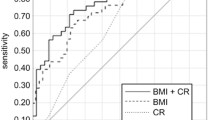
Patients with APA who underwent ADX exhibited higher eGFR declines than patients with IHA treated with MRA at the 6-month post-treatment evaluation point. A high preoperative plasma aldosterone concentration (PAC) in patients with APA and a high body mass index (BMI) in patients with IHA were identified as independent predictors of higher eGFR decline at 6 months post-treatment (β=0.42 and β=0.36, respectively). In patients with APA, the cutoff PAC to best predict a 20% decrease in eGFR following ADX, as determined by receiver operating characteristic analysis, was 524 pg/mL. In patients with IHA, the cutoff BMI to best predict a 10% decrease in eGFR following MRA administration was 25.3 kg/m2. In addition, lower preoperative flow-mediated vasodilation was associated with eGFR decline after ADX in patients with APA.
Conclusions
Greater attention should be given to the above-mentioned risk factors to prevent renal impairment following each treatment in patients with both APA and IHA.


Similar content being viewed by others
References
J.W. Funder, R.M. Carey, F. Mantero et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 101, 1889–1916 (2016)
D. Watanabe, S. Morimoto, N. Morishima, A. Ichihara, Clinical impacts of endothelium-dependent flow-mediated vasodilation assessment on primary aldosteronism. Endocr. Connect. 10, 578–587 (2021)
M. Choi, U.I. Scholl, P. Yue et al. K+ channel mutations in adrenal aldosterone-producing adenomas and hereditary hypertension. Science 331, 768–772 (2011)
S. Monticone, J. Burrello, D. Tizzani et al. Prevalence and clinical manifestations of primary aldosteronism encountered in primary care practice. J. Am. Coll. Cardiol. 11, 1811–1820 (2017)
M. Yoon, N. Hong, J. Ha et al. Prevalence and clinical characteristics of primary aldosteronism in a tertiary-care center in Korea. Hypertens. Res. 45, 1418–1429 (2022)
Y. Takeda, K. Furukawa, S. Inaba, I. Miyamori, H. Mabuchi, Genetic analysis of aldosterone synthase in patients with idiopathic hyperaldosteronism. J. Clin. Endocrinol. Metab. 84, 1633–1637 (1999)
Y. Iwakura, R. Morimoto, M. Kudo et al. Predictors of decreasing glomerular filtration rate and prevalence of chronic kidney disease after treatment of primary aldosteronism: renal outcome of 213 cases. J. Clin. Endocrinol. Metab. 99, 1593–1598 (2014)
G.L. Hundemer, G.C. Curhan, N. Yozamp, M. Wang, A. Vaidya, Renal outcomes in medically and surgically treated primary aldosteronism. Hypertension 72, 658–666 (2018)
M. Yoshioka, Y. Nakajima, T. Miyamoto et al. Age-dependent progression of renal dysfunction after adrenalectomy for aldosterone-producing adenomas in Japan. J. Endocr. Soc. 17, 577–589 (2018)
H. Kobayashi, M. Abe, Y. Nakamura et al. Association between acute fall in estimated glomerular filtration rate after treatment for primary aldosteronism and long-term decline in renal function. Hypertension 74, 630–638 (2019)
Y. Kobayashi, T. Haze, Y. Yano et al. Associations between changes in plasma renin activity and aldosterone concentrations and changes in kidney function after treatment for primary aldosteronism. Kidney Int. Rep. 20, 1291–1297 (2020)
C.K. Chan, W.S. Yang, Y.H. Lin et al. Arterial stiffness is associated with clinical outcome and cardiorenal injury in lateralized primary aldosteronism. J. Clin. Endocrinol. Metab. 105, e3950–e3960 (2020)
T. Nishikawa, M. Omura, F. Satoh et al. Guidelines for the diagnosis and treatment of primary aldosteronism-the Japan Endocrine Society 2009. Endocr. J. 58, 711–721 (2011)
T.A. Williams, J.W.M. Lenders, P. Mulatero et al. Outcomes after adrenalectomy for unilateral primary aldosteronism: an international consensus on outcome measures and analysis of remission rates in an international cohort. Lancet Diabetes Endocrinol. 5, 689–699 (2017)
R. Nakamaru, K. Yamamoto, H. Akasaka et al. Sex differences in renal outcomes after medical treatment for bilateral primary aldosteronism. Hypertension 77, 537–545 (2021)
R. Nakamaru, K. Yamamoto, H. Akasaka et al. Age-stratified comparison of clinical outcomes between medical and surgical treatments in patients with unilateral primary aldosteronism. Sci. Rep. 25, 6925 (2021)
K. Matsushita, J. Coresh, Y. Sang et al. Estimated glomerular filtration rate and albuminuria for prediction of cardiovascular outcomes: a collaborative meta-analysis of individual participant data. Lancet Diabetes Endocrinol. 3, 514–525 (2015)
X. Lin, M.H.E. Ullah, X. Wu et al. Cerebro-cardiovascular risk, target organ damage, and treatment outcomes in primary aldosteronism. Front. Cardiovasc. Med. 8, 798364 (2022)
Y. Ohno, M. Sone, N. Inagaki et al. Obesity as a key factor underlying idiopathic hyperaldosteronism. J. Clin. Endocrinol. Metab. 103, 4456–4464 (2018)
H. Kataoka, K. Nitta, J. Hoshino, Visceral fat and attribute-based medicine in chronic kidney disease. Front. Endocrinol. (Lausanne) 14, 1097596 (2023)
S. Kishimoto, K. Oki, T. Maruhashi et al. A comparison of adrenalectomy and eplerenone on vascular function in patients with aldosterone-producing adenoma. J. Clin. Endocrinol. Metab. 105, 3474–3485 (2020)
S. Kishimoto, K. Oki, T. Maruhashi et al. KCNJ5 mutation is a predictor for recovery of endothelial function after adrenalectomy in patients with aldosterone-producing adenoma. Hypertens. Res. 46, 2213–2227 (2023)
M.P. Theodorakopoulou, M. Schoina, P. Sarafidis, Assessment of endothelial and microvascular function in CKD: older and newer techniques, associated risk factors, and relations with outcomes. Am. J. Nephrol. 51, 931–949 (2020)
Y. Li, R. Cui, K. Liu et al. Relationship between endothelial dysfunction and prevalence of chronic kidney disease: the circulatory risk in communities study (CIRCS). J. Atheroscler. Thromb. 28, 622–629 (2021)
C.H. Chang, Y.H. Hu, Y.C. Tsai et al. Arterial stiffness and blood pressure improvement in aldosterone-producing adenoma harboring KCNJ5 mutations after adrenalectomy. Oncotarget 8, 29984–29995 (2017)
H. Kobayashi, Y. Nakamura, M. Abe et al. Impact of a change to a novel chemiluminescent immunoassay for measuring plasma aldosterone on the diagnosis of primary aldosteronism. Endocr. J. 70, 489–500 (2023)
Acknowledgements
We are grateful to the staff of the Department of Internal Medicine at Tokyo Women’s Medical University for their assistance.
Funding
This study was supported, in part, by a Japan Society for the Promotion of Science Grant-in-Aid for Scientific Research (JSPS KAKENHI; Grant Number 22K08167, to S.M.).
Author contributions
D.W., S.M., N.M. and A.I. contributed to the design and implementation of the research, to the analysis of the results and to the writing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interets.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Watanabe, D., Morimoto, S., Morishima, N. et al. Comparisons of risk factors for post-treatment renal dysfunction between the two major subtypes of primary aldosteronism. Endocrine 84, 245–252 (2024). https://doi.org/10.1007/s12020-023-03627-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-023-03627-w