Abstract
Purpose
Pediatric pituitary adenomas (PPA) are rare. Although PPAs are mostly benign, they can be challenging to manage. Most studies evaluating PPA are based on surgical series. We aimed to present the clinical features, hormonal status and treatment outcomes of children with PPA managed in a joint neuroendocrine setting.
Methods
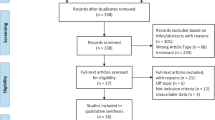
In this single-center study, demographic, clinical and endocrinological data of patients under 19 years old who were followed up with the diagnosis of PPA between 2002-2022 were retrospectively reviewed. A total of 21 studies published in the past 20 years were also systematically reviewed.
Results
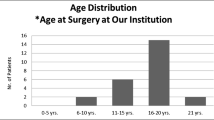
There were 79 patients (52 girls, 27 boys) with a median age of 15.8 years. Median follow-up time was 30 months. The most common adenoma subtype was non-functioning adenoma (NFA) (35.5%), followed by prolactinoma (29.1%), corticotropinoma (21.5%), and somatotropinoma (13.9%), respectively. The frequency of micro and macroadenomas was almost equal while 38% of all adenomas were invasive. Headache, visual impairment and menstrual irregularity were the most common complaints, while the most common hormonal deficiency at diagnosis was central hypothyroidism (31.6%), followed by hypogonadotropic hypogonadism (22.7%), growth hormone deficiency (15.2%) and central adrenal insufficiency (11.4%), respectively. Fifty patients (63.2%) underwent endoscopic endonasal transsphenoidal surgery (EETS). Following the surgery, impaired endocrine functions recovered at a rate of 62% while permanent central diabetes insipidus was observed in 6%, and new onset hypopituitarism developed in 4%.
Conclusion
NFA was more common in this cohort than in previous reports, which is one of the largest PPA series in the literature. Hormonal disorders, which were common at the time of diagnosis, were largely resolved with appropriate endocrinological and surgical approaches, while the rate of pituitary hormonal deficiencies after EETS was relatively low. Therefore, we recommend that children with PPA be managed in the setting of a high-volume pituitary center to provide long-term low morbidity.
Similar content being viewed by others
References
M.F. Keil, C.A. Stratakis, Pituitary tumors in childhood: an update in their diagnosis, treatment and molecular genetics. Expert. Rev. Neurother. 8, 563–574 (2008)
A.F. Daly, A. Beckers, The Epidemiology of Pituitary Adenomas. Endocrinol. Metab. Clin. North Am. 49, 347–355 (2020)
A. Perry, C.S. Graffeo, C. Marcellino, B.E. Pollock, N.M. Wetjen, F.B. Meyer, Pediatric Pituitary Adenoma: Case Series, Review of the Literature, and a Skull Base Treatment Paradigm. J. Neurol. Surg. B. Skull. Base. 79, 91–114 (2018)
F. Guaraldi, H.L. Storr, L. Ghizzoni, E. Ghigo, M.O. Savage, Paediatric pituitary adenomas: a decade of change. Horm. Res. Paediatr. 81, 145–155 (2014)
E. Knosp, E. Steiner, K. Kitz, C. Matula, Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery 33, 610–617 (1993)
R. Ferrigno, V. Hasenmajer, S. Caiulo, M. Minnetti, P. Mazzotta, H.L. Storr, A.M. Isidori, A.B. Grossman, M.C. De Martino, M.O. Savage, Paediatric Cushing’s disease: Epidemiology, pathogenesis, clinical management and outcome. Rev. Endocr. Metab. Disord. 22, 817–835 (2021)
L. Katznelson, E.R. Laws Jr, S. Melmed, M.E. Molitch, M.H. Murad, A. Utz, J.A. Wass, Endocrine Society. Acromegaly: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 99, 3933–3951 (2014)
M. Mehrazin, Pituitary tumors in children: clinical analysis of 21 cases. Child Nerv. Syst. 23, 391–398 (2007)
C. Webb, R.A. Prayson, Pediatric pituitary adenomas. Arch. Pathol. Lab. Med. 132, 77–80 (2008)
D. Locatelli, L. Massimi, M. Rigante, V. Custodi, G. Paludetti, P. Castelnuovo, C. Di Rocco, Endoscopic endonasal transsphenoidal surgery for sellar tumors in children. Int. J. Pediatr. Otorhinolaryngol. 74, 1298–1302 (2010)
P.E. Tarapore, M.E. Sughrue, L. Blevins, K.I. Auguste, N. Gupta, S. Kunwar, Microscopic endonasal transsphenoidal pituitary adenomectomy in the pediatric population. J. Neurosurg. Pediatr. 7, 501–509 (2011)
R. Zhan, G. Xu, T.M. Wiebe, X. Li, Surgical outcomes of the endoscopic transsphenoidal route to pituitary tumours in paediatric patients >10 years of age: 5 years of experience at a single institute. Arch. Dis. Child. 100, 774–778 (2015)
N. Zhang, P. Zhou, Y. Meng, F. Ye, S. Jiang, A retrospective review of 34 cases of pediatric pituitary adenoma. Childs. Nerv. Syst. 33, 1961–1967 (2017)
W. Jiao, Y. Huang, W. Sun, T. Lei, Microscopic Transnasal Transsphenoidal Surgery for Pediatric Pituitary Adenomas. J. Craniofac. Surg. 28, 1010–1012 (2017)
K.L. Krajewski, R. Rotermund, J. Flitsch, Pituitary adenomas in children and young adults. Childs. Nerv. Syst. 34, 1691–1696 (2018)
J. Chen, R.E. Schmidt, S. Dahiya, Pituitary Adenoma in Pediatric and Adolescent Populations. J. Neuropathol. Exp. Neurol. 78, 626–632 (2019)
A.M. Abunimer, H. Abou-Al-Shaar, M.A. Azab, M. Karsy, J. Guan, J.R. Kestle, W.T. Couldwell, Transsphenoidal Approaches for Microsurgical Resection of Pituitary Adenomas in Pediatric Patients. World. Neurosurg. 123, 186–193 (2019)
D. Locatelli, P. Veiceschi, P. Castelnuovo, N. Tanriover, O. Evliyaoglu, H. Canaz, D. Ugurlar, N. Gazioglu, Transsphenoidal surgery for pituitary adenomas in pediatric patients: a multicentric retrospective study. Childs. Nerv. Syst. 35, 2119–2126 (2019)
J.L. Quon, L.H. Kim, P.H. Hwang, Z.M. Patel, G.A. Grant, S.H. Cheshier, M.S.B. Edwards, Transnasal endoscopic approach for pediatric skull base lesions: a case series. J. Neurosurg. Pediatr. 14, 1–12 (2019)
A.K. Upadhyay, V. Kumar, A. Kumar Gupta, M. Rastogi, M. Husain, Microscopic Trans-sphenoidal surgery in paediatric pituitary adenoma: An institutional experience. IP. Indian. J. Neurosci. 6, 20–24 (2020)
A.P. Kelly, J.P. Greenfield, G.A. Dobri, T.H. Schwartz, Pediatric pituitary adenomas are more aggressive, more likely to be hormone producing and are more difficult to cure than adult pituitary adenomas: case series and systematic literature review. Childs. Nerv. Syst. 38, 729–738 (2022)
R. Wang, Z. Wang, Y. Song, L. Li, X. Han, S. Han, Comparative analysis of pituitary adenoma with and without apoplexy in pediatric and adolescent patients: a clinical series of 80 patients. Neurosurg. Rev. 45, 491–498 (2022)
S. Cannavo, M. Venturino, L. Curto, E. De Menis, C. D’Arrigo, P. Tita, D. Billeci, F. Trimarchi, Clinical presentation and outcome of pituitary adenomas in teenagers. Clin. Endocrinol. 58, 519–527 (2003)
L. Torres-García, R.M. Cerda-Flores, M. Márquez, Pediatric pituitary adenomas in Northeast Mexico. A follow-up study. Endocrine 62, 361–370 (2018)
A. Sethi, M. Didi, P. Dharmaraj, R. Ramakrishnan, S. Senniappan, U. Das, S. Avula, A. Sinha, C. Mallucci, K. Weerasinghe, C. Daousi, C. Gilkes, N. Thorp, J. Blair, Obesity is common at diagnosis of childhood pituitary adenoma and may persist following successful treatment. Clin. Endocrinol. (Oxf). 92, 323–330 (2020)
S. Giovinazzo, S. Puglisi, O.R. Cotta, A. Alibrandi, T. Aversa, L. Cannavò, F. Ferraù, S. Cannavò, Long-term cardiometabolic outcome in patients with pituitary adenoma diagnosed in chilhood and adolescence. Pituitary 24, 483–491 (2021)
S.S. Jayant, R. Pal, A. Rai, K. Gupta, B.D. Radotra, R. Walia, S. Dhandapani, M. Tripathi, C.K. Ahuja, P. Gupta, A. Bhansali, L. Das, P. Dutta, Paediatric Pituitary Adenomas: Clinical Presentation, Biochemical Profile and Long-Term Prognosis. Neurol. India. 70, 304–311 (2022)
T. Breil, C. Lorz, D. Choukair, J. Mittnacht, I. Inta, D. Klose, J. Jesser, E. Schulze, M. Bettendorf, Clinical Features and Response to Treatment of Prolactinomas in Children and Adolescents: A Retrospective Single-Centre Analysis and Review of the Literature. Horm. Res. Paediatr. 89, 157–165 (2018)
E. Eren, A. Törel Ergür, Ş.P. İşgüven, E. Çelebi Bitkin, M. Berberoğlu, Z. Şıklar, F. Baş, S. Yel, S. Baş, E. Söbü et al. Clinical and Laboratory Characteristics of Hyperprolactinemia in Children and Adolescents: National Survey. J. Clin. Res. Pediatr. Endocrinol. 11, 149–156 (2019)
M.E. Molitsch, R.L. Elton, R.E. Blackwell, B. Caldwell, R.J. Chang, R. Jaffe, G. Joplin, R.J. Robbins, J. Tyson, M.O. Thorner, Bromocriptine as primary therapy for prolactin-secreting macroadenomas: results of a prospective multicenter study. J. Clin. Endocrinol. Metab. 60, 698–705 (1985)
M.O. Savage, L.F. Chan, F. Afshar, P.N. Plowman, A.B. Grossman, H.L. Storr, Advances in the management of paediatric Cushing’s disease. Horm. Res. 69, 327–333 (2008)
R.M. Paragliola, A. Corsello, G. Papi, A. Pontecorvi, S.M. Corsello, Cushing’s Syndrome Effects on the Thyroid. Int. J. Mol. Sci. 22, 3131 (2021)
A. Wędrychowicz, B. Hull, K. Tyrawa, A. Kalicka-Kasperczyk, G. Zieliński, J. Starzyk, Cushing disease in children and adolescents - assessment of the clinical course, diagnostic process, and effects of the treatment - experience from a single paediatric centre. Pediatr. Endocrinol. Diabetes. Metab. 25, 127–143 (2019)
H.L. Storr, K.I. Alexandraki, L. Martin, A.M. Isidori, G.A. Kaltsas, J.P. Monson, G.M. Besser, M. Matson, J. Evanson, F. Afshar, I. Sabin, M.O. Savage, A.B. Grossman, Comparisons in the epidemiology, diagnostic features and cure rate by transsphenoidal surgery between paediatric and adult-onset Cushing’s disease. Eur. J. Endocrinol. 164, 667–674 (2011)
R.R. Lonser, J.J. Wind, L.K. Nieman, R.J. Weil, H.L. DeVroom, E.H. Oldfield, Outcome of surgical treatment of 200 children with Cushing’s disease. J. Clin. Endocrinol. Metab. 98, 892–901 (2013)
E.H. Dyer, T. Civit, A. Visot, O. Delalande, P. Derome, Transsphenoidal surgery for pituitary adenomas in children. Neurosurgery 34, 207–212 (1994)
P.A. Crock, D.K. Ludecke, U.J. Knappe, W. Saeger, A personal series of 100 children operated for Cushing’s disease (CD): optimizing minimally invasive diagnosis and transnasal surgery to achieve nearly 100% remission including reoperations. J. Pediatr. Endocrinol. Metab. 31, 1023–1031 (2018)
S. Nishio, T. Morioka, S. Suzuki, I. Takeshita, M. Fukui, T. Iwaki, Pituitary tumours in adolescence: clinical behaviour and neuroimaging features of seven cases. J. Clin. Neurosci. 8, 231–234 (2001)
E. Manojlovic-Gacic, B.E. Engström, O. Casar-Borota, Histopathological classification of non-functioning pituitary neuroendocrine tumors. Pituitary 21(2), 119–129 (2018)
S.L. Asa, O. Mete, A. Perry, R.Y. Osamura, Overview of the 2022 WHO Classification of Pituitary Tumors. Endocr. Pathol. 33(1), 6–26 (2022)
T. Kolitz, Y. Greenman, Refractory nonfunctioning pituitary adenomas. Pituitary 26(3), 278–280 (2023)
V.V. Thaker, A.E. Lage, G. Kumari, V.M. Silvera, L.E. Cohen, Clinical Course of Nonfunctional Pituitary Microadenoma in Children: A Single-Center Experience. J. Clin. Endocrinol. Metab. 104, 5906–5912 (2019)
K.M. Derrick, W.A. Gomes, R.C. Gensure, Incidence and Outcomes of Pituitary Microadenomas in Children with Short Stature/Growth Hormone Deficiency. Horm. Res. Paediatr. 90, 151–160 (2018)
J.A. Jane Jr, R.M. Starke, M.A. Elzoghby, D.L. Reames, S.C. Payne, M.O. Thorner, J.C. Marshall, E.R. Laws Jr, M.L. Vance, Endoscopic transsphenoidal surgery for acromegaly: remission using modern criteria, complications, and predictors of outcome. J. Clin. Endocrinol. Metab. 96, 2732–2740 (2011)
R.M. Starke, D.M. Raper, S.C. Payne, M.L. Vance, E.H. Oldfield, J.A. Jane Jr, Endoscopic vs microsurgical transsphenoidal surgery for acromegaly: outcomes in a concurrent series of patients using modern criteria for remission. J. Clin. Endocrinol. Metab. 98, 3190–3198 (2013)
P.C. Walz, A. Drapeau, A. Shaikhouni, J. Eide, A.J. Rugino, A. Mohyeldin, R. Carrau, D. Prevedello, Pediatric pituitary adenomas. Childs. Nerv. Syst. 35, 2107–2118 (2019)
A.F. Daly, M.A. Tichomirowa, A. Beckers, The epidemiology and genetics of pituitary adenomas. Best. Pract. Res. Clin. Endocrinol. Metab. 23, 543–554 (2009)
S. Jackman, F. Diamond, Pituitary adenomas in childhood and adolescence. Pediatr. Endocrinol. Rev. 10, 450–459 (2013)
Author information
Authors and Affiliations
Contributions
F.K.: data collection, formal analysis, investigation, methodology, validation, visualization, writing. J.H.J.: formal analysis, investigation, methodology, validation, and writing – review & editing. M.C.: data collection, formal analysis, investigation, validation. SC: methodology, validation, writing-review & editing, and formal analysis. F.M.C.J.: data collection, formal analysis, investigation, methodology, validation, and writing – review & editing. All the authors gave their final approval of the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
This study was conducted by the Department of Pediatric Endocrinology and the Department of Neurosurgery at a tertiary referral pituitary center. This study was performed in line with the principles of the Declaration of Helsinki. Written informed consent was obtained from the parents. The study protocol was approved by the Kocaeli University Medical School Ethics Committee (approval number: 2021/24).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kilci, F., Jones, J.H., Çaklılı, M. et al. Clinical and therapeutic outcomes of pediatric pituitary adenomas: a single pituitary center experience. Endocrine 83, 160–170 (2024). https://doi.org/10.1007/s12020-023-03523-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-023-03523-3