Abstract
Background
The extent of surgery in patients with papillary thyroid cancer (PTC) is a subject of ongoing debate. We aimed to explore the attitude of Spanish specialists (endocrinologists, surgeons, and otolaryngologists) in real life on the surgical management of low-risk PTC.
Methods
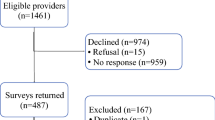
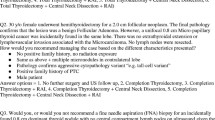
We designed an anonymous, web-based survey to inquire information regarding the preferences of interviewees for hemithyroidectomy (Hem), total thyroidectomy (TT) and prophylactic central neck dissection (pCND) in one standard patient with PTC and six clinical variants. We differentiated between small (1.1–2.5 cm) and large (2.6–4.0 cm) tumors.
Results
A total of 278 valid responses were received and divided into two groups: group END (n = 135) and group SUR (n = 143, 101 general surgeons and 42 otolaryngologists). The preference for Hem was low in the standard patient and similar between both groups (40.6 vs 49.0%, NS). This preference decreased for tumors measuring 2.6–4.0 cm, multifocal, with risk location, family history of thyroid cancer, or history of irradiation, and increased in patients older than 65 years or with comorbidity. Preference for pCND ranged from 12.6–71.1% in the group END and from 22.4–65.0% in the group SUR, with few differences between the two. In multivariate analysis, being a high-volume specialist was associated with a lower preference for Hem, while having private practice was associated with a more favorable opinion of Hem.
Conclusion
The real clinical practice of Spanish specialists is far from what is recommended by the clinical guidelines in patients with low-risk PTC, especially among high-volume professionals.

Similar content being viewed by others
Data availability
Data are available through a reasonable request to the corresponding author.
References
J.J. Díez, Continuing controversies on the extent of surgery in papillary thyroid carcinoma. Gland Surg. 12(1), 11–15 (2023). https://doi.org/10.21037/gs-22-693
B.R. Haugen, E.K. Alexander, K.C. Bible, G.M. Doherty, S.J. Mandel, Y.E. Nikiforov, F. Pacini, G.W. Randolph, A.M. Sawka, M. Schlumberger, K.G. Schuff, S.I. Sherman, J.A. Sosa, D.L. Steward, R.M. Tuttle, L. Wartofsky, 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 26(1), 1–133 (2016). https://doi.org/10.1089/thy.2015.0020
I.R. McDougall, C.A. Camargo, Treatment of micropapillary carcinoma of the thyroid: where do we draw the line?. Thyroid. 17(11), 1093–1096 (2007). https://doi.org/10.1089/thy.2007
X.M. Yu, Y. Wan, R.S. Sippel, H. Chen, Should all papillary thyroid microcarcinomas be aggressively treated? An analysis of 18,445 cases. Ann. Surg. 254(4), 653–660 (2011). https://doi.org/10.1097/SLA.0b013e318230036d
Y.W. Jeon, H.G. Gwak, S.T. Lim, J. Schneider, Y.J. Suh, Long-term prognosis of unilateral and multifocal papillary thyroid microcarcinoma after unilateral lobectomy versus total thyroidectomy. Ann. Surg. Oncol. 26(9), 2952–2958 (2019). https://doi.org/10.1245/s10434-019-07482-w
K. Matsuzu, K. Sugino, K. Masudo, M. Nagahama, W. Kitagawa, H. Shibuya, K. Ohkuwa, T. Uruno, A. Suzuki, S. Magoshi, J. Akaishi, C. Masaki, M. Kawano, N. Suganuma, Y. Rino, M. Masuda, K. Kameyama, H. Takami, K. Ito, Thyroid lobectomy for papillary thyroid cancer: long-term follow-up study of 1,088 cases. World J. Surg. 38(1), 68–79 (2014). https://doi.org/10.1007/s00268-013-2224-1
J. Lee, J.H. Park, C.R. Lee, W.Y. Chung, C.S. Park, Long-term outcomes of total thyroidectomy versus thyroid lobectomy for papillary thyroid microcarcinoma: comparative analysis after propensity score matching. Thyroid 23(11), 1408–1415 (2013). https://doi.org/10.1089/thy.2012.0463
J.J. Díez, A. Oleaga, C. Álvarez-Escolá, T. Martín, J.C. Galofré, Grupo de Trabajo de Cáncer de Tiroides de la Sociedad Española de Endocrinología y Nutrición, [Clinical guideline for management of patients with low risk differentiated thyroid carcinoma]. Endocrinol. Nutr. 62(6), e57–72 (2015). https://doi.org/10.1016/j.endonu.2015.02.006. Spanish.
J.J. Díez, V. Alcázar, P. Iglesias, A. Romero-Lluch, J. Sastre, B.P. Corral, C. Zafón, J.C. Galofré, M.J. Pamplona, Thyroid lobectomy in patients with differentiated thyroid cancer: an analysis of the clinical outcomes in a nationwide multicenter study. Gland Surg. 10(2), 678–689 (2021). https://doi.org/10.21037/gs-20-712
C. Zafon, J.J. Díez, J.C. Galofré, D.S. Cooper, Nodular thyroid disease and thyroid cancer in the era of precision medicine. Eur. Thyroid J. 6, 65–74 (2017). https://doi.org/10.1159/000457793
J.J. Díez, J.C. Galofré, A. Oleaga, E. Grande, M. Mitjavila, P. Moreno; Grupo de Trabajo de Cáncer de Tiroides de la Sociedad Española de Endocrinología y Nutrición, [Consensus statement for accreditation of multidisciplinary thyroid cancer units]. Endocrinol Nutr. 63(3), e1–15 (2016). https://doi.org/10.1016/j.endonu.2015.07.005. Spanish .
M.A. Adam, J. Pura, L. Gu, M.A. Dinan, D.S. Tyler, S.D. Reed, R. Scheri, S.A. Roman, J.A. Sosa,, Extent of surgery for papillary thyroid cancer is not associated with survival: an analysis of 61,775 patients. Ann. Surg. 260(4), 601–605 (2014). https://doi.org/10.1097/SLA.0000000000000925. discussion 605-7
R.M. Gartland, C.C. Lubitz, Impact of extent of surgery on tumor recurrence and survival for papillary thyroid cancer patients. Ann. Surg. Oncol. 25(9), 2520–2525 (2018). https://doi.org/10.1245/s10434-018-6550-2
A.D. McDow, M.C. Saucke, N.A. Marka, K.L. Long, S.C. Pitt, Thyroid lobectomy for low-risk papillary thyroid cancer: A national survey of low- and high-volume surgeons. Ann. Surg. Oncol. 28(7), 3568–3575 (2021). https://doi.org/10.1245/s10434-021-09898-9
Y.I. Cheon, S.C. Shin, M. Lee, E.S. Sung, J.C. Lee, M. Kim, B.H. Kim, I.J. Kim, B.J. Lee, Survey of Korean head and neck surgeons and endocrinologists for the surgical extent of 1.5 and 2.5 cm papillary thyroid carcinoma. Gland Surg. 11(11), 1744–1753 (2022). https://doi.org/10.21037/gs-22-326
Ö. Makay, M. Özdemir, Y.G. Şenyürek, F. Tunca, M. Düren, M. Uludağ, M. Hacıyanlı, G. Içöz, A. Işgör, S. Özbaş, Z. Özcan, S. Tezelman, Surgical approaches for papillary microcarcinomas: Turkey’s perspective. Turk J Surg. 34(2), 89–93 (2018). https://doi.org/10.5152/turkjsurg.2018.3596
A.D. McDow, B.R. Roman, M.C. Saucke, C.B. Jensen, N. Zaborek, J.L. Jennings, L. Davies, J.P. Brito, S.C. Pitt, Factors associated with physicians’ recommendations for managing low-risk papillary thyroid cancer. Am. J. Surg. 222(1), 111–118 (2021). https://doi.org/10.1016/j.amjsurg.2020.11.021
P. Perros, K. Boelaert, S. Colley, C. Evans, R.M. Evans, G. Gerrard Ba, J. Gilbert, B. Harrison, S.J. Johnson, T.E. Giles, L. Moss, V. Lewington, K. Newbold, J. Taylor, R.V. Thakker, J. Watkinson, G.R. Williams; British Thyroid Association, Guidelines for the management of thyroid cancer. Clin. Endocrinol. (Oxf) 81, 1–122 (2014). https://doi.org/10.1111/cen.12515
N. Agrawal, M.R. Evasovich, E. Kandil, S.I. Noureldine, E.A. Felger, R.P. Tufano, D.H. Kraus, L.A. Orloff, R. Grogan, P. Angelos, B.C. Stack Jr, B. McIver, G.W. Randolph, Indications and extent of central neck dissection for papillary thyroid cancer: An American Head and Neck Society Consensus Statement. Head Neck 39(7), 1269–1279 (2017). https://doi.org/10.1002/hed.24715
J.J. Díez, E. Anda, J. Sastre, B. Pérez Corral, C. Álvarez-Escolá, L. Manjón, M. Paja, M. Sambo, P. Santiago Fernández, C. Blanco Carrera, J.C. Galofré, E. Navarro, C. Zafón, E. Sanz, A. Oleaga, O. Bandrés, S. Donnay, A. Megía, M. Picallo, C. Sánchez Ragnarsson, G. Baena-Nieto, J.C.F. García, B. Lecumberri, M.S. de la Vega, A.R. Romero-Lluch, P. Iglesias, Prevalence and risk factors for hypoparathyroidism following total thyroidectomy in Spain: a multicentric and nation-wide retrospective analysis. Endocrine 66(2), 405–415 (2019). https://doi.org/10.1007/s12020-019-02014-8
W. Zhao, L. You, X. Hou, S. Chen, X. Ren, G. Chen, Y. Zhao, The effect of prophylactic central neck dissection on locoregional recurrence in papillary thyroid cancer after total thyroidectomy: A systematic review and meta-analysis : pCND for the locoregional recurrence of papillary thyroid cancer. Ann. Surg. Oncol 24(8), 2189–2198 (2017). https://doi.org/10.1245/s10434-016-5691-4
S. Zhan, D. Luo, W. Ge, B. Zhang, T. Wang, Clinicopathological predictors of occult lateral neck lymph node metastasis in papillary thyroid cancer: A meta-analysis. Head Neck 41(7), 2441–2449 (2019). https://doi.org/10.1002/hed.25762
J.W. Kim, J.L. Roh, G. Gong, K.J. Cho, S.H. Choi, S.Y. Nam, S.Y. Kim, Recurrence in patients with clinically early-stage papillary thyroid carcinoma according to tumor size and surgical extent. Am. J. Surg. 212(3), 419–425.e1 (2016). https://doi.org/10.1016/j.amjsurg.2015.12.015
C.H. Shin, J.L. Roh, D.E. Song, K.J. Cho, S.H. Choi, S.Y. Nam, S.Y. Kim, Prognostic value of tumor size and minimal extrathyroidal extension in papillary thyroid carcinoma. Am. J. Surg. 220(4), 925–931 (2020). https://doi.org/10.1016/j.amjsurg.2020.02.020
M.A. Adam, S. Thomas, L. Youngwirth, T. Hyslop, S.D. Reed, R.P. Scheri, S.A. Roman, J.A. Sosa, Is there a minimum number of thyroidectomies a surgeon should perform to optimize patient outcomes?. Ann. Surg. 265(2), 402–407 (2017). https://doi.org/10.1097/SLA.0000000000001688
A. Hauch, Z. Al-Qurayshi, G. Randolph, E. Kandil, Total thyroidectomy is associated with increased risk of complications for low- and high-volume surgeons. Ann. Surg. Oncol. 21(12), 3844–52 (2014). Epub 2014 Jun 19. PMID: 24943236 https://doi.org/10.1245/s10434-014-3846-8
F. Menegaux, J.C. Lifante, Controversy: For or against thyroid lobectomy in >1cm differentiated thyroid cancer?. Ann. Endocrinol. (Paris) 82(2), 78–82 (2021). https://doi.org/10.1016/j.ando.2021.03.004
V. Hsiao, T.J. Light, A.A. Adil, M. Tao, A.S. Chiu, M. Hitchcock, N. Arroyo, S. Fernandes-Taylor, D.O. Francis, Complication rates of total thyroidectomy vs hemithyroidectomy for treatment of papillary thyroid microcarcinoma: A systematic review and meta-analysis. JAMA Otolaryngol Head Neck Surg. 148(6), 531–539 (2022). https://doi.org/10.1001/jamaoto.2022.0621
B.H.H. Lang, C.K.H. Wong, Lobectomy is a more cost-effective option than total thyroidectomy for 1 to 4 cm papillary thyroid carcinoma that do not possessclinically recognizable high-risk features. Ann. Surg. Oncol 23, 3641–3652 (2016).
M. Padovano, M. Scopetti, R. Tomassi, F. Manetti, S. D’Errico, A. Santurro, G. De Toma, P. Frati, P. Miccoli, V. Fineschi, Mapping complications in thyroid surgery: statistical data are useful for medico-legal management of a recurrent safety issue. Updates Surg. 74(5), 1725–1732 (2022). https://doi.org/10.1007/s13304-022-01357-8
C. Zhang, Y. Li, J. Li, X. Chen, Total thyroidectomy versus lobectomy for papillary thyroid cancer: A systematic review and meta-analysis. Medicine (Baltimore) 99(6), e19073 (2020). https://doi.org/10.1097/MD.0000000000019073
J.A. Sosa, H.M. Bowman, J.M. Tielsch, N.R. Powe, T.A. Gordon, R. Udelsman, The importance of surgeon experience for clinical and economic outcomes from thyroidectomy. Ann. Surg. 228(3), 320–330 (1998). https://doi.org/10.1097/00000658-199809000-00005
Acknowledgements
We thank SEEN, endocrine surgery section of the AEC and SEORL-CCC who endorsed our survey and assisted its dissemination and all members of these societies who took the time to complete the survey.
Author contributions
Conception and design: J.J.D.; administrative support, provision of study materials, collection and assembly of data, data analysis and interpretation: all authors. Manuscript writing of the first draft: J.J.D.; final approval of manuscript: all authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Díez, J.J., Parente, P. & Durán-Poveda, M. Surgical management of low-risk papillary thyroid cancer in real life in Spain: a nationwide survey of endocrine neck surgeons and endocrinologists. Endocrine 83, 422–431 (2024). https://doi.org/10.1007/s12020-023-03488-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-023-03488-3