Abstract
Background and aim
Diabetes mellitus has been linked to a lower rate of cancer survival and an increase in the incidence of most malignancies. Investigations showed that diabetes might affect ovarian cancer (OC) prognosis and survival. Based on the current information, this study intends to review the risk factors, molecular pathways, and impact of diabetes on OC.
Methods
The data was derived from online databases, including Web of Science, PubMed, and Scopus. The inclusion criteria were original studies, which included the risk factors, molecular mechanisms, and impact of diabetes on OC. The effect of different antidiabetic drugs was also discussed in this manuscript. All of the clinical, in vivo, and in vitro studies were included in the present study.
Results
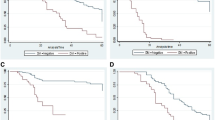
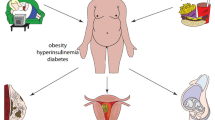
The diagnosis of diabetes mellitus negatively affects the survival and prognosis in OC cases. The epidemiologic data shows that the risk of OC increases in patients with diabetes mellitus compared to the healthy population. Insulin-like growth factors family was raised in diabetic patients, which target several mechanisms, including targeting oxidative stress, angiogenesis, and tumor markers. Antidiabetic drugs such as metformin, sitagliptin, and rosiglitazone have a promising effect on elongation of survival and enhancement of prognosis in OC patients.
Conclusions
Diabetes mellitus is a significant risk factor for OC in women, and it negatively impacts survival and prognosis. Molecular mechanisms such as IGF family, oxidative stress, and inflammatory cytokines have been identified to explain this relationship. Antidiabetic drugs like metformin, sitagliptin, and rosiglitazone have shown promise in improving survival and prognosis of OC patients.


Similar content being viewed by others
Data availability
All data generated during this study are included in this published article.
References
T. Chowdhury, Diabetes and cancer. QJM Int. J. Med. 103(12), 905–915 (2010).
I.L. Romero et al. Relationship of type II diabetes and metformin use to ovarian cancer progression, survival, and chemosensitivity. Obstet. Gynecol. 119(1), 61–67 (2012). https://doi.org/10.1097/AOG.0b013e3182393ab3. ppJan
K. Müssig, H.-U. Häring, Insulin signal transduction in normal cells and its role in carcinogenesis. Exp. Clin. Endocrinol. Diabetes 118(06), 356–359 (2010).
M. Pollak, Insulin and insulin-like growth factor signalling in neoplasia. Nat. Rev. Cancer 8(12), 915–928 (2008).
D.M. Lamkin et al. Glucose as a prognostic factor in ovarian carcinoma. Cancer 115(5), 1021–1027 (2009).
S. Becker, L. Dossus, R. Kaaks, Obesity related hyperinsulinaemia and hyperglycaemia and cancer development. Arch. Physiol. Biochem. 115(2), 86–96 (2009).
A. Bakhru, R.J. Buckanovich, J.J. Griggs, The impact of diabetes on survival in women with ovarian cancer. Gynecol. Oncol. 121(1), 106–111 (2011). https://doi.org/10.1016/j.ygyno.2010.12.329.
L. Wang, L. Zhong, B. Xu, M. Chen, H. Huang, Diabetes mellitus and the risk of ovarian cancer: a systematic review and meta-analysis of cohort and case-control studies. BMJ Open 10(12), e040137 (2020). https://doi.org/10.1136/bmjopen-2020-040137.
J.-Y. Lee, I. Jeon, J.W. Kim, Y.-S. Song, J.-M. Yoon, S.M. Park, Diabetes mellitus and ovarian cancer risk: a systematic review and meta-analysis of observational studies. Int. J. Gynecol. Cancer 23(3), 402–412 (2013). https://doi.org/10.1097/IGC.0b013e31828189b2.
H. Mulholland, L. Murray, C. Cardwell, M. Cantwell, Dietary glycaemic index, glycaemic load and endometrial and ovarian cancer risk: a systematic review and meta-analysis. Br. J. Cancer 99(3), 434–441 (2008).
D. Zhang, N. Li, Y. Xi, Y. Zhao, T. Wang, Diabetes mellitus and risk of ovarian cancer. A systematic review and meta-analysis of 15 cohort studies. Diabetes Res Clin Pract. 130, 43–52 (2017). https://doi.org/10.1016/j.diabres.2017.04.005.
L. Wang, L. Zhong, B. Xu, M. Chen, H. Huang, Diabetes mellitus and the risk of ovarian cancer: a systematic review and meta-analysis of cohort and case–control studies. BMJ Open 10(12), e040137 (2020). 10.1136/bmjopen-2020-040137.
D. LeRoith, J.M.P. Holly, B.E. Forbes, Insulin-like growth factors: ligands, binding proteins, and receptors. Mol. Metab. 52, 101245 (2021). https://doi.org/10.1016/j.molmet.2021.101245
Y.W. Lin, X.F. Weng, B.L. Huang, H.P. Guo, Y.W. Xu, Y.H. Peng, IGFBP-1 in cancer: expression, molecular mechanisms, and potential clinical implications. Am. J. Transl. Res. 13(3), 813–832 (2021).
N. Khanlarkhani et al. Metabolic risk factors of ovarian cancer: a review. JBRA Assist Reprod. 26(2), 335–347 (2022). https://doi.org/10.5935/1518-0557.20210067.
D. Yee, F.R. Morales, T.C. Hamilton, D.D. Von Hoff, Expression of insulin-like growth factor I, its binding proteins, and its receptor in ovarian cancer. Cancer Res. 51(19), 5107–5112 (1991).
W.H. Gotlieb et al. Insulin-like growth factor receptor I targeting in epithelial ovarian cancer. Gynecol. Oncol. 100(2), 389–396 (2006).
E.P. Beck et al. Identification of insulin and insulin-like growth factor I (IGF I) receptors in ovarian cancer tissue. Gynecol. Oncol. 53(2), 196–201 (1994).
B. Weigang, M. Nap, A. Bittl, W. Jaeger, Immunohistochemical localization of insulin-like growth factor 1 receptors in benign and malignant tissues of the female genital tract. Tumor Biol. 15(4), 236–246 (1994).
A. Karasik, J. Menczer, C. Pariente, H. Kanety, Insulin-like growth factor-I (IGF-I) and IGF-binding protein-2 are increased in cyst fluids of epithelial ovarian cancer. J. Clin. Endocrinol. Metab. 78(2), 271–276 (1994).
A. Ouban, P. Muraca, T. Yeatman, D. Coppola, Expression and distribution of insulin-like growth factor-1 receptor in human carcinomas. Human Pathol. 34(8), 803–808 (2003).
J. Brokaw et al. IGF-I in epithelial ovarian cancer and its role in disease progression. Growth Factors 25(5), 346–354 (2007).
D. Spentzos et al. IGF axis gene expression patterns are prognostic of survival in epithelial ovarian cancer. Endocr. Relat. Cancer 14(3), 781–790 (2007).
R.A. Sayer et al. High insulin-like growth factor-2 (IGF-2) gene expression is an independent predictor of poor survival for patients with advanced stage serous epithelial ovarian cancer. Gynecol. Oncol. 96(2), 355–361 (2005).
L. Lu et al. The relationship of insulin-like growth factor-II, insulin-like growth factor binding protein-3, and estrogen receptor-alpha expression to disease progression in epithelial ovarian cancer. Clin. Cancer Res. 12(4), 1208–1214 (2006).
J. Lancaster et al. High expression of insulin-like growth factor binding protein-2 messenger RNA in epithelial ovarian cancers produces elevated preoperative serum levels. Int. J. Gynecol. Cancer 16(4), 1529–1535 (2006).
A. Flyvbjerg, O. Mogensen, B. Mogensen, O.S. Nielsen, Elevated serum insulin-like growth factor-binding protein 2 (IGFBP-2) and decreased IGFBP-3 in epithelial ovarian cancer: correlation with cancer antigen 125 and tumor-associated trypsin inhibitor. J. Clin. Endocrinol. Metab. 82(7), 2308–2313 (1997).
D. Katsaros et al. IGFBP-3 in epithelial ovarian carcinoma and its association with clinico-pathological features and patient survival. Eur. J. Cancer 37(4), 478–485 (2001).
P. Torng et al. Insulin-like growth factor binding protein-3 (IGFBP-3) acts as an invasion-metastasis suppressor in ovarian endometrioid carcinoma. Oncogene 27(15), 2137–2147 (2008).
B. Waksmański, J. Dudkiewicz, T. Kowalski, Changes in insulin-like growth factor I, 17-b-estradiol, and progesterone in postmenopausal women with benign and malignant ovarian tumours. Med. Sci. Monit. 7(5), 919–923 (2001).
K. Wilson et al. Regulation and function of the extracellular matrix protein tenascin-C in ovarian cancer cell lines. Br. J. Cancer 80(5), 685–692 (1999).
M.-R. Shen et al. Insulin-like growth factor 1 stimulates KCl cotransport, which is necessary for invasion and proliferation of cervical cancer and ovarian cancer cells. J. Biol. Chem. 279(38), 40017–40025 (2004).
Y. Tanaka, H. Kobayashi, M. Suzuki, Y. Hirashima, N. Kanayama, T. Terao, Genetic downregulation of pregnancy‐associated plasma protein‐A (PAPP‐A) by bikunin reduces IGF‐I‐dependent Akt and ERK1/2 activation and subsequently reduces ovarian cancer cell growth, invasion and metastasis. Int. J. Cancer 109(3), 336–347 (2004).
Z. Cao, L.-Z. Liu, D.A. Dixon, J.Z. Zheng, B. Chandran, B.-H. Jiang, Insulin-like growth factor-I induces cyclooxygenase-2 expression via PI3K, MAPK and PKC signaling pathways in human ovarian cancer cells. Cell. Signal. 19(7), 1542–1553 (2007).
B.R. Whitley, L.M. Beaulieu, J.C. Carter, F.C. Church, Phosphatidylinositol 3-kinase/Akt regulates the balance between plasminogen activator inhibitor-1 and urokinase to promote migration of SKOV-3 ovarian cancer cells. Gynecol. Oncol. 104(2), 470–479 (2007).
W. Kuhn et al. Prognostic significance of urokinase (uPA) and its inhibitor PAI-1 for survival in advanced ovarian carcinoma stage FIGO IIIc. Br. J. Cancer 79(11), 1746–1751 (1999).
M.E. van der Burg, S.C. Henzen‐Logmans, E.M. Berns, W.L. van Putten, J.G. Klijn, J.A. Foekens, Expression of urokinase‐type plasminogen activator (uPA) and its inhibitor PAI‐1 in benign, borderline, malignant primary and metastatic ovarian tumors. Int. J. Cancer 69(6), 475–479 (1996).
H. Kanety et al. Increased insulin-like growth factor binding protein-2 (IGFBP-2) gene expression and protein production lead to high IGFBP-2 content in malignant ovarian cyst fluid. Br. J. Cancer 73(9), 1069–1073 (1996).
E.-J. Lee et al. Insulin-like growth factor binding protein 2 promotes ovarian cancer cell invasion. Mol. Cancer 4(1), 1–8 (2005).
G.Y. Locker et al. ASCO 2006 update of recommendations for the use of tumor markers in gastrointestinal cancer. J. Clin. Oncol. 24(33), 5313–5327 (2006).
O. Uygur-Bayramicli et al. Type 2 diabetes mellitus and CA 19-9 levels. World J. Gastroenterol. 13(40), 5357–5359 (2007). https://doi.org/10.3748/wjg.v13.i40.5357.
M. Dede, S. Gungor, M. Yenen, I. Alanbay, N. Duru, A. Haşimi, CA19-9 may have clinical significance in mature cystic teratomas of the ovary. Int. J. Gynecol. Cancer 16(1), (2006).
H.Y. Cho, M.S. Kyung, Serum CA19-9 as a predictor of malignancy in primary ovarian mucinous tumors: a matched case-control study. Med. Sci. Monit. 20, 1334–1339 (2014). https://doi.org/10.12659/msm.890954.
M. Zhang, B. Zhao, J. Xie, Y. Liang, Z. Yang, Serum human epididymis protein 4 is associated with renal function and diabetic kidney disease in patients with type 2 diabetes mellitus. Biomed. Res. Int. 2019, 4831459 (2019). https://doi.org/10.1155/2019/4831459.
P.F. Li, Y.J. Lin, Y.J. Liang, W.L. Chen, The association between human epididymis secretory protein 4 and metabolic syndrome. J. Clin. Med. 11(9), (2022) https://doi.org/10.3390/jcm11092362.
R. Lugano, M. Ramachandran, A. Dimberg, Tumor angiogenesis: causes, consequences, challenges and opportunities. Cell. Mol. Life Sci. 77(9), 1745–1770 (2020).
S. Reuter, S.C. Gupta, M.M. Chaturvedi, B.B. Aggarwal, Oxidative stress, inflammation, and cancer: how are they linked. Free Radic. Biol. Med. 49(11), 1603–1616 (2010).
S.D. Hursting, N.A. Berger, Energy balance, host-related factors, and cancer progression. J. Clin. Oncol. 28(26), 4058 (2010).
L.D. Kellenberger et al. The role of dysregulated glucose metabolism in epithelial ovarian cancer. J. Oncol. 2010, 514310 (2010). https://doi.org/10.1155/2010/514310.
W. Duan et al. Hyperglycemia, a neglected factor during cancer progression. BioMed Res. Int. 2014, 461917 (2014).
E.J. Gallagher, D. LeRoith, Diabetes, antihyperglycemic medications and cancer risk: smoke or fire?. Curr. Opin. Endocrinol. Diabetes Obes. 20(5), 485–494 (2013).
R.S. Hundal et al. Mechanism by which metformin reduces glucose production in type 2 diabetes. Diabetes 49(12), 2063–2069 (2000).
D.R. Morales, A.D. Morris, Metformin in cancer treatment and prevention. Annu. Rev. Med. 66(1), 17–29 (2015).
B. Viollet, B. Guigas, N.S. Garcia, J. Leclerc, M. Foretz, F. Andreelli, Cellular and molecular mechanisms of metformin: an overview. Clin. Sci. 122(6), 253–270 (2012).
M. Pollak, The insulin and insulin-like growth factor receptor family in neoplasia: an update. Nat. Rev. Cancer 12(3), 159–169 (2012).
Y. Yi, W. Zhang, J. Yi, Z.-X. Xiao, Role of p53 family proteins in metformin anti-cancer activities. J. Cancer 10(11), 2434 (2019).
Y. Cui, J. Zhou, F. Rong, Combination of metformin and RG7388 enhances inhibition of growth and induction of apoptosis of ovarian cancer cells through the PI3K/AKT/mTOR pathway. Biochem. Biophys. Res. Commun. 533(4), 665–671 (2020).
Y. Fu, Q. Zhang, X. Wang, H. He, Antidiabetic drug metformin mitigates ovarian cancer SKOV3 cell growth by triggering G2/M cell cycle arrest and inhibition of m-TOR/PI3K/Akt signaling pathway. Eur. Rev. Med. Pharmacol. Sci. 21(5), 1169–1175 (2017).
N.-Y. Kim, H.-Y. Lee, C. Lee, Metformin targets Axl and Tyro3 receptor tyrosine kinases to inhibit cell proliferation and overcome chemoresistance in ovarian cancer cells. Int. J. Oncol. 47(1), 353–360 (2015).
E. Lengyel et al. Metformin inhibits ovarian cancer growth and increases sensitivity to paclitaxel in mouse models. Am. J. Obstet. Gynecol. 212(4), 479 (2015).
J.H. Dang et al. Metformin in combination with cisplatin inhibits cell viability and induces apoptosis of human ovarian cancer cells by inactivating ERK 1/2. Oncol. Lett. 14(6), 7557–7564 (2017).
R. Erices et al. Diabetic concentrations of metformin inhibit platelet-mediated ovarian cancer cell progression. Oncotarget 8(13), 20865 (2017).
X. Yang et al. Metformin antagonizes ovarian cancer cells malignancy through MSLN mediated IL-6/STAT3 signaling. Cell Transplant. 30, 09636897211027819 (2021).
R. Rattan, R.P. Graham, J.L. Maguire, S. Giri, V. Shridhar, Metformin suppresses ovarian cancer growth and metastasis with enhancement of cisplatin cytotoxicity in vivo. Neoplasia 13(5), 483–IN28 (2011).
K. Yao, H. Zheng, T. Li, Association between metformin use and the risk, prognosis of gynecologic cancer. Front. Oncol. 12, 942380 (2022). https://doi.org/10.3389/fonc.2022.942380.
Y. Zheng, J. Zhu, H. Zhang, Y. Liu, H. Sun, Metformin plus first-line chemotherapy versus chemotherapy alone in the treatment of epithelial ovarian cancer: a prospective open-label pilot trial. Cancer Chemother. Pharmacol. 84(6), 1349–1357 (2019).
M.R. Khawaja et al. Phase I dose escalation study of temsirolimus in combination with metformin in patients with advanced/refractory cancers. Cancer Chemother. Pharmacol. 77(5), 973–977 (2016).
J.R. Brown et al., Phase II clinical trial of metformin as a cancer stem cell-targeting agent in ovarian cancer. JCI Insight 5(11) (2020). https://doi.org/10.1172/jci.insight.133247.
M. Jensterle, A. Janez, B. Mlinar, J. Marc, J. Prezelj, M. Pfeifer, Impact of metformin and rosiglitazone treatment on glucose transporter 4 mRNA expression in women with polycystic ovary syndrome. Eur. J. Endocrinol. 158(6), 793–801 (2008).
S.J. Lessard et al. Rosiglitazone enhances glucose tolerance by mechanisms other than reduction of fatty acid accumulation within skeletal muscle. Endocrinology 145(12), 5665–5670 (2004).
A. Aljada, L. O’Connor, Y.-Y. Fu, S.A. Mousa, PPARγ ligands, rosiglitazone and pioglitazone, inhibit bFGF-and VEGF-mediated angiogenesis. Angiogenesis 11(4), 361–367 (2008).
H. Zhang et al. Suppression of multidrug resistance by rosiglitazone treatment in human ovarian cancer cells through downregulation of FZD1 and MDR1 genes. Anticancer Drugs 26(7), 706–715 (2015). https://doi.org/10.1097/cad.0000000000000236.
T. Nargis, P. Chakrabarti, Significance of circulatory DPP4 activity in metabolic diseases. IUBMB Life 70(2), 112–119 (2018).
A. Kosowska, et al., Sitagliptin modulates the response of ovarian cancer cells to chemotherapeutic agents. Int. J. Mol. Sci. 21(23), 8976 (2020). https://www.mdpi.com/1422-0067/21/23/8976.
Acknowledgements
The authors thank Behbahan Faculty of Medical Sciences for financial support.
Funding
This research was supported by the Behbahan Faculty of Medical Sciences (Grant # 401044) and F.K. has received research support from Behbahan Faculty of Medical Sciences.
Author information
Authors and Affiliations
Contributions
F.K. contributed to the study conception and design. The first draft of the manuscript was written by F.K. and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Karimi, F., Dinarvand, N., Sabaghan, M. et al. Diabetes and ovarian cancer: risk factors, molecular mechanisms and impact on prognosis. Endocrine 83, 1–9 (2024). https://doi.org/10.1007/s12020-023-03477-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-023-03477-6