Abstract
Purpose
In women with Polycystic Ovarian Syndrome (PCOS), an increased risk of disordered eating has been described. There is growing interest regarding a possible interconnection between psychological states and increased appetite in women with PCOS. Acute stress is characterized by increased Corticotropin Releasing Hormone (CRH) secretion. The aim was to estimate the ghrelin concentrations during CRH test.
Methods
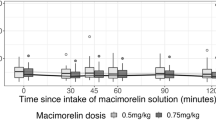
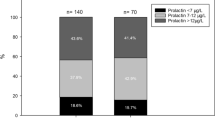
Twenty postmenopausal women with PCOS and twenty age- and BMI- matched postmenopausal control women were recruited at Aretaieion University Hospital. In the morning (9 am) all subjects had anthropometric measurements (weight, height, waist circumference) and a fasting sample for hormonal measurements. An intravenous (iv) CRH stimulation test conducted over 1 min. Serum active ghrelin levels were measured at 0, 15, 30, 60, 90, 120 min after iv CRH administration.
Results
The postmenopausal PCOS group had a higher waist circumference compared to postmenopausal controls. Active ghrelin concentrations increased significantly from 0 to 15 min, to 30 min, to 60 min, to 90 min and then decreased to 120 min. However, within the postmenopausal control group there were no significant changes in serum active ghrelin levels. Serum active ghrelin concentrations were significantly greater in the postmenopausal control group at 0, 15 and 120 min compared to the postmenopausal PCOS group. At 90 min active ghrelin concentrations were significantly greater in the postmenopausal PCOS group. Delta Area Under the Curve of active ghrelin (ΔAUCghr) was significantly greater in the postmenopausal PCOS group compared to controls.
Conclusions
In postmenopausal PCOS, but not in postmenopausal controls, iv CRH administration induces increased serum active ghrelin secretion, suggesting a possible anti-stress adaptive mechanism. An increase in serum active ghrelin may induce hunger as a side-effect of this presumed adaptive mechanism.


Similar content being viewed by others
References
N.F. Goodman, R.H. Cobin, W. Futterweit, J.S. Glueck, R.S. Legro, E. Carmina, American Association of Clinical Endocrinologists (AACE); American College of Endocrinology (ACE); Androgen Excess and PCOS Society (AES). Clinical guide to the best practices in the evaluation and treatment of Polycystic Ovary Syndrome. Endocr. Pract. 21, 1291–300 (2015)
I. Lee, L.G. Cooney, S. Saini, M.E. Smith, M.D. Samel, K.C. Allison, A. Dokras, Increased risk of disordered eating in polycystic ovary syndrome. Fertil. Steril. 107, 796–802 (2017)
Bear MH, Reddy V, Bollu PC: Neuroanatomy, Hypothalamus. In: Stat pearls. Treasure Island (FL): StatPearls Publishing (2022).
D. Barlampa, M.S. Bompoula, A. Bargiota, S. Kalantaridou, G. Mastorakos, G. Valsamakis, Hypothalamic Inflammation as a Potential Pathophysiologic Basis for the Heterogeneity of Clinical, Hormonal, and Metabolic Presentation in PCOS. Nutr 13, 520 (2021)
M.A. Charifson, B.C. Trumble, Evolutionary origins of polycystic ovary syndrome: An environmental mismatch disorder. Evol. Med. Public Health 1, 50–63 (2019)
S. Benson, P.C. Arck, S. Tan, S. Hahn, K. Mann, K. Rifaie, O.E. Janssen, M. Schedlowski, S. Elsenbruch, Disturbed stress responses in women with polycystic ovary syndrome. Psychoneuroendocrinol 34, 727–735 (2009)
A.L. Damone, J.D. Loxton, A. Earnest, L.J. Moran, Depression, anxiety and perceived stress in women with and without PCOS: A community-based study. Psychol. Med. 49, 1510–1520 (2019)
J.S. Kim, S.Y. Han, K.J. Iremonger, Stress experience and hormone feedback tune distinct components of hypothalamic CRH neuron activity. Nat. Commun. 10, 5696 (2019)
S.C. Weninger, A.J. Dunn, L.J. Muglia, P. Dikkes, K.A. Miczek, A.H. Swiergiel, C.W. Berridge, J.A. Majzoub, Stress-induced behaviors require the corticotropin-releasing hormone (CRH) receptor, but not CRH. PNAS 96, 8283–8288 (1999)
B.R. Basu, O. Chowdhury, S.K. Saha, Possible Link Between Stress-related Factors and Altered Body. J. Hum. Reprod. Sci. 11, 10–18 (2018)
L.J. Moran, M. Noakes, P.M. Clifton, G.A. Wittert, L. Tomlinson, C. Galletly, N.D. Luscombe, R.J. Norman, Ghrelin and measures of satiety are altered in polycystic ovary syndrome but not differentially affected by diet composition. J. Clin. Endocrinol. Metab. 89, 3337–44 (2004)
H.J. Teede, A.E. Joham, E. Paul, L.J. Moran, D. Loxton, D. Jolley, C. Lombard, Longitudinal weight gain in women identified with polycystic ovary syndrome: results of an observational study in young women. Obesity 21, 1526–32 (2013)
D. Glintborg, A. Houborg, M. Petersen, P. Ravn, A.P. Hermann, M. Andersen, Comparison of regional fat mass measurement by whole body DXA scans and anthropometric measures to predict insulin resistance in women with polycystic ovary syndrome and controls. Acta Obstet. Gynecol. Scan. 95, 1235–1243 (2016)
L. Hajivandi, M. Noroozi, F. Mostafavi, M. Ekramzadeh, Food habits in overweight and obese adolescent girls with Polycystic ovary syndrome (PCOS): a qualitative study in Iran. BMC Pediatr. 20, 277 (2020)
G. Muccioli, M. Tschop, M. Pappoti, R. Deghenghi, E. Ghigo, Neuroendocrine and peripheral activities of ghrelin: Implications in metabolism and obesity. Eur. J. Pharmacol. 440, 235–254 (2002)
C. Schöfl, R. Horn, T. Schill, H.W. Schlösser, M.J. Müller, G. Brabant, Circulating ghrelin levels in patients with polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 87, 4607–4610 (2002)
J. Rodin, Insulin levels, hunger, and food intake: An example of feedback loops in body weight regulation. Health Psychol. 4, 1–24 (1985)
A. Tchernof, J. Calles-Escandon, C.K. Sites, E.T. Poehlman, Menopause, central body fatness, and insulin resistance: effects of hormone-replacement therapy. Coron. Arter. Dis. 9, 503–11 (1998)
M. Markopoulos, G. Valsamakis, E. Kouskouni, A. Boutsiadis, I. Papassotiriou, G. Creatsas, G. Mastorakos, Study of carbohydrate metabolism indices and adipocytokine profile and their relationship with androgens in polycystic ovary syndrome after menopause. Eur. J. Endocrinol. 168, 83–90 (2012)
D.H. St Pierre, A.D. Karelis, L. Coderre, F. Marita, J. Fontaine, D. Mignault, M. Brochu, J.P. Bastard, K. Cianflone, E. Doucet, P. Imbeault, R. Lauret, Association of acylated and nonacylated ghrelin with insulin sensitivity in overweight and obese postmenopausal women. J. Clin. Endocrinol. Metab. 92, 264–269 (2007)
A. Gambineri, C. Pelusi, V. Vicennati, U. Pagotto, R. Pasquali, Obesity and the polycystic ovary syndrome. Int. J. Obes. 26, 883–896 (2002)
R. Azziz, Controversy in clinical endocrinology: diagnosis of polycystic ovary syndrome: The Rotterdam criteria are premature. J. Clin. Endocrinol. Metab. 91, 781–5 (2006)
T.M. Wallace, J.C. Levy, D.R. Matthews, Use and abuse of HOMA modeling. Diab. Care 27, 1487–1495 (2004)
G.P. Chrousos, H.M. Schulte, E.H. Oldfield, P.W. Gold, G.B. Cutler Jr, D.L. Loriaux, The corticotropin-releasing factor stimulation test. An aid in the evaluation of patients with Cushing’s. N. Engl. J. Med. 310, 622–626 (1984)
D. Falconnet, J. She, R. Tornay, E. Leimgruber, D. Bernasconi, L. Lagopoulos, P. Renaud, N. Demierre, P. van den Bogaard, Rapid, sensitive and real-time multiplexing platform for the analysis of protein and nucleic-acid biomarkers. Anal. Chem. 3(87), 1582–1589 (2015)
S.A. Dunbar, Applications of Luminex xMAP technology for rapid, high-throughput multiplexed nucleic acid detection. Clin. Chim. Acta 363, 71–82 (2006)
L. Chang, The role of stress on physiologic responses and clinical symptoms in irritable bowel syndrome. Gastroenterol 140, 761–5 (2011)
A. Stengel, Y. Trache, Corticotropin-releasing factor signaling and visceral response to stress. Exp. Biol. Med. 235, 1168–78 (2010)
S. Fukudo, J. Suzuki, Colonic motility, autonomic function and gastrointestinal hormones under psychological stress on irritable bowel syndrome. Tohuku J. Exp. Med. 151, 373–385 (1987)
Furman B. Corticotropin Releasing Factor. xPharm The Comprehensive Pharmacology Reference 1–4 (2007)
F.M. Dautzenberg, R.L. Hauger, The CRF peptide family and their receptors: yet more partners discovered. Trends Pharm. 23, 71–7 (2002)
S. Liu, W. Ren, M.H. Qu, G.A. Bishop, G.D. Wang, X.Y. Wang, Y. Xia, J.D. Wood, Expression of type 1 corticotropin –releasing factor receptor in the guinea pig enteric nervous system. J. Comp. Neurol. 481, 284–298 (2005)
E. Chatzaki, B.J. Murphy, L. Wang, M. Million, G.V. Ohning, P.D. Crowe, R. Petroski, Y. Tache, D.E. Grigoriadis, Differential profile of CRF receptor distribution in the rat stomach and duodenum assessed by newly developed CRF receptor antibodies. J. Neurochem. 88, 1–11 (2004)
E. Chatzaki, M. Lambropoulou, T.C. Constantinidis, N. Papadopoulos, Y. Tache, G. Minopoulos, D.E. Grigoriadis, Corticotropin releasing factor receptor type 2 in the human stomach: protective biological role by inhibition of apoptosis. J. Cell Physiol. 209, 905–911 (2006)
C. Porcher, A. Peinnequin, S. Pelissier, J. Meregnani, V. Sinniger, F. Canini, B. Bonaz, Endogenous expression and in vitro study of CRF related peptides and CRF receptors in the rat gastric antrum. Peptides 27, 1464–1475 (2006)
R.R. Banerjee, S.M. Rangwala, J.S. Shapiro, Regulation of fasted blood glucose by resistin. Sci 303, 1195–8 (2004)
R. Kimura, D. Kondo, S. Takemi, M. Fujishiro, S. Tsukahara, T. Sakai, I. Sakata, The role of central corticotrophin –releasing factor receptor signaling in plasma glucose maintenance through ghrelin secretion in calorie restricted mice. J. Neuroendocrinol. 33, e 12961 (2021). 10.111/jne.12961
E. Kristensson, M. Sundqvist, M. Astin, M. Kjerling, H. Mattsson, C. Dornonville De La Cour, Acute psychological stress raises plasma ghrelin in the rat. Regul. Pept. 134, 114–117 (2006)
M.V. Schmidt, S. Levine, S. Alam, D. Harbich, V. Sterlemann, K. Ganea, E.R. de Kloet, F. Holsboer, M.V. Muller, Metabolic signals modulate hypothalamic-pituitary-adrenal axis activation during maternal separation of the neonatal mouse. J. Neuroendocrinol. 18, 865–874 (2006)
U. Pagotto, A. Gambineri, V. Vicennati, M.L. Heiman, M. Tschop, R. Pasquali, Plasma ghrelin obesity and the polycystic ovary syndrome: correlation with insulin resistance and androgen levels. J. Clin. Endocrinol. Metab. 87, 5625–5629 (2002)
T. Shiiya, M. Nakazato, M. Mizuta, Y. Date, M.S. Mondal, M. Tanaka, S. Nozoe, K. Kangawa, S. Matsukura, Plasma ghrelin levels in lean and obese humans and the effect of glucose on ghrelin secretion. J. Clin. Endocrinol. Metab. 87, 240–244 (2002)
T.M. Barber, F.F. Casanueva, M. Lage, S. Franks, M.I. McCarthy, J.A.H. Wass, Ghrelin is reduced in women with polycystic ovary syndrome and correlates inversely with HOMA IR and testosterone. Endocr. Abstr. 13, 254 (2007)
A. Pavicic, D. Baldani, L. Srgatic, M. Kasum, G. Zlopasa, S. Oguis, M. Herman, Altered leptin, adiponectin, resistin and ghrelin secretion may represent an intrinsic polycystic ovary syndrome abnormality. Gynecol. Endocrinol. 35, 401–405 (2019)
T. Gao, L. Wu, F. Chang, G. Cao, Low circulating ghrelin levels in women with polycystic ovary syndrome: A systematic review and meta-analysis. Endocr. J. 63, 93–100 (2016)
P. Marzullo, B. Verti, G. Savia, G.E. Walker, G. Guzzaloni, M. Tagliaferri, A. Di Blasio, A. Liuzzi, The Relationship between active ghrelin levels and human obesity involves alterations in resting energy expenditure. J. Clin. Endocrinol. Metab. 89, 936–939 (2004)
K. Raspopow, A. Abizaid, K. Matheson, H. Anisman, Psychosocial stressor effects on cortisol and ghrelin in emotional and non-emotional eaters: influence of anger and shame. Horm. Behav. 58, 677–684 (2010)
P. Monteleone, A. Tortorella, P. Scognamiglio, I. Serino, A.M. Monteleone, M. Maj, The acute salivary ghrelin response to a psychosocial stress is enhanced in symptomatic patients with bulimia nervosa: a pilot study. Neuropsychobiol 66, 230–236 (2012)
S.J. Spencer, L. Xu, M.A. Clarke, M. Lemus, A. Reichenbach, B. Geenen, T. Kozicz, J.B. Anrews, Ghrelin regulates the Hypothalamic-Pituitary-Adrenal axis and restrict s anxiety after acute stress. Biol. Psychiatry 72, 457–465 (2012)
M. Lutter, I. Sakata, L.S. Osborne, S.A. Rovinsky, J.G. Andersson, S. Jung, S. Birnbaum, M. Yanagisawa, J.K. Elmquist, E.J. Nestler, J.M. Zigman, Nat. Neurosci. 11, 752–753 (2008)
M.A. Hedegaard, B. Holst, The complex signaling pathways of the ghrelin receptor. Endocrinol 161, 4 (2020)
C. Hansson, M. Alvarez-Crespo, M. Taube, K.P. Skibicka, L. Schmidt, L. Karlsson-Lindahl et al. Influence of ghrelin on the central serotonergic signaling system in mice. Neuropharmacology 79, 498–505 (2014). (2014)
A. Kawakami, N. Okada, K. Rokkaku, K. Honda, S. Ishibashi, T. Onaka, Leptin inhibits and ghrelin augments hypothalamic noradrenaline release after stress. Stress 11, 363–369 (2008)
I. Merchenthaler, M.A. Hynes, S. Vigh, A.V. Schally, P. Petrusz, Immunocytochemical localization of corticotropin releasing factor (CRF) in the rat spinal cord. Brain Res. 275, 373–377 (1983)
R. Udelsman, J.P. Harwood, M.A. Millan, G.P. Chrousos, G.S. Goldstein, R. Zimlichman, K.J. Catt, G. Aguilera, Functional corticotropin releasing factor receptors in the primate peripheral sympathetic nervous system. Nat. (Lond.) 319, 147–150 (1986)
R.J. Valentino, L.A. Pavcovich, H. Hirata, Evidence for corticotropin-releasing hormone projections from Barrington’s nucleus to the periaqueductal gray and dorsal motor nucleus of the vagus in the rat. J. Comp. Neurol. 18(363), 402–22 (1995)
Funding
This work received fund (No 1535, to G.M.) by the Ethnikon and Kapodistriakon University of Athens.
Author information
Authors and Affiliations
Contributions
M.M. data collection and methodology. T.M.B. and S.K.: critical revision, design. A.B.: analysis of data, design. C.S., and I.P.: analysis of data. N.F.V.: final approval. G.M.: critical review, design, resources. G.V.: conceptualization, design, interpretation, drafting, final approval.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
This study was performed in line with principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee Aretaieion University Hospital Ethnikon and Kapodistriakon University of Athens (1535, Aretaieion Hospital, June 2011).
Consent to publish
All subjects signed written informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Markopoulos, M., Barber, T.M., Bargiota, A. et al. Acute iv CRH administration significantly increases serum active ghrelin in postmenopausal PCOS women compared to postmenopausal controls. Endocrine 81, 613–620 (2023). https://doi.org/10.1007/s12020-023-03406-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-023-03406-7