Abstract
Purpose
Patients with Cushing’s disease (CD) experienced transient central adrenal insufficiency (CAI) after successful surgery. However, the reported recovery time of hypothalamic-pituitary-adrenal (HPA) axis varied and the related factors which could affect recovery time of HPA axis had not been extensively studied. This study aimed to analyze the duration of CAI and explore the factors affecting HPA axis recovery in post-operative CD patients with biochemical remission.
Methods
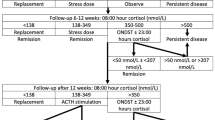
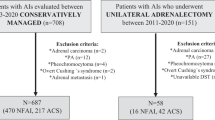
Medical records of diagnosis with CD in Huashan Hospital were reviewed between 2014 and 2020. 140 patients with biochemical remission and regular follow-up after surgery were enrolled in this retrospective cohort study according to the criteria. Demographic details, clinical and biochemical information at baseline and each follow-up (within 2 years) were collected and analyzed.
Results
Overall, 103 patients (73.6%) recovered from transient CAI within 2 years follow-up and the median recovery time was 12 months [95% confidence intervals (CI): 10–14]. The age was younger and midnight ACTH at baseline was significantly lower, while the TT3 and FT3 levels were significantly higher in patients with recovered HPA compared to patients with persistent CAI at 2-year follow-up (p < 0.05). In persistent CAI group, more patients underwent partial hypophysectomy. TT3 at diagnosis was an independent related factor of the recovery of HPA axis, even after adjusting for gender, age, duration, surgical history, maximum tumor diameter, surgical strategy, and postoperative nadir serum cortisol level (p = 0.04, OR: 6.03, 95% CI: 1.085, 22.508). Among patients with unrecovered HPA axis at 2-year follow-up, 23 CAI patients (62%) were accompanied by multiple pituitary axis dysfunction besides HPA axis, including hypothyroidism, hypogonadism, or central diabetes insipidus.
Conclusion
HPA axis recovered in 73.6% of CD patients within 2 years after successful surgery, and the median recovery time was 12 months. TT3 level at diagnosis was an independent related factor of postoperative recovery of HPA axis in CD patients. Moreover, patients coexisted with other hypopituitarism at 2-year follow-up had a high probability of unrecovered HPA axis.




Similar content being viewed by others
Data availability
The data are available on request from the authors.
Abbreviations
- ACTH:
-
adrenocorticotrophic hormone
- TT3:
-
total triiodothyronine
- FT3:
-
free triiodothyronine
- UFC:
-
urinary free cortisol
- PRL:
-
prolactin
- FSH:
-
follicle-stimulating hormone
- LH:
-
luteinizing hormone
- TT4:
-
total thyroxine
- FT4:
-
free thyroxine
- TSH:
-
thyroid-stimulating hormone
- IGF-1:
-
insulin-like growth factor 1
- HbA1c:
-
hemoglobin A1c
- TC:
-
total cholesterol
- TG:
-
triglyceride
- SBP:
-
systolic blood pressure
- DBP:
-
diastolic blood pressure
- IPSS:
-
Inferior Petrosal Sinus Sampling
References
B.M. Biller, A.B. Grossman, P.M. Stewart et al. Treatment of adrenocorticotropin-dependent Cushing’s syndrome: a consensus statement. J. Clin. Endocrinol. Metab. 93, 2454–2462 (2008). https://doi.org/10.1210/jc.2007-2734
L.K. Nieman, B.M. Biller, J.W. Findling et al. The diagnosis of Cushing’s syndrome: an Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 93, 1526–1540 (2008). https://doi.org/10.1210/jc.2008-0125
L.K. Nieman, B.M. Biller, J.W. Findling et al. Treatment of Cushing’s syndrome: an endocrine society clinical practice guideline. J Clin. Endocrinol Metab. 100, 2807–2831 (2015). https://doi.org/10.1210/jc.2015-1818
R.M. Paragliola, G. Papi, A. Pontecorvi, et al. (2017) Treatment with synthetic glucocorticoids and the hypothalamus-pituitary-adrenal axis. Int J. Mol. Sci. 18, https://doi.org/10.3390/ijms18102201.
C.M. Berr, G. Di Dalmazi, A. Osswald et al. Time to recovery of adrenal function after curative surgery for Cushing’s syndrome depends on etiology. J. Clin. Endocrinol. Metab. 100, 1300–1308 (2015). https://doi.org/10.1210/jc.2014-3632
M.I. Khan, M.A. Habra, I.E. McCutcheon et al. Random postoperative day-3 cortisol concentration as a predictor of hypothalamic-pituitary-adrenal axis integrity after transsphenoidal surgery. Endocrine Pract. 17, 717–726 (2011). https://doi.org/10.4158/ep11013.Or
A.L. Serban, E. Sala, G. Carosi et al. Recovery of adrenal function after pituitary surgery in patients with cushing disease: persistent remission or recurrence? Neuroendocrinology 108, 211–218 (2019). https://doi.org/10.1159/000496846
M. Fleseriu, R. Auchus, I. Bancos et al. Consensus on diagnosis and management of Cushing’s disease: a guideline update. Lancet Diabetes Endocrinol. 9, 847–875 (2021). https://doi.org/10.1016/s2213-8587(21)00235-7
C. Dai, M. Feng, B. Sun et al. Surgical outcome of transsphenoidal surgery in Cushing’s disease: a case series of 1106 patients from a single center over 30 years. Endocrine 75, 219–227 (2022). https://doi.org/10.1007/s12020-021-02848-1
E. Valassi, B.M. Biller, B. Swearingen et al. Delayed remission after transsphenoidal surgery in patients with Cushing’s disease. J Clin. Endocrinol Metab. 95, 601–610 (2010). https://doi.org/10.1210/jc.2009-1672
X. He, J. Findling, R.J.P. Auchus, (2022) Glucocorticoid withdrawal syndrome following treatment of endogenous Cushing Syndrome. https://doi.org/10.1007/s11102-022-01218-y.
E.V. Varlamov, G. Vila, M. Fleseriu, Perioperative management of a patient with cushing disease. J. Endocrine Soc. 6, bvac010 (2022). https://doi.org/10.1210/jendso/bvac010
Q. Cui, D. Liu, B. Xiang et al. Morning serum cortisol as a predictor for the HPA axis recovery in cushing’s disease. Int. J. Endocrinol. 2021, 4586229 (2021). https://doi.org/10.1155/2021/4586229
M. Fleseriu, I.A. Hashim, N. Karavitaki et al. Hormonal replacement in hypopituitarism in adults: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 101, 3888–3921 (2016). https://doi.org/10.1210/jc.2016-2118
C.P.A.S. Council, Consensus of Chinese experts on diagnosis and treatment of Cushing’s disease. Natl. Med. J. China 96, 835–840 (2015)
C. Tatsi, M. Neely, C. Flippo et al. Recovery of hypothalamic-pituitary-adrenal axis in paediatric Cushing disease. Clin. Endocrinol. 94, 40–47 (2021). https://doi.org/10.1111/cen.14300
M. Lodish, S.V. Dunn, N. Sinaii et al. Recovery of the hypothalamic-pituitary-adrenal axis in children and adolescents after surgical cure of Cushing’s disease. J. Clin. Endocrinol. Metab. 97, 1483–1491 (2012). https://doi.org/10.1210/jc.2011-2325
M. Klose, K. Jørgensen, L. Kristensen, Characteristics of recovery of adrenocortical function after treatment for Cushing’s syndrome due to pituitary or adrenal adenomas. Clin. Endocrinol. 61, 394–399 (2004). https://doi.org/10.1111/j.1365-2265.2004.02111.x
R.N. Re, I.A. Kourides, E.C. Ridgway et al. The effect of glucocorticoid administration on human pituitary secretion of thyrotropin and prolactin. J. Clin. Endocrinol. Metab. 43, 338–346 (1976). https://doi.org/10.1210/jcem-43-2-338
T.J. Visser, S.W. Lamberts, Regulation of TSH secretion and thyroid function in Cushing’s disease. Acta endocrinologica 96, 480–483 (1981). https://doi.org/10.1530/acta.0.0960480
R.M. Paragliola, A. Corsello, G. Papi, et al. (2021) Cushing’s syndrome effects on the thyroid. Int. J. Mol. Sci. 22, https://doi.org/10.3390/ijms22063131.
S. Shekhar, R. McGlotten, S. Auh et al. The hypothalamic-pituitary-thyroid axis in cushing syndrome before and after curative surgery. J. Clin. Endocrinol. Metab. 106, e1316–e1331 (2021). https://doi.org/10.1210/clinem/dgaa858
B. Xiang, R. Tao, X. Liu et al. A study of thyroid functions in patients with Cushing’s syndrome: a single-center experience. Endocrine Connections 8, 1176–1185 (2019). https://doi.org/10.1530/ec-19-0309
H. Zheng, Q. Wang, Q. Cui et al. The hypothalamic-pituitary-gonad axis in male Cushing’s disease before and after curative surgery. Endocrine 77, 357–362 (2022). https://doi.org/10.1007/s12020-022-03083-y
S. Sciacchitano, C. Capalbo, C. Napoli et al. Nonthyroidal illness syndrome: to treat or not to treat? have we answered the question? a review of metanalyses. Front. Endocrinol. 13, 850328 (2022). https://doi.org/10.3389/fendo.2022.850328
Acknowledgements
We are indebted to the patients who participated in this study and all the doctors contributing to the diagnosis and treatment of these patients. This work was supported by grants from Multidisciplinary Diagnosis and Treatment (MDT) demonstration project in research hospitals (Shanghai Medical College, Fudan University, NO: DGF501053-2/014).
Author contributions
Q.C. analyzed the data and wrote the manuscript. Q.C., X.L., Q.S., W.S. and H.Z. collected the data. Z.M., M.S., X.S., Y.W. and Y.Z. performed transsphenoidal surgeries. Y.L. and Z.Z. revised the study and manuscript. S.Z. and M.H. recruited patients. H.Y. and S.Z. conducted the study design and quality control. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cui, Q., Liu, X., Sun, Q. et al. The recovery time of hypothalamic-pituitary-adrenal axis after curative surgery in Cushing’s disease and its related factor. Endocrine 81, 349–356 (2023). https://doi.org/10.1007/s12020-023-03405-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-023-03405-8