Abstract
Background
Using machine learning (ML) to explore the noninvasive differential diagnosis of Cushing’s disease (CD) and ectopic corticotropin (ACTH) secretion (EAS) model is the next hot research topic. This study was to develop and evaluate ML models for differentially diagnosing CD and EAS in ACTH-dependent Cushing’s syndrome (CS).
Methods
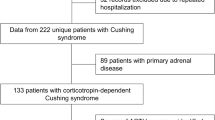
Two hundred sixty-four CD and forty-seven EAS were randomly divided into training and validation and test datasets. We applied 8 ML algorithms to select the most suitable model. The diagnostic performance of the optimal model and bilateral petrosal sinus sampling (BIPSS) were compared in the same cohort.
Results
Eleven adopted variables included age, gender, BMI, duration of disease, morning cortisol, serum ACTH, 24-h UFC, serum potassium, HDDST, LDDST, and MRI. After model selection, the Random Forest (RF) model had the most extraordinary diagnostic performance, with a ROC AUC of 0.976 ± 0.03, a sensitivity of 98.9% ± 4.4%, and a specificity of 87.9% ± 3.0%. The serum potassium, MRI, and serum ACTH were the top three most important features in the RF model. In the validation dataset, the RF model had an AUC of 0.932, a sensitivity of 95.0%, and a specificity of 71.4%. In the complete dataset, the ROC AUC of the RF model was 0.984 (95% CI 0.950–0.993), which was significantly higher than HDDST and LDDST (both p < 0.001). There was no significant statistical difference in the comparison of ROC AUC between the RF model and BIPSS (baseline ROC AUC 0.988 95% CI 0.983–1.000, after stimulation ROC AUC 0.992 95% CI 0.983–1.000). This diagnostic model was shared as an open-access website.
Conclusions
A machine learning-based model could be a practical noninvasive approach to distinguishing CD and EAS. The diagnostic performance might be close to BIPSS.





Similar content being viewed by others
References
M. Fleseriu, R. Auchus, I. Bancos et al. Consensus on diagnosis and management of Cushing’s disease: a guideline update. Lancet Diabetes Endocrinol. 9(12), 847–875 (2021). https://doi.org/10.1016/s2213-8587(21)00235-7
L.K. Nieman, Molecular derangements and the diagnosis of ACTH-dependent Cushing’s syndrome. Endocr. Rev. (2021). https://doi.org/10.1210/endrev/bnab046
C. Frete, J.B. Corcuff, E. Kuhn et al. Non-invasive diagnostic strategy in ACTH-dependent Cushing’s syndrome. J. Clin. Endocrinol. Metab. 105(10) (2020). https://doi.org/10.1210/clinem/dgaa409
K. Ritzel, F. Beuschlein, C. Berr et al. ACTH after 15 min distinguishes between Cushing’s disease and ectopic Cushing’s syndrome: a proposal for a short and simple CRH test. Eur. J. Endocrinol. 173(2), 197–204 (2015). https://doi.org/10.1530/eje-14-0912
E.R. Laws, M.P. Catalino, Editorial. Machine learning and artificial intelligence applied to the diagnosis and management of Cushing disease. Neurosurg. Focus 48(6), E6 (2020). https://doi.org/10.3171/2020.3.focus20213
Y. Fan, Y. Li, X. Bao et al. Development of machine learning models for predicting postoperative delayed remission in patients with Cushing’s disease. J. Clin. Endocrinol. Metab. 106(1), e217–e231 (2021). https://doi.org/10.1210/clinem/dgaa698
T.C. Hollon, A. Parikh, B. Pandian et al. A machine learning approach to predict early outcomes after pituitary adenoma surgery. Neurosurg. Focus 45(5), E8 (2018). https://doi.org/10.3171/2018.8.Focus18268
Y. Liu, X. Liu, X. Hong et al. Prediction of recurrence after transsphenoidal surgery for Cushing’s disease: the use of machine learning algorithms. Neuroendocrinology 108(3), 201–210 (2019). https://doi.org/10.1159/000496753
W. Zhang, D. Li, M. Feng et al. Electronic medical records as input to predict postoperative immediate remission of Cushing’s disease: application of word embedding. Front. Oncol. 11, 754882 (2021). https://doi.org/10.3389/fonc.2021.754882
W. Zhang, M. Sun, Y. Fan et al. Machine learning in preoperative prediction of postoperative immediate remission of histology-positive Cushing’s disease. Front. Endocrinol. 12, 635795 (2021). https://doi.org/10.3389/fendo.2021.635795
M. Zoli, V.E. Staartjes, F. Guaraldi et al. Machine learning–based prediction of outcomes of the endoscopic endonasal approach in Cushing disease: is the future coming. Neurosurg. Focus 48(6), E5 (2020). https://doi.org/10.3171/2020.3.focus2060
S. Shahrestani, T. Cardinal, A. Micko et al. Neural network modeling for prediction of recurrence, progression, and hormonal non-remission in patients following resection of functional pituitary adenomas. Pituitary 24(4), 523–529 (2021). https://doi.org/10.1007/s11102-021-01128-5
S. Isci, D.S.Y. Kalender, F. Bayraktar, A. Yaman, Machine learning models for classification of Cushing’s syndrome using retrospective data. IEEE J. Biomed. Health Inf. 25(8), 3153–3162 (2021). https://doi.org/10.1109/JBHI.2021.3054592
W. Luo, D. Phung, T. Tran et al. Guidelines for developing and reporting machine learning predictive models in biomedical research: a multidisciplinary view. J. Med. Internet Res. 18(12), e323 (2016). https://doi.org/10.2196/jmir.5870. 2016/12/16
F. Pedregosa, G. Varoquaux, A. Gramfort et al. Scikit-learn: machine learning in Python. J. Mach. Learn. Res. 12, 2825–2830 (2011)
E.H. Oldfield, J.L. Doppman, L.K. Nieman et al. Petrosal sinus sampling with and without corticotropin-releasing hormone for the differential diagnosis of Cushing’s syndrome. N. Engl. J. Med. 325(13), 897–905 (1991). https://doi.org/10.1056/nejm199109263251301
C. Cortes, V. Vapnik, Support-vector networks. Mach. Learn. 20(3), 273–297 (1995). https://doi.org/10.1007/BF00994018
N.S. Altman, An introduction to kernel and nearest-neighbor nonpara-metric regression. Am. Stat. 46, 175–185 (1992)
S.C. Bagley, H. White, B.A. Golomb, Logistic regression in the medical literature: standards for use and reporting, with particular attention to one medical domain. J. Clin. Epidemiol. 54(10), 979–985 (2001). https://doi.org/10.1016/s0895-4356(01)00372-9
A. Tharwat, Principal component analysis—a tutorial. Int. J. Appl. Pattern Recognit. 3(3), 197–240 (2016). https://doi.org/10.1504/IJAPR.2016.079733
L. Breiman, C.J. Stone, R.A. Olshen. Classification and Regression Trees. (CRC Press, USA, 1984)
L. Breiman, C.J. Stone, R.A. Olshen, Random forests. Mach. Learn. 45(no. 1), 5–32 (2001)
Y. Freund, R.E. Schapire, Experiments with a New Boosting Algorithm, pp. 148–156 (Citeseer, 1996)
J.H. Friedman, Stochastic gradient boosting. Comput. Stat. Data Anal. 38(4), 367–378 (2002)
S. Varma, R. Simon, Bias in error estimation when using cross-validation for model selection. BMC Bioinforma. 7(1), 1–8 (2006)
S.B. Blunt, L.M. Sandler, J.M. Burrin, G.F. Joplin, An evaluation of the distinction of ectopic and pituitary ACTH dependent Cushing’s syndrome by clinical features, biochemical tests and radiological findings. Q. J. Med. 77(283), 1113–1133 (1990). https://doi.org/10.1093/qjmed/77.2.1113
M. Barbot, L. Trementino, M. Zilio et al. Second-line tests in the differential diagnosis of ACTH-dependent Cushing’s syndrome. Pituitary 19(5), 488–495 (2016). https://doi.org/10.1007/s11102-016-0729-y
K. Chen, S. Chen, L. Lu et al. An optimized pathway for the differential diagnosis of ACTH-dependent Cushing’s syndrome based on low-dose dexamethasone suppression test. Front. Endocrinol. 12, 720823 (2021). https://doi.org/10.3389/fendo.2021.720823
Acknowledgements
We are grateful to Mr. Yi Lyu and Mr. Peiyu Wang for their guidance and help with the methodology of this study.
Funding
National High Level Hospital Clinical Research Funding (2022-PUMCH-B-016). National College Student Innovation and Entrepreneurship Training Program (2022zglc06080). Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (2021-I2M-1-023).
Author information
Authors and Affiliations
Contributions
S.C., L.L., H.P., and H.Z. contributed to the study conception and design. Data collection was finished by D.Z. Data analysis was performed by X.L. The first draft of the manuscript was written by X.L. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of PUMCH, Chinese Academy of Medical Sciences (approval number: JS1233). Patients signed informed consent before information and blood samples were collected and approved using their information and samples in future scientific research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lyu, X., Zhang, D., Pan, H. et al. Machine learning models for differential diagnosis of Cushing’s disease and ectopic ACTH secretion syndrome. Endocrine 80, 639–646 (2023). https://doi.org/10.1007/s12020-023-03341-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-023-03341-7