Abstract
Background
Most pituitary adenomas (PAs) are considered to have a soft tumor consistency. However, there is a non-negligible percentage (5–13%) of tumors presenting or exhibiting a fibrous consistency that would entail a more difficult and complicated surgical excision with higher surgical morbidity and mortality rates.
Purpose
To analyze the clinical consequences of PA tumor consistency on the surgical outcomes in patients undergoing endonasal endoscopic transsphenoidal (EET) pituitary surgery.
Methods
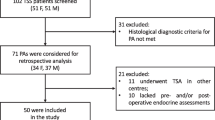
An ambispective study of patients with PAs operated on through an EET approach in two Spanish tertiary hospitals over the last 12 years. A total of 226 consecutive interventions were carried out in the Neurosurgery Departments of the Hospital Universitario Ramón y Cajal (HURC) and the Hospital Universitario Puerta del Sur by the same neurosurgeon. PAs were grouped into soft (n = 150) and fibrous (n = 76). All patients underwent hormonal and magnetic resonance imaging (MRI) studies before and after surgery. In addition, neurosurgical complications were recorded in each patient.
Results
Fibrous adenomas were independently associated with lower resection rates compared to soft adenomas (fibrous gross total resection [GTR] rate 48.7% vs. 76.3%, p < 0.001), even in those adenomas without invasion of the cavernous sinus (Knosp grades 0, I, and II). There were more intraoperative cerebrospinal fluid (CSF) leaks in patients with fibrous PAs. Moreover, fibrous PAs showed higher rates of postoperative hypopituitarism, permanent diabetes insipidus (DI) and postoperative treatments (hormonal treatment and radiotherapy). The excision of a fibrous PA required a longer surgical time (22.5 min more than soft PAs, p = 0.014), regardless of other factors.
Conclusion
The consistency of the PAs significantly conditions both the results of surgery (lower resections rates), complications (higher incidence of postoperative hypopituitarism, permanent DI), and the prognosis (higher incidence of postoperative treatments) of the patient undergoing EET.



Similar content being viewed by others
References
Q.T. Ostrom et al. CBTRUS Statistical Report: primary brain and other central nervous system tumors diagnosed in the United States in 2012–2016. Neuro. Oncol. 21(5), v1–v100 (2019)
M. Cappelletti, A.G. Ruggeri, L. Spizzichino, A. D’Amico, E. D’avella, R. Delfini, Fibrous pituitary macroadenomas: predictive role of preoperative radiologic investigations for proper surgical planning in a cohort of 66 patients. World Neurosurg. 121(Jan), e449–e457 (2019)
L. Yiping, X. Ji, G. Daoying, Y. Bo, Prediction of the consistency of pituitary adenoma: a comparative study on diffusion-weighted imaging and pathological results. J. Neuroradiol. 43(3 Jun), 186–194 (2016)
J.W. Rutland et al. Analysis of 7-tesla diffusion-weighted imaging in the prediction of pituitary macroadenoma consistency. J. Neurosurg. 134(3), 771–779 (2021)
M.E. Molitch, Diagnosis and treatment of pituitary adenomas: a review. JAMA - J. Am. Med. Assoc. 317(5), 516–524 (2017)
S. Schur, O. Lasry, M.A. Tewfik & S. Di Maio, Assessing the association of tumor consistency and gland manipulation on hormonal outcomes and delayed hyponatremia in pituitary macroadenoma surgery. Interdiscip. Neurosurg. Adv. Tech. Case Manag., 20, no. November, 2020
M.J. Rutkowski et al. Development and clinical validation of a grading system for pituitary adenoma consistency. J. Neurosurg. 134(6), 1800–1807 (2021)
E. Knosp, E. Steiner, K. Kitz, C. Matula, Pituitary adenomas with invasion of the cavernous sinus space. Neurosurgery 33(4 Oct), 610–618 (1993)
J.C. Fernandez-Miranda et al. Cavernous sinus compartments from the endoscopic endonasal approach: anatomical considerations and surgical relevance to adenoma surgery. J. Neurosurg. 129(2), 430–441 (2018)
A.E. Ortiz-Flores et al. Role of sampling times and serum cortisol cut-off concentrations on the routine assessment of adrenal function using the standard cosyntropin test in an academic hospital from Spain: a retrospective chart review. BMJ Open 8(5), 1–10 (2018)
L. Katznelson et al. Acromegaly: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 99(11), 3933–3951 (2014)
L.K. Nieman et al. The diagnosis of Cushing’s syndrome: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 93(5), 1526–1540 (2008)
P. Beck-Peccoz, A. Lania, A. Beckers, K. Chatterjee, J.-L. Wemeau, 2013 European thyroid association guidelines for the diagnosis and treatment of thyrotropin-secreting pituitary tumors. Eur. Thyroid J. 2(2), 76–82 (2013)
S. Melmed et al. Diagnosis and treatment of hyperprolactinemia: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 96(2), 273–288 (2011)
M. Araujo-Castro et al. Postoperative management of patients with pituitary tumors submitted to pituitary surgery. Experience of a Spanish Pituitary Tumor Center of Excellence. Endocrine 69(1), 5–17 (2020)
A.L. Pappy, A. Savinkina, C. Bicknese, S. Neill, N.M. Oyesiku, A.G. Ioachimescu, Predictive modeling for pituitary adenomas: single center experience in 501 consecutive patients. Pituitary 22(5), 520–531 (2019)
A.O. Asemota, M. Ishii, H. Brem, G.L. Gallia, Comparison of complications, trends, and costs in endoscopic vs microscopic pituitary surgery: analysis from a US health claims database. Clin. Neurosurg. 81(3), 458–471 (2017)
L. Lv et al. Clinical and pathologic characteristics predicted the postoperative recurrence and progression of pituitary adenoma: a retrospective study with 10 years follow-up. World Neurosurg. 118(Oct), e428–e435 (2018)
S. Dhandapani, H. Singh, H.M. Negm, S. Cohen, V.K. Anand, T.H. Schwartz, Cavernous sinus invasion in pituitary adenomas: systematic review and pooled data meta-analysis of radiologic criteria and comparison of endoscopic and microscopic surgery. World Neurosurg. 96, 36–46 (2016)
M.A. Mooney et al. Proposal and validation of a simple grading scale (TRANSSPHER Grade) for predicting gross total resection of nonfunctioning pituitary macroadenomas after transsphenoidal surgery. Oper. Neurosurg. 17(5), 460–469 (2019)
T. Ouyang et al. Outcomes and Complications of Aggressive Resection Strategy for Pituitary Adenomas in Knosp Grade 4 With Transsphenoidal Endoscopy. Front. Oncol. 11, 1–12 (2021)
A. Acitores Cancela, V. Rodríguez Berrocal, H. Pian, J.S. Martínez San Millán, J.J. Díez, P. Iglesias,, Clinical relevance of tumor consistency in pituitary adenoma. Hormones 20(3), 463–473 (2021).
X. Y. Chen et al. Relationship between pituitary adenoma consistency and extent of resection based on tumor/cerebellar peduncle T2-weighted imaging intensity (TCTI) ratio of the point on preoperative magnetic resonance imaging (MRI) corresponding to the residual point on Postoperative MRI. Med. Sci. Monit. 26, 1–8 (2020)
W.A. Azab et al. Endoscopic endonasal excision of large and giant pituitary adenomas: radiological and intraoperative correlates of the extent of resection. World Neurosurg. 126, e793–e802 (2019)
A.K. Thotakura, M.R. Patibandla, M.K. Panigrahi, A. Mahadevan, Is it really possible to predict the consistency of a pituitary adenoma preoperatively? Neurochirurgie 63, 453–457 (2017)
A. Micko et al. Challenging Knosp high-grade pituitary adenomas. J. Neurosurg. 132, 1739–1746 (2020).
S. Yamada et al. Clinicopathological characteristics and therapeutic outcomes in thyrotropin-secreting pituitary adenomas: a single-center study of 90 cases. J. Neurosurg. 121(6 Dec), 1462–1473 (2014)
J.A. Gondim, J.P.C. Almeida, L.A.F. Albuquerque, E.F. Gomes, M. Schops, Giant pituitary adenomas: surgical outcomes of 50 cases operated on by the endonasal endoscopic approach. World Neurosurg. 82(1–2), e281–e290 (2014)
A.S. Little et al. Evaluation of surgical resection goal and its relationship to extent of resection and patient outcomes in a multicenter prospective study of patients with surgically treated, nonfunctioning pituitary adenomas: a case series. Oper. Neurosurg. 18(1), 26–33 (2020)
M. Araujo-Castro et al. Predictive model of surgical remission in acromegaly: age, presurgical GH levels and Knosp grade as the best predictors of surgical remission. J. Endocrinol. Invest. 44(1), 183–193 (2021)
R.D. Almutairi et al. Gross total resection of pituitary adenomas after endoscopic vs. microscopic transsphenoidal surgery: a meta-analysis. Acta Neurochir. (Wien.) 160(5 May), 1005–1021 (2018)
X. Bao et al. Extended transsphenoidal approach for pituitary adenomas invading the cavernous sinus using multiple complementary techniques. Pituitary 19(1), 1–10 (2016)
G. Alzhrani, W. Sivakumar, M.S. Park, P. Taussky, W.T. Couldwell, Delayed complications after transsphenoidal surgery for pituitary adenomas. World Neurosurg. 109(Jan), 233–241 (2018)
T.H. Schwartz, A role for centers of excellence in transsphenoidal surgery. World Neurosurg. 80(3–4), 270–271 (2013)
M.S. Agam, M.A. Wedemeyer, B. Wrobel, M.H. Weiss, J.D. Carmichael, G. Zada, Complications associated with microscopic and endoscopic transsphenoidal pituitary surgery: experience of 1153 consecutive cases treated at a single tertiary care pituitary center. J. Neurosurg. 130(5), 1576–1583 (2019)
S.H. Kim et al. Immediate postoperative measurement of thyroid-stimulating hormone as an early predictor of remission in thyroid-stimulating hormone–secreting pituitary adenomas. J. Neurosurg., pp. 1–7, 2020
D.J. Lobatto et al. Preoperative risk factors for postoperative complications in endoscopic pituitary surgery: a systematic review. Pituitary 21(1), 84–97 (2018)
N. Fatemi et al. Pituitary hormonal loss and recovery after transsphenoidal adenoma removal. Neurosurgery 63(4), 709–718 (2008)
A. Campero, J.F. Villalonga, A. Basso, Anatomical risk factors for intraoperative cerebrospinal fluid leaks during transsphenoidal surgery for pituitary adenomas. World Neurosurg. 124, e346–e355 (2019)
M. Araujo-Castro, F. Mariño-Sánchez, A. Acitores Cancela, A. García Fernández, S. García Duque, V. Rodríguez Berrocal, Is it possible to predict the development of diabetes insipidus after pituitary surgery? Study of 241 endoscopic transsphenoidal pituitary surgeries. J. Endocrinol. Invest. 44, 1457–1464 (2021)
W.T. Burke, D.J. Cote, D.L. Penn, S. Iuliano, K. McMillen, E.R. Laws, Diabetes Insipidus after endoscopic transsphenoidal surgery. Neurosurgery 87(5), 949–955 (2020)
P. Nayak, A.S. Montaser, J. Hu, D.M. Prevedello, L.S. Kirschner, L. Ghalib, Predictors of postoperative diabetes insipidus following endoscopic resection of pituitary adenomas. J. Endocr. Soc. 2(9), 1010–1019 (2018)
E. Uvelius, P. Siesjö, 3-D endoscopy in surgery of pituitary adenomas, prospective evaluation of patient gain using basic outcome parameters. J. Clin. Neurosci. 76, 166–170 (2020)
P. Leach, A.H. Abou-Zeid, T. Kearney, J. Davis, P.J. Trainer, K.K. Gnanalingham, Endoscopic transsphenoidal pituitary surgery: evidence of an operative learning curve. Neurosurgery 67(5), 1205–1212 (2010)
H. Cheng et al. Prolonged operative duration is associated with complications: a systematic review and meta-analysis. J. Surg. Res. 229, 134–144 (2018)
J. Cyprich et al. Comparative preoperative characteristics and postoperative outcomes at a private versus a safety-net hospital following endoscopic endonasal transsphenoidal resection of pituitary adenomas. J. Neurosurg 134, 742–749 (2021)
A. Thotakura, M. Patibandla, M. Panigrahi, G. Addagada, Predictors of visual outcome with transsphenoidal excision of pituitary adenomas. Asian J. Neurosurg. 12(1), 1 (2017)
R.W. Ho, H.M. Huang, J.T. Ho, The influence of pituitary adenoma size on vision and visual outcomes after trans-sphenoidal adenectomy: a report of 78 cases. J. Korean Neurosurg. Soc. 57(1), 23–31 (2015)
C. Thomé, D. Zevgaridis, Delayed visual deterioration after pituitary surgery - A review introducing the concept of vascular compression of the optic pathways. Acta Neurochir. (Wien.) 146(10), 1131–1135 (2004)
H. Do et al. Extent of resection, visual, and endocrinologic outcomes for endoscopic endonasal surgery for recurrent pituitary adenomas. World Neurosurg. 102, 35–41 (2017)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
The studies involving human participants were reviewed and approved by the Ethical Committee of the Ramón y Cajal Hospital.
Informed consent
The patients/participants provided their written informed consent to participate in this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Acitores Cancela, A., Rodríguez Berrocal, V., Pian Arias, H. et al. Effect of pituitary adenoma consistency on surgical outcomes in patients undergoing endonasal endoscopic transsphenoidal surgery. Endocrine 78, 559–569 (2022). https://doi.org/10.1007/s12020-022-03161-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-022-03161-1