Abstract
Purpose
The aim of the study was to evaluate indexes of insulin resistance and cardiometabolic risk in a large population of workers with overweight or obesity, in order to identify a possible efficient, cheap and simple strategy to apply in workers’ health surveillance.
Methods
The evaluation of IR and cardiometabolic risk indexes (HOMA, QUICKI, Ty/HDLC, TyG, insuTAG, Castelli risk indexes 1 and 2, non-HDLC, TRL-C, AIP, and VAI) was performed in a population of 1195 working-age subjects with overweight or obesity (322 males, mean age 49 ± 11 years).
Results
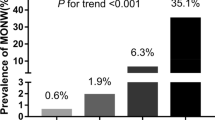
The prevalence of IR and cardiometabolic risk was higher among males for all indexes. Aging, waist circumference, BMI, blood pressure, glucose, CRP, fibrinogen and uric acid were correlated more frequently with IR/cardiometabolic indexes in women, homocysteine in men. The percentage of the workers identified as insulin resistant (IR+) or at higher cardiometabolic risk greatly vary according to the different index used.
Conclusion
With a small group of biomarkers and anthropometric measures (fasting glucose and insulin, lipid profile, BMI and waist circumference) is possible to calculate a number of IR/cardiometabolic indexes, which, likely reflecting different pathophysiological aspects also related to gender, might help in a personalized evaluation of IR and cardiometabolic risk.

Graphical abstract

Similar content being viewed by others
References
R.H. Eckel, S.E. Kahn, E. Ferrannini, A.B. Goldfine, D.M. Nathan, M.W. Schwartz, R.J., S.R. Smith, Obesity and type 2 diabetes: what Can be unified and what needs to be individualized? Diabetes Care 34 (2011). https://doi.org/10.2337/dc11-0447.
J.P. Moriarty, M.E. Branda, K.D. Olsen, N.D. Shah, B.J. Borah, A.E. Wagie, J.S. Egginton, J.M. Naessens, The effects of incremental costs of smoking and obesity on health care costs among adults: a 7-year longitudinal study. J. Occup. Environ. Med. 54 (2012). https://doi.org/10.1097/JOM.0b013e318246f1f4.
M.S. Greenfield, L. Doberne, F. Kraemer, T. Tobey, G. Reaven. Assessment of insulin resistance with the insulin suppression test and the euglycemic clamp. Diabetes. 30 (1981). https://doi.org/10.2337/diab.30.5.387.
R.A. DeFronzo, J.D. Tobin, R. Andres, Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am. J. Physiol. Endocrinol. Metab. Gastrointest. Physiol. 6 (1979). https://doi.org/10.1152/ajpendo.1979.237.3.e214.
D.R. Matthews, J.P. Hosker, A.S. Rudenski, B.A. Naylor, D.F. Treacher, R.C. Turner. Homeostasis model assessment: insulin resis tance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28 (1985). https://doi.org/10.1007/BF00280883.
A. Katz, S.S. Nambi, K. Mather, A.D. Baron, D.A. Follmann, G. Sullivan, M.J. Quon, Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J. Clin. Endocrinol. Metab. 85 (2000). https://doi.org/10.1210/jcem.85.7.6661.
M. Gutt, C.L. Davis, S.B. Spitzer, M.M. Llabre, M. Kumar, E.M. Czarnecki, N. Schneiderman, J.S. Skyler, J.B. Marks, Validation of the insulin sensitivity index (ISI0,120): Comparison with other measures. Diabetes Res. Clin. Pract. 47 (2000). https://doi.org/10.1016/S0168-8227(99)00116-3.
F. Tosi, E. Bonora, P. Moghetti, Insulin resistance in a large cohort of women with polycystic ovary syndrome: a comparison between euglycaemic-hyperinsulinaemic clamp and surrogate indexes. Hum. Reprod. 32 (2017) https://doi.org/10.1093/humrep/dex308.
T. McLaughlin, G. Reaven, F. Abbasi, C. Lamendola, M. Saad, D. Waters, J. Simon, R.M. Krauss. Is there a simple way to identify insulin-resistant individuals at increased risk of cardiovascular disease? Am. J. Cardiol. 96 (2005). https://doi.org/10.1016/j.amjcard.2005.03.085.
R. Quispe, R.J. Manalac, K.F. Faridi, M.J. Blaha, P.P. Toth, K.R. Kulkarni, K. Nasir, S.S. Virani, M. Banach, R.S. Blumenthal et al. Relationship of the triglyceride to high-density lipoprotein cholesterol (TG/HDL-C) ratio to the remainder of the lipid profile: The Very Large Database of Lipids-4 (VLDL-4) study. Atherosclerosis 242 (2015). https://doi.org/10.1016/j.atherosclerosis.2015.06.057.
S.H. Lee, H.S. Kwon, Y.M. Park, H.S. Ha, S.H. Jeong, H.K. Yang, J.H. Lee, H.W. Yim, M. Il Kang; W.C. Lee et al. Predicting the development of diabetes using the product of triglycerides and glucose: the chungju metabolic disease cohort (CMC) study. PLoS ONE 9 (2014). https://doi.org/10.1371/journal.pone.0090430.
R.N. Thota, K.A. Abbott, J.J.A. Ferguson, M. Veysey, M. Lucock, S. Niblett, K. King, M.L. Garg, InsuTAG: a novel physiologically relevant predictor for insulin resistance and metabolic syndrome. Sci. Rep. 7 (2017). https://doi.org/10.1038/s41598-017-15460-z.
W.P. Castelli, R.D. Abbott, P.M. McNamara, Summary estimates of cholesterol used to predict coronary heart disease. Circulation 67 (1983). https://doi.org/10.1161/01.CIR.67.4.730.
X. Su, Y. Kong, D. Peng, Evidence for changing lipid management strategy to focus on non-high density lipoprotein cholesterol. Lipids Health Dis. 18 (2019). https://doi.org/10.1186/s12944-019-1080-x.
M. Dobiásová AIP--atherogenic index of plasma as a significant predictor of cardiovascular risk: from research to practice. Vnitr Lek. 52 (2006).
M.C. Amato, C. Giordano, Visceral adiposity index: an indicator of adipose tissue dysfunction. Int. J. Endocrinol. (2014). https://doi.org/10.1155/2014/730827.
L. Vigna, C. Vassalle, A.S. Tirelli, F. Gori, L. Tomaino, L. Sabatino, F. Bamonti, Gender-related association between uric acid, homocysteine, γ-glutamyltransferase, inflammatory biomarkers and metabolic syndrome in subjects affected by obesity. Biomark. Med. 11 (2017). https://doi.org/10.2217/bmm-2017-0072.
A. Borai, C. Livingstone, I. Kaddam, G. Ferns. Selection of the appropriate method for the assessment of insulin resistance. BMC Med. Res. Methodol. 11 (2011). https://doi.org/10.1186/1471-2288-11-158.
R. Muniyappa, S. Lee, H. Chen, M.J. Quon, Current approaches for assessing insulin sensitivity and resistance in vivo: Advantages, limitations, and appropriate usage. Am. J. Physiol. - Endocrinol. Metab. 294 (2008). https://doi.org/10.1152/ajpendo.00645.2007.
L.E. Simental-Mendía, M. Rodríguez-Morán, F. Guerrero-Romero, The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab. Syndr. Relat. Disord. 6 (2008). https://doi.org/10.1089/met.2008.0034.
F. Guerrero-Romero, L.E. Simental-Mendía, M. González-Ortiz, E. Martínez-Abundis, M.G. Ramos-Zavala, S.O. Hernández-González, O. Jacques-Camarena, M. Rodríguez-Morán, The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic-hyperinsulinemic clamp. J. Clin. Endocrinol. Metab. 95 (2010). https://doi.org/10.1210/jc.2010-0288.
F. Lucatello, L. Vigna, M. Carugno, A.S. Tirelli, P.A. Bertazzi, L. Riboldi, Comparison of indexes for assessing insulin resistance for the health surveillance among workers [Confronto tra indici per la valutazione dell’insulino-resistenza nella sorveglianza sanitaria dei lavoratori]. G. Ital. Med. Lav. Ergon. 34 (2012).
N. Ahn, S.E. Baumeister, U. Amann, W. Rathmann, A. Peters, C. Huth, B. Thorand, C. Meisinger, Visceral adiposity index (VAI), lipid accumulation product (LAP), and product of triglycerides and glucose (TyG) to discriminate prediabetes and diabetes. Sci. Rep. 9 (2019). https://doi.org/10.1038/s41598-019-46187-8.
J. Millán, X. Pintó, A. Muñoz, M. Zúñiga, J. Rubiés-Prat, L.F. Pallardo, L. Masana, A. Mangas, A. Hernández-Mijares, P. González-Santos, J.F. Ascaso, J. Pedro-Botet, Lipoprotein ratios: physiological significance and clinical usefulness in cardiovascular prevention. Vasc. Health Risk Manag. 5 (2009). https://doi.org/10.2147/vhrm.s6269.
W. Masson, M. Lobo, D. Siniawski, G. Molinero, M. Huerín, J.P. Nogueira, Impact of lipid-lowering therapy on mortality according to the baseline non-HDL cholesterol level: a meta-analysis. High Blood Press. Cardiovasc. Prev. 26 (2019). https://doi.org/10.1007/s40292-019-00330-8.
A. Varbo, M. Benn, A. Tybjærg-Hansen, B.G. Nordestgaard, Elevated remnant cholesterol causes both low-grade inflammation and ischemic heart disease, whereas elevated low-density lipoprotein cholesterol causes ischemic heart disease without inflammation. Circulation 128 (2013). https://doi.org/10.1161/CIRCULATIONAHA.113.003008.
O. Castañer, X. Pintó, I. Subirana, A.J. Amor, E. Ros, Á. Hernáez, M.Á. Martínez-González, D. Corella, J. Salas-Salvadó, R. Estruch et al. Remnant cholesterol, not LDL cholesterol, is associated with incident cardiovascular disease. J. Am. Coll. Cardiol. 76 (2020). https://doi.org/10.1016/j.jacc.2020.10.008.
M. Dobiášová, J. Frohlich, The plasma parameter log (TG/HDL-C) as an atherogenic index: Correlation with lipoprotein particle size and esterification rate inapob-lipoprotein-depleted plasma (FERHDL). Clin. Biochem. 34 (2001). https://doi.org/10.1016/S0009-9120(01)00263-6.
E. Al Shawaf, E. Al-Ozairi, F. Al-Asfar, A. Mohammad, S. Al-Beloushi, S. Devarajan, F. Al-Mulla, J. Abubaker, H. Arefanian, Atherogenic index of plasma (AIP) a tool to assess changes in cardiovascular disease risk post laparoscopic sleeve gastrectomy. J. Diabetes Res. 2020 (2020). https://doi.org/10.1155/2020/2091341.
H. King, M. Rewers, Global estimates for prevalence of diabetes mellitus and impaired glucose tolerance in adults. Diabetes Care 16 (1993). https://doi.org/10.2337/diacare.16.1.157.
V. Regitz-Zagrosek, E. Lehmkuhl, M.O. Weickert, Gender differences in the metabolic syndrome and their role for cardiovascular disease. Clin. Res. Cardiol. 95 (2006) https://doi.org/10.1007/s00392-006-0377-8.
A.G. Huebschmann, R.R. Huxley, W.M. Kohrt, P. Zeitler, J.G. Regensteiner, J.E.B. Reusch, Sex differences in the burden of type 2 diabetes and cardiovascular risk across the life course. Diabetologia 62 (2019). https://doi.org/10.1007/s00125-019-4939-5.
J. Logue, J. J. Walker, H.M. Colhoun, G.P. Leese, R.S. Lindsay, J.A. McKnight, A.D. Morris, D.W. Pearson, J.R. Petrie, S. Philip et al. Do men develop type 2 diabetes at lower body mass indices than women? Diabetologia 54 (2011). https://doi.org/10.1007/s00125-011-2313-3.
S. Paul, G. Thomas, A. Majeed, K. Khunti, K. Klein, Women develop type 2 diabetes at a higher body mass index than men. Diabetologia 55, 1556–7 (2012).
N. Sattar, Gender aspects in type 2 diabetes mellitus and cardiometabolic risk. Best Pract. Res. Clin. Endocrinol. Metab. 27 (2013). https://doi.org/10.1007/s00125-012-2496-2.
M.K. Breyer, A. Ofenheimer, J. Altziebler, S. Hartl, O.C. Burghuber, M. Studnicka, D. Purin, C. Heinzle, H. Drexel, F.M.E. Franssen et al. Marked differences in prediabetes- and diabetes-associated comorbidities between men and women—Epidemiological results from a general population-based cohort aged 6-80 years—The LEAD (Lung, hEart, sociAl, boDy) study. Eur. J. Clin. Investig. 50 (2020). https://doi.org/10.1111/eci.13207.
A. Al-Salameh, P. Chanson, S. Bucher, V. Ringa L. Becquemont. Cardiovascular disease in type 2 diabetes: a review of sex-related differences in predisposition and prevention. Mayo Clin. Proc. 94(2) (2019). https://doi.org/10.1016/j.mayocp.2018.08.007.
V. Grossmannm, V.H. Schmitt, T. Zeller, M. Panova-Noeva, A. Schulz, D. Laubert-Reh, C. Juenger, R.B. Schnabel, T.G.J. Abt, R. Laskowski, J. Wiltink, E. Schulz, S. Blankenberg, K.J. Lackner, T. Münzel, PWild, P.S. Profile of the immune and inflammatory response in individuals with prediabetes and type 2 diabetes. Diabetes Care 38 (2015). https://doi.org/10.2337/dc14-3008.
J. Dierkes, A. Jeckel, A. Ambrosch, S. Westphal, C. Luley, H. Boeing, Factors explaining the difference of total homocysteine between men and women in the European investigation into cancer and nutrition potsdam study. Metabolism. 50 (2001) https://doi.org/10.1053/meta.2001.23286.
S. Pitla, B. Nagalla, Gender-related differences in the relationship between plasma homocysteine, anthropometric and conventional biochemical coronary heart disease risk factors in middle-aged indians. Ann. Nutr. Metab. 54 (2009). https://doi.org/10.1159/000199452.
B. Vogel, M. Acevedo, Y. Appelman, C.N. Bairey Merz, A. Chieffo, G.A. Figtree, M. Guerrero, V. Kunadian, C.S.P. Lam, A.H.E.M. Maas, A.S. Mihailidou, A. Olszanecka, J.E. Poole, C. Saldarriaga, J. Saw, J., Zühlke, R. Mehran, The Lancet women and cardiovascular disease Commission: reducing the global burden by 2030. Lancet. 19 (2021). https://doi.org/10.1016/S0140-6736(21)00684-X.
C. Vassalle, T. Simoncini, P. Chedraui, F.R. Pérez-López, Why sex matters: the biological mechanisms of cardiovascular disease. Gynecol. Endocrinol. 28(9), 746–751 (2012). https://doi.org/10.3109/09513590.2011.652720.
C. Vassalle, R. Sciarrino, S. Bianchi, D. Battaglia, A. Mercuri, S. Maffei, Sex-related differences in association of oxidative stress status with coronary artery disease. Fertil. Steril. 97(2), 414–419 (2012). https://doi.org/10.1016/j.fertnstert.2011.11.045.
M. Amiri, I. Karabegović, A.C. van Westing, A.J.C.F. Verkaar, S. Beigrezaei, M. Lara, W.M. Bramer, T. Voortman, Whole-diet interventions and cardiovascular risk factors in postmenopausal women: a systematic review of controlled clinical trials. Maturitas 155, 40–53 (2022). https://doi.org/10.1016/j.maturitas.2021.10.001.
S. Sciomer, F. Moscucci, S. Maffei, S. Gallina, A.V. Mattioli, Prevention of cardiovascular risk factors in women: The lifestyle paradox and stereotypes we need to defeat. Eur. J. Prev. Cardiol. 26(6), 609–610 (2019). https://doi.org/10.1177/2047487318810560.
M. D’Adamo, L. Perego, M. Cardellini, M.A. Marini, S. Frontoni, F. Andreozzi, A. Sciacqua, D. Lauro, P. Sbraccia, M. Federici et al. The -866A/A genotype in the promoter of the human uncoupling protein 2 gene is associated with insulin resistance and increased risk of type 2 diabetes. Diabetes 53 (2004) https://doi.org/10.2337/diabetes.53.7.1905.
C. Capurso, A. Capurso. From excess adiposity to insulin resistance: the role of free fatty acids. Vascul. Pharmacol. 57 (2012). https://doi.org/10.1016/j.vph.2012.05.003.
G. Riccardi, R. Giacco, A.A. Rivellese, Dietary fat, insulin sensitivity and the metabolic syndrome. Clin. Nutr. 23 (2004). https://doi.org/10.1016/j.clnu.2004.02.006.
M.S. Zhou, I.H. Schulman, Q. Zeng, Link between the renin-angiotensin system and insulin resistance: Implications for cardiovascular disease. Vasc. Med. 17 (2012). https://doi.org/10.1177/1358863X12450094.
ME. Lindholm, F. Marabita, D. Gomez-Cabrero, H. Rundqvist, TJ. Ekström, J. Tegnér, CJ. Sundberg, An integrative analysis reveals coordinated reprogramming of the epigenome and the transcriptome in human skeletal muscle after training. Epigenetics 9, 1557–69 (2014).
S. Placzkowska, L. Pawlik-Sobecka, I. Kokot, A. Piwowar, Indirect insulin resistance detection: current clinical trends and laboratory limitations. Biomed. Pap. 163 (2019). https://doi.org/10.5507/bp.2019.021.
Acknowledgements
Center of Obesity and Work, Occupational Health Unit of Clinica del Lavoro “L. Devoto”, Fondazione IRCCS Ca’ Granda, Ospedale Maggiore Policlinico, Milan (Italy).
Author contributions
C.V., L.V., S.A.T.: study conceptualization; S.D.P., L.T., S.A.T., F.B., S.T., L.V., M.G.: data acquisition, and database assessment; C.V., M.G.: data analysis; C.V., L.V.: drafting of the manuscript. All authors contributed to the manuscript intellectual content and gave approval to the final version.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
The study was conducted according to the Good Clinical Practice guidelines and approved by Human Ethic Committee of Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico (Registration number: 852).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vigna, L., Tirelli, A.S., Gaggini, M. et al. Insulin resistance and cardiometabolic indexes: comparison of concordance in working-age subjects with overweight and obesity. Endocrine 77, 231–241 (2022). https://doi.org/10.1007/s12020-022-03087-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-022-03087-8