Abstract
Objectives
We adopted the machine-learning algorithms and deep-learning sequential model to determine and optimize most important factors for overweight and obesity in Chinese preschool-aged children.
Methods
This is a cross-sectional survey conducted in 2020 at Beijing and Tangshan. Using a stratified cluster random sampling strategy, children aged 3-6 years were enrolled. Data were analyzed using the PyCharm and Python.
Results
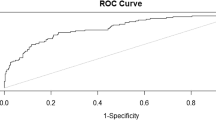
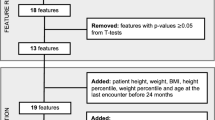
A total of 9478 children were eligible for inclusion, including 1250 children with overweight or obesity. All children were randomly divided into the training group and testing group at a 6:4 ratio. After comparison, support vector machine (SVM) outperformed the other algorithms (accuracy: 0.9457), followed by gradient boosting machine (GBM) (accuracy: 0.9454). As reflected by other 4 performance indexes, GBM had the highest F1 score (0.7748), followed by SVM with F1 score at 0.7731. After importance ranking, the top 5 factors seemed sufficient to obtain descent performance under GBM algorithm, including age, eating speed, number of relatives with obesity, sweet drinking, and paternal education. The performance of the top 5 factors was reinforced by the deep-learning sequential model.
Conclusions
We have identified 5 important factors that can be fed to GBM algorithm to better differentiate children with overweight or obesity from the general children, with decent prediction performance.




Similar content being viewed by others
References
A. Pandita, D. Sharma, D. Pandita et al. Childhood obesity: prevention is better than cure. Diabetes Metab. Syndr. Obes. 9, 83–89 (2016)
NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 390, 2627–2642 (2017)
World Health Organization. Obesity and Overweight. World Health Organization (WHO) http://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight (2018). Accessed 28 May 2018
T. Lobstein, R. Jackson-Leach, M.L. Moodie et al. Child and adolescent obesity: part of a bigger picture. Lancet. 385, 2510–2520 (2015)
P. Jia, H. Xue, J. Zhang, Y. Wang. Time trend and demographic and geographic disparities in childhood obesity prevalence in China-evidence from twenty years of longitudinal data. Int. J. Environ. Res. Public Health. 14, 369 (2017)
Y. Dong, C. Jan, Y. Ma et al. Economic development and the nutritional status of Chinese school-aged children and adolescents from 1995 to 2014: an analysis of five successive national surveys. Lancet Diabetes Endocrinol. 7, 288–299 (2019)
A. Smego, J.G. Woo, J. Klein et al. High body mass index in infancy may predict severe obesity in early childhood. J. Pediatr. 183, 87–93 (2017)
S.G. Hassink. Early child care and education: a key component of obesity prevention in infancy. Pediatrics. 140, e20172846 (2017)
S.E. Benjamin Neelon, T. Østbye, D. Hales et al. Preventing childhood obesity in early care and education settings: lessons from two intervention studies. Child Care Health Dev. 42, 351–358 (2016)
J. Yan, L. Liu, Y. Zhu et al. The association between breastfeeding and childhood obesity: a meta-analysis. BMC Public Health 14, 1267 (2014)
C. Padez, I. Mourao, P. Moreira, V. Rosado, Long sleep duration and childhood overweight/obesity and body fat. Am. J. Hum. Biol. 21, 371–376 (2009)
K.E. Hunter, B.J. Johnson, L. Askie et al. Transforming Obesity Prevention for CHILDren (TOPCHILD) Collaboration: protocol for a systematic review with individual participant data meta-analysis of behavioural interventions for the prevention of early childhood obesity. BMJ Open 12, e048166 (2022)
N. Liu, H. Li, Z. Guo et al. Prevalence and factors associated with overweight or obesity among 2- to 6-year-old children in Hunan, China: a cross-sectional study. Public Health Nutr. 1–32 (2022)
S.J. Russell, S. Hope, H. Croker et al. Modeling the impact of calorie-reduction interventions on population prevalence and inequalities in childhood obesity in the Southampton Women’s Survey. Obes. Sci. Pract. 7, 545–554 (2021)
S. Liu, J. Zhang, J. Ma et al. Synergistic interaction between bedtime and eating speed in predicting overweight and obesity in Chinese preschool-aged children. Aging (Albany NY) 11, 2127–2137 (2019)
B. Zhou, Y. Yuan, K. Wang et al. Interaction effects of significant risk factors on overweight or obesity among 7222 preschool-aged children from Beijing. Aging (Albany NY) 12, 15462–15477 (2020)
M.N. LeCroy, R.S. Kim, J. Stevens et al. Identifying key determinants of childhood obesity: a narrative review of machine learning studies. Child Obes. 17, 153–159 (2021)
P. Doupe, J. Faghmous, S. Basu, Machine learning for health services researchers. Value Health 22, 808–815 (2019)
C. Colmenarejo. Machine learning models to predict childhood and adolescent obesity: a review. Nutrients 12, 2466 (2020)
S.M. Li, M.Y. Ren, J. Gan et al. Machine learning to determine risk factors for myopia progression in primary school children: the Anyang childhood eye study. Ophthalmol. Ther. 11, 573–585 (2022)
F. Ramos-Gomez, M. Marcus, C.A. Maida et al. Using a machine learning algorithm to predict the likelihood of presence of dental caries among children aged 2 to 7. Dent. J. (Basel) 9, 141 (2021)
U.M. Haque, E. Kabir, R. Khanam, Detection of child depression using machine learning methods. PLoS One 16, e0261131 (2021)
Q. Wang, M. Yang, X. Deng et al. Explorations on risk profiles for overweight and obesity in 9501 preschool-aged children. Obes. Res. Clin. Pract. 16, 106–114 (2022)
M. Yang, X. Deng, S. Wang et al. Risk factors for allergic diseases: a cross-sectional survey of 9,501 Chinese preschool-aged children. Transl. Pediatr. 10, 1989–2005 (2021)
M. Yang, X. Deng, S. Wang et al. Identification and characterization of factors associated with short stature and pre-shortness in Chinese preschool-aged children. Endocr. Connect 10, 607–619 (2021)
The Coordinating Team in the Department of Nutrition for Health and Development of the World Health Organization. WHO Child Growth Standards. (World Health Organization (ISBN 92 4 154693 X), 2006) p. 260–295
World Health Organization: Child growth standards-BMI-for-age. https://www.who.int/childgrowth/standards/bmi_for_age/en/. Accessed 11 Nov 2019
M. de Onis, T. Lobstein, Defining obesity risk status in the general childhood population: which cut-offs should we use? Int. J. Pediatr. Obes. 5, 458–460 (2010)
P. González-Muniesa, M.A. Mártinez-González, F.B. Hu et al. Obesity. Nat. Rev. Dis. Primers 3, 17034 (2017)
K.W. DeGregory, P. Kuiper, T. DeSilvio et al. A review of machine learning in obesity. Obes. Rev. 19, 668–685 (2018)
A. Chatterjee, M.W. Gerdes, S.G. Martinez. Identification of risk factors associated with obesity and overweight-a machine learning overview. Sensors (Basel) 20, 2737 (2020)
A. Qasim, M. Turcotte, R.J. de Souza et al. On the origin of obesity: identifying the biological, environmental and cultural drivers of genetic risk among human populations. Obes. Rev. 19, 121–149 (2018)
É.M. Butler, J.G.B. Derraik, R.W. Taylor, W.S. Cutfield, Childhood obesity: how long should we wait to predict weight? J. Pediatr. Endocrinol. Metab. 31, 497–501 (2018)
J.O. Robson, S.G. Verstraete, S. Shiboski et al. A risk score for childhood obesity in an urban latino cohort. J. Pediatr. 172, 29–34.e21 (2016)
É.M. Butler, J.G.B. Derraik, R.W. Taylor, W.S. Cutfield, Prediction models for early childhood obesity: applicability and existing issues. Horm. Res. Paediatr. 90, 358–367 (2018)
A. Cortés-Martín, G. Colmenarejo, M.V. Selma, J.C. Espín, Genetic polymorphisms, mediterranean diet and microbiota-associated urolithin metabotypes can predict obesity in childhood-adolescence. Sci. Rep. 10, 7850 (2020)
G.W. Cha, H.J. Moon, Y.C. Kim. Comparison of random forest and gradient boosting machine models for predicting demolition waste based on small datasets and categorical variables. Int. J. Environ. Res. Public Health 18, 8530 (2021)
E.J. Atkinson, T.M. Therneau, L.J. Melton III et al. Assessing fracture risk using gradient boosting machine (GBM) models. J. Bone Miner Res. 27, 1397–1404 (2012)
D.M. Yu, L.H. Ju, L.Y. Zhao et al. [Prevalence and characteristics of overweight and obesity in Chinese children aged 0-5 years]. Zhonghua Liu Xing Bing Xue Za Zhi 39, 710–714 (2018)
M. Lin, L. Pan, L. Tang et al. Association of eating speed and energy intake of main meals with overweight in Chinese pre-school children. Public Health Nutr. 17, 2029–2036 (2014)
Author information
Authors and Affiliations
Contributions
Z.Z. planned and designed the study and directed its implementation. Z.Z. drafted the protocol. Q.W., M.Y., B.P., M.X., and Y.Z. obtained statutory and ethics approvals. Q.W. and M.Y. contributed to data acquisition. Q.W. and W.N. conducted statistical analyses. Q.W., M.Y., B.P., and M.X., did the data preparation and quality control. Q.W. and W.N. wrote the manuscript. All authors read and approved the final manuscript prior to submission.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, Q., Yang, M., Pang, B. et al. Predicting risk of overweight or obesity in Chinese preschool-aged children using artificial intelligence techniques. Endocrine 77, 63–72 (2022). https://doi.org/10.1007/s12020-022-03072-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-022-03072-1