Abstract
Objective
Ovarian neuroendocrine neoplasm is a rare and highly heterogeneous neoplasm. This study is aimed to describe its demographic and clinicopathological features and identify its prognostic factors.
Methods
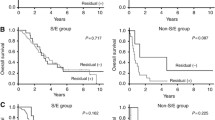
Clinical data of 399 patients diagnosed with ovarian neuroendocrine neoplasms between 2004 and 2016 in the Surveillance, Epidemiology, and End Results (SEER) database were analysed retrospectively. Survival curves were drawn using the Kaplan–Meier method, comparisons among different subgroups were evaluated using log-rank tests, and multivariate Cox regression analyses identified independent prognostic factors.
Results
The five-year survival rates of patients with different histological types (carcinoid tumour, neuroendocrine carcinoma and special type of carcinoid tumour) were 25.5%, 96.1% and 75.0%, respectively (P < 0.001). Multivariate Cox analysis revealed that in carcinoid tumours, advanced FIGO stage was the only predictor. Additionally, no significant difference was observed among stages II, III and IV using the log-rank test. In neuroendocrine carcinoma, an advanced FIGO stage and high-grade differentiation were risk factors, while chemotherapy was a protective factor. Among all ovarian neuroendocrine neoplasms with a known histological differentiation status, no significant difference was observed among different histological types; only high-grade differentiation was an independent risk factor, and chemotherapy was a protective factor.
Conclusions
Patients with neuroendocrine carcinomas and carcinoid tumours of an advanced FIGO stage have a poor prognosis. Poor differentiation of neuroendocrine carcinomas indicates a short survival time, and adjuvant chemotherapy appears to be effective. Histological differentiation of ovarian neuroendocrine neoplasms is the most potent prognostic factor comparing to other known factors. Taken together, ovarian neuroendocrine neoplasms might be better classified as low- or high-grade ones rather than the currently used classification based on histological types in the future.





Similar content being viewed by others
References
R.J. Kurman, M.L. Carcangiu, C.S. Herrington, R.H. Young, World Health Organization Classification of Tumours of the Female Reproductive Organs. International Agency for Research on Cancer (IARC), Lyon (2014).
I.M. Modlin, K.D. Lye, M. Kidd, A 5-decade analysis of 13,715 carcinoid tumors. Cancer 97, 934–959 (2003). https://doi.org/10.1002/cncr.11105
A.J.C. Talerman, o. i. o. & gynecology. Germ cell tumors of the ovary 9, 44–47 (1997)
Y. Zhu et al. Clinicopathologic characteristics and survival outcomes in neuroendocrine carcinoma of the ovary. Int J Gynecol Cancer 30, 207–212 (2020). https://doi.org/10.1136/ijgc-2019-000746
J. Sehouli et al. Neuroendocrine neoplasms of the ovary: A retrospective study of the North Eastern German Society of Gynecologic Oncology (NOGGO). Anticancer research 36, 1003–1009 (2016).
E. Guadagno, G. De Rosa, M. Del Basso De Caro, Neuroendocrine tumours in rare sites: differences in nomenclature and diagnostics-a rare and ubiquitous histotype. J Clin Pathol 69, 563–574 (2016). https://doi.org/10.1136/jclinpath-2015-203551
P. Baker, E. Oliva, R. Young, A. Talerman, R.J.T.A.J.O.S.P. Scully, Ovarian mucinous carcinoids including some with a carcinomatous component: a report of 17 cases. 25, 557–568, https://doi.org/10.1097/00000478-200105000-00001 (2001).
G. Akerstrom, P. Hellman, Surgery on neuroendocrine tumours. Best Pract Res Clin Endocrinol Metab 21, 87–109 (2007). https://doi.org/10.1016/j.beem.2006.12.004
L.R. Zhai et al. Primary ovarian carcinoid: two cases report and review of literature. Medicine (Baltimore) 99, e21109 (2020). https://doi.org/10.1097/MD.0000000000021109
N.S. Reed et al. Gynecologic Cancer InterGroup (GCIG) consensus review for carcinoid tumors of the ovary. Int J Gynecol Cancer 24, S35–S41 (2014). https://doi.org/10.1097/IGC.0000000000000265
J. Gibbs, S. Mei, K. Economos, Y.C. Lee, M.J. Kanis, Clinicopathologic features, incidence, and survival trends of gynecologic neuroendocrine tumors: a SEER database analysis. Am J Obstet Gynecol 221, 53 e51–53 e56 (2019). https://doi.org/10.1016/j.ajog.2019.02.052
X. Yang, J. Chen, R. Dong, Pathological features, clinical presentations and prognostic factors of ovarian large cell neuroendocrine carcinoma: a case report and review of published literature. J Ovarian Res 12, 69 (2019). https://doi.org/10.1186/s13048-019-0543-z
C. Toumpanakis, R.A. Standish, E. Baishnab, M.C. Winslet, M.E. Caplin, Goblet cell carcinoid tumors (adenocarcinoid) of the appendix. Dis Colon Rectum 50, 315–322 (2007). https://doi.org/10.1007/s10350-006-0762-4
M. Kaiho-Sakuma et al. Aggressive neuroendocrine tumor of the ovary with multiple metastases treated with everolimus: A case report. Gynecol Oncol Rep 23, 20–23 (2018). https://doi.org/10.1016/j.gore.2018.01.002
A. Rinke et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors (PROMID): results of long-term survival. Neuroendocrinology 104, 26–32 (2017). https://doi.org/10.1159/000443612
J.K. Ramage et al. Guidelines for the management of gastroenteropancreatic neuroendocrine (including carcinoid) tumours (NETs). Gut 61, 6–32 (2012). https://doi.org/10.1136/gutjnl-2011-300831
S.J.F.Z.P. Oberndorfer, Karzinoide Tumoren des Dunndarms. 1 (1907).
Author contributions
L.Y. is the guarantor of the manuscript. W.H. and L.Y. contributed to conception and design of the study. W.H., L.Q.Y., Y.B., and X.L. contributed to the acquisition and analysis of data. W.H. wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, W., Bao, Y., Luo, X. et al. Neuroendocrine neoplasms of the ovary: an analysis of clinicopathological characteristics and prognosis with a focus on histological grading. Endocrine 77, 188–198 (2022). https://doi.org/10.1007/s12020-022-03067-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-022-03067-y