Abstract
Purpose
Muscle dysfunction is considered a sign of poor prognosis in patients with type 2 diabetes (T2D). Thus, early detection of muscle disorders is particularly important in the T2D population. Free fatty acids (FFAs) are clinical indicators of metabolic diseases and muscle function; hence, we aimed to investigate the association between FFAs and muscle function.
Methods
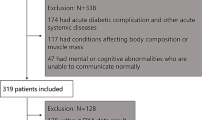
A total of 160 adult subjects with T2D were characterized and analyzed in this study. Muscle mass and function were measured by walking speed, grip strength and height-adjusted appendicular skeletal muscle mass (ASMM). Partial correlation was applied to explore the correlations between FFAs and muscle indicators. Receiver operating characteristic (ROC) curves were utilized to determine the diagnostic value of FFAs in muscle mass and function.
Results
The FFAs levels were negatively correlated with ASMM (r = −0.347, P = 1.0E-05), grip strength (r = −0.313, P = 7.1E-05) and walking speed (r = −0.167, P = 0.039). Notably, the relationships between FFAs levels and ASMM and walking speed remained significant even after adjusting for age, sex, body mass index (BMI), diabetes duration, and hemoglobin A1C (HbA1c). The combination of conventional indicators, including age, BMI, and HbA1c levels, provided a discrimination of low grip strength with an AUC of 0.648, and low walking speed with an AUC of 0.714. Importantly, when FFAs levels were added to the model, the value of the ROC curve was further improved, with an AUC of 0.785 for low grip strength and 0.755 for low walking speed.
Conclusions
The current study demonstrated a negative correlation between FFAs and muscle indicators in adult patients with T2D after adjusting for HbA1c levels. FFAs may play an important role in the pathological processes of muscle dysfunction in adults with T2D.



Similar content being viewed by others
Abbreviations
- T2D:
-
type 2 diabetes
- FFAs:
-
free fatty acids
- ASMM:
-
height-adjusted appendicular skeletal muscle mass
- ROC:
-
receiver operating characteristic curves
- BMI:
-
body mass index
- HbA1c:
-
hemoglobin A1C
- IDF:
-
International Diabetes Federation
- SBP:
-
systolic blood pressure
- DBP:
-
diastolic blood pressure
- ASM:
-
appendicular skeletal muscle
References
Y. Li, D. Teng, X. Shi, G. Qin, Y. Qin, H. Quan, B. Shi, H. Sun, J. Ba, B. Chen, et al., Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ 369, m997 (2020)
A.B. Engin, A. Engin, Protein kinases signaling in pancreatic beta-cells death and type 2 diabetes. Adv. Exp. Med. Biol. 1275, 195–227 (2021)
R.R. Kalyani, E.J. Metter, J. Egan, S.H. Golden, L. Ferrucci, Hyperglycemia predicts persistently lower muscle strength with aging. Diabetes Care 38, 82–90 (2015)
H. Umegaki, Sarcopenia and frailty in older patients with diabetes mellitus. Geriatr. Gerontol. Int. 16, 293–299 (2016)
M. Domański, K. Ciechanowski, Sarcopenia: a major challenge in elderly patients with end-stage renal disease. J. Aging Res. 2012, 754739 (2012)
K.S. Kim, K.S. Park, M.J. Kim, S.K. Kim, Y.W. Cho, S.W. Park, Type 2 diabetes is associated with low muscle mass in older adults. Geriatr. Gerontol. Int. 14(Suppl 1), 115–121 (2014)
T.N. Kim, M.S. Park, S.J. Yang, H.J. Yoo, H.J. Kang, W. Song, J.A. Seo, S.G. Kim, N.H. Kim, S.H. Baik et al. Prevalence and determinant factors of sarcopenia in patients with type 2 diabetes: the Korean Sarcopenic Obesity Study (KSOS). Diabetes Care 33, 1497–1499 (2010)
T. Wang, X. Feng, J. Zhou, H. Gong, S. Xia, Q. Wei, X. Hu, R. Tao, L. Li, F. Qian et al. Type 2 diabetes mellitus is associated with increased risks of sarcopenia and pre-sarcopenia in Chinese elderly. Sci. Rep. 6, 38937 (2016)
A. Bar, M. Targosz-Korecka, J. Suraj, B. Proniewski, A. Jasztal, B. Marczyk, M. Sternak, M. Przybyło, A. Kurpińska, M. Walczak et al. Degradation of glycocalyx and multiple manifestations of endothelial dysfunction coincide in the early phase of endothelial dysfunction before atherosclerotic plaque development in apolipoprotein E/low-density lipoprotein receptor-deficient mice. J. Am. Heart Assoc. 8, e011171 (2019)
S.M. Barbalho, U.A.P. Flato. Physical exercise and myokines: relationships with sarcopenia and cardiovascular complications. Int. J. Mol. Sci. 21, 3607 (2020)
S.S. Park, Y.K. Seo. Excess accumulation of lipid impairs insulin sensitivity in skeletal muscle. Int. J. Mol. Sci. 21, 1949 (2020)
M. Xue, F. Zhang, X. Ji, H. Yu, X. Jiang, Y. Qiu, J. Yu, J. Chen, F. Yang, Z. Bao, Oleate ameliorates palmitate-induced impairment of differentiative capacity in C2C12 myoblast cells. Stem Cells Dev. 30, 289–300 (2021)
A. Jiang, H. Guo, L. Zhang, X. Jiang, X. Zhang, W. Wu. Free fatty acid impairs myogenic differentiation through the AMPKα-MicroRNA 206 pathway. Mol. Cell Biol. 42, e0032721 (2022)
Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2019. Diabetes Care. 42, S13-S28 (2019).
L.K. Chen, L.K. Liu, J. Woo, P. Assantachai, T.W. Auyeung, K.S. Bahyah, M.Y. Chou, L.Y. Chen, P.S. Hsu, O. Krairit et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J. Am. Med. Dir. Assoc. 15, 95–101 (2014)
S.A. Arslanian, S.C. Kalhan, Correlations between fatty acid and glucose metabolism. Potential explanation of insulin resistance of puberty. Diabetes 43, 908–914 (1994)
R. Nishimura, Y. Tanaka, K. Koiwai, K. Ishida, A. Salsali, S. Kaspers, S. Kohler, S.S. Lund, Effect of empagliflozin on free fatty acids and ketone bodies in Japanese patients with type 2 diabetes mellitus: a randomized controlled trial. Nutrients. 36, 2769–2782 (2019)
D.A. Hood, J.M. Memme, A.N. Oliveira, M. Triolo, Maintenance of skeletal muscle mitochondria in health, exercise, and aging. Annu. Rev. Physiol. 81, 19–41 (2019)
X.M. Wei, W.B. Yang, X.X. Su, A.D. Zhang, W. Jin, Y.H. Fang, Plasma free fatty acid is associated with ischemic cardiomyopathy and cardiac dysfunction severity in systolic heart failure patients with diabetes. Chin. Med. J. 134, 472–474 (2020)
R. Vettor, G. Milan, C. Franzin, M. Sanna, P. De Coppi, R. Rizzuto, G. Federspil, The origin of intermuscular adipose tissue and its pathophysiological implications. Am. J. Physiol. Endocrinol. Metab. 297, E987–E998 (2009)
C. Brøns, L.G. Grunnet, Mechanisms in endocrinology: Skeletal muscle lipotoxicity in insulin resistance and type 2 diabetes: a causal mechanism or an innocent bystander? Eur. J. Endocrinol. 176, R67–R78 (2017)
Acknowledgements
The authors thank the participants for their continuing participation in this research effort.
Funding
This study was supported by Beijing Municipal Administration of Hospitals Incubating Program (PX2020034), Xuanwu Hospital Science Program for Fostering Young Scholars (QNPY2020014), the pilot project for public welfare development and reform of Beijing-affiliated medical research institutes (Beijing Medical Research 2021-8) and Capital Medical University Scientific Research Cultivation Fund (PYZ21033).
Author information
Authors and Affiliations
Contributions
JLF analyzed the data and wrote the manuscript; LNS and ZJM contributed to data collection; SLX contributed to the data interpretation, reviewed the manuscript and revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Informed consent
Informed consent was obtained from all individual participants and/or parents/guardians included in the study.
Research involving human participants and/or animals
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Fu, J., Sun, L., Mu, Z. et al. Free fatty acids are associated with muscle dysfunction in Chinese adults with type 2 diabetes. Endocrine 77, 41–47 (2022). https://doi.org/10.1007/s12020-022-03053-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-022-03053-4