Abstract
Purpose
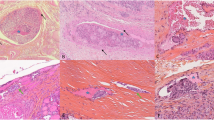
Lymph node metastasis is common in patients with papillary thyroid cancer (PTC). Some metastatic lymph nodes may present extranodal extension (ENE). The clinical role of ENE in PTC has yet to be clearly identified. We evaluated macroscopic ENE as a potential prognostic indicator of lung metastasis in PTC.
Patients and methods
We identified 1140 consecutive patients who had PTC initially resected at our cancer center. Clinical data and pathological results were reviewed. Univariate and multivariate logistic regression analyses were used to figure out the association between clinicopathological variables and lung metastasis.
Results
In this cohort, 51.7% of PTC patients had lymph node metastasis; 10.4% had macroscopic ENE positive nodes; 2.3% had lung metastasis. In patients with lymph node metastasis, the average number of positive nodes was 5.10 ± 4.91. Multivariable analysis of clinicopathological factors revealed that extrathyroidal extension (odds ratio [OR], 3.57; 95% CI, 1.41–9.04), macroscopic ENE (OR, 7.08; 95% CI, 2.54–19.74), and number of positive nodes were significantly associated with lung metastasis. Compared with 0–3 positive nodes, 7–9 positive nodes denoted a moderate risk of lung metastasis (OR, 4.53; 95% CI, 1.03–19.85). And 10 positive nodes or more indicated a high risk of lung metastasis (OR, 9.63; 95% CI, 2.65–35.02).
Conclusion
Macroscopic ENE could serve as a strong independent prognostic factor of lungmetastasis in PTC. More attention should be paid to patients with ENE positive nodes duringfollow-up.

Similar content being viewed by others
Data availability
The datasets generated analyzed during the current study are available from the corresponding author on reasonable request.
References
H. Park, J. Park, S.Y. Park, T.H. Kim, S.W. Kim, J.H. Chung, Clinical course from diagnosis to death in patients with well-differentiated thyroid cancer. Cancers 12(8) (2020). https://doi.org/10.3390/cancers12082323
J.D. Lin, T.C. Chao, S.C. Chou, C. Hsueh, Papillary thyroid carcinomas with lung metastases. Thyroid.: Off. J. Am. Thyroid. Assoc. 14(12), 1091–1096 (2004). https://doi.org/10.1089/thy.2004.14.1091
A. Machens, H. Dralle, Correlation between the number of lymph node metastases and lung metastasis in papillary thyroid cancer. J. Clin. Endocrinol. Metab. 97(12), 4375–4382 (2012). https://doi.org/10.1210/jc.2012-1257
Y.S. Lee, Y.S. Lim, J.C. Lee, S.G. Wang, I.J. Kim, S.M. Son, B.J. Lee, Clinical implications of bilateral lateral cervical lymph node metastasis in papillary thyroid cancer: a risk factor for lung metastasis. Ann. surgical Oncol. 18(12), 3486–3492 (2011). https://doi.org/10.1245/s10434-011-1763-7
Y.M. Park, S.G. Wang, D.H. Shin, I.J. Kim, S.M. Son, B.J. Lee, Lymph node status of lateral neck compartment in patients with N1b papillary thyroid carcinoma. Acta Oto-laryngologica 136(3), 319–324 (2016). https://doi.org/10.3109/00016489.2015.1116045
Y. Ito, T. Kudo, Y. Takamura, K. Kobayashi, A. Miya, A. Miyauchi, Prognostic factors of papillary thyroid carcinoma vary according to sex and patient age. World J. Surg. 35(12), 2684–2690 (2011). https://doi.org/10.1007/s00268-011-1288-z
M.B. Amin, F.L. Greene, S.B. Edge, C.C. Compton, J.E. Gershenwald, R.K. Brookland, L. Meyer, D.M. Gress, D.R. Byrd, D.P. Winchester, The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA: Cancer J. Clin. 67(2), 93–99 (2017). https://doi.org/10.3322/caac.21388
H.I. Kim, J. Hyeon, S.Y. Park, H.S. Ahn, K. Kim, J.M. Han, J.C. Bae, J.H. Shin, J.S. Kim, S.W. Kim, J.H. Chung, T.H. Kim, Y.L. Oh, Impact of extranodal extension on risk stratification in papillary thyroid carcinoma. Thyroid.: Off. J. Am. Thyroid. Assoc. 29(7), 963–970 (2019). https://doi.org/10.1089/thy.2018.0541
M.E. Rowe, U. Ozbek, R.A. Machado, L.E. Yue, J.C. Hernandez-Prera, A. Valentino, M. Qazi, M. Brandwein-Weber, X. Liu, B.M. Wenig, M.L. Urken, The prevalence of extranodal extension in papillary thyroid cancer based on the size of the metastatic node: adverse histologic features are not limited to larger lymph nodes. Endocr. Pathol. 29(1), 80–85 (2018). https://doi.org/10.1007/s12022-018-9518-7
J.L. Roh, J.W. Park, J. Jeong, G. Gong, K.J. Cho, S.H. Choi, S.Y. Nam, S.Y. Kim, Extranodal extension of lymph node metastasis as a prognostic indicator of recurrence and survival in papillary thyroid carcinoma. J. Surgical Oncol. 116(4), 450–458 (2017). https://doi.org/10.1002/jso.24713
J.W. Kim, J.L. Roh, G. Gong, K.J. Cho, S.H. Choi, S.Y. Nam, S.Y. Kim, Extent of extrathyroidal extension as a significant predictor of nodal metastasis and extranodal extension in patients with papillary thyroid carcinoma. Ann. surgical Oncol. 24(2), 460–468 (2017). https://doi.org/10.1245/s10434-016-5594-4
M.J. Shim, J.L. Roh, G. Gong, K.J. Choi, J.H. Lee, S.H. Cho, S.Y. Nam, S.Y. Kim, Preoperative detection and predictors of level V lymph node metastasis in patients with papillary thyroid carcinoma. Br. J. Surg. 100(4), 497–503 (2013). https://doi.org/10.1002/bjs.9024
G.W. Randolph, Q.Y. Duh, K.S. Heller, V.A. LiVolsi, S.J. Mandel, D.L. Steward, R.P. Tufano, R.M. Tuttle, American Thyroid Association Surgical Affairs Committee’s Taskforce on Thyroid Cancer Nodal, S.: The prognostic significance of nodal metastases from papillary thyroid carcinoma can be stratified based on the size and number of metastatic lymph nodes, as well as the presence of extranodal extension. Thyroid.: Off. J. Am. Thyroid. Assoc. 22(11), 1144–1152 (2012). https://doi.org/10.1089/thy.2012.0043
B.H. Lang, T.W. Shek, A.O. Chan, C.Y. Lo, K.Y. Wan, Significance of size of persistent/recurrent central nodal disease on surgical morbidity and response to therapy in reoperative neck dissection for papillary thyroid carcinoma. Thyroid.: Off. J. Am. Thyroid. Assoc. 27(1), 67–73 (2017). https://doi.org/10.1089/thy.2016.0337
C.W. Lee, J.L. Roh, G. Gong, K.J. Cho, S.H. Choi, S.Y. Nam, S.Y. Kim, Risk factors for recurrence of papillary thyroid carcinoma with clinically node-positive lateral neck. Ann. surgical Oncol. 22(1), 117–124 (2015). https://doi.org/10.1245/s10434-014-3900-6
S.H. Nam, J.L. Roh, G. Gong, K.J. Cho, S.H. Choi, S.Y. Nam, S.Y. Kim, Nodal factors predictive of recurrence after thyroidectomy and neck dissection for papillary thyroid carcinoma. Thyroid.: Off. J. Am. Thyroid. Assoc. 28(1), 88–95 (2018). https://doi.org/10.1089/thy.2017.0334
S.H. Lee, J.L. Roh, G. Gong, K.J. Cho, S.H. Choi, S.Y. Nam, S.Y. Kim, Risk Factors for recurrence after treatment of N1b papillary thyroid carcinoma. Ann. Surg. (2018). https://doi.org/10.1097/SLA.0000000000002710
E. Song, J. Ahn, D.E. Song, W.W. Kim, M.J. Jeon, T.Y. Sung, T.Y. Kim, K.W. Chung, W.B. Kim, Y.K. Shong, S.J. Hong, Y.M. Lee, W.G. Kim, Modified risk stratification based on cervical lymph node metastases following lobectomy for papillary thyroid carcinoma. Clin. Endocrinol. 92(4), 358–365 (2020). https://doi.org/10.1111/cen.14115
B.H. Lang, T.W. Shek, K.Y. Wan, Impact of microscopic extra-nodal extension (ENE) on locoregional recurrence following curative surgery for papillary thyroid carcinoma. J. Surgical Oncol. 113(5), 526–531 (2016). https://doi.org/10.1002/jso.24180
N. Chereau, C. Buffet, C. Tresallet, F. Tissier, L. Leenhardt, F. Menegaux, Recurrence of papillary thyroid carcinoma with lateral cervical node metastases: Predictive factors and operative management. Surgery 159(3), 755–762 (2016). https://doi.org/10.1016/j.surg.2015.08.033
M.L. Urken, G.C. Haser, I. Likhterov, B.M. Wenig, The impact of metastatic lymph nodes on risk stratification in differentiated thyroid cancer: have we reached a higher level of understanding? Thyroid.: Off. J. Am. Thyroid. Assoc. 26(4), 481–488 (2016). https://doi.org/10.1089/thy.2015.0544
M.H. Wu, W.T. Shen, J. Gosnell, Q.Y. Duh, Prognostic significance of extranodal extension of regional lymph node metastasis in papillary thyroid cancer. Head. Neck 37(9), 1336–1343 (2015). https://doi.org/10.1002/hed.23747
Y. Ito, T. Kudo, K. Kobayashi, A. Miya, K. Ichihara, A. Miyauchi, Prognostic factors for recurrence of papillary thyroid carcinoma in the lymph nodes, lung, and bone: analysis of 5,768 patients with average 10-year follow-up. World J. Surg. 36(6), 1274–1278 (2012). https://doi.org/10.1007/s00268-012-1423-5
Y.M. Lee, J.W. Cho, S.J. Hong, J.H. Yoon, Dynamic risk stratification in papillary thyroid carcinoma measuring 1 to 4 cm. J. surgical Oncol. 118(4), 636–643 (2018). https://doi.org/10.1002/jso.25182
M. Lango, D. Flieder, R. Arrangoiz, C. Veloski, J.Q. Yu, T. Li, B. Burtness, R. Mehra, T. Galloway, J.A. Ridge, Extranodal extension of metastatic papillary thyroid carcinoma: correlation with biochemical endpoints, nodal persistence, and systemic disease progression. Thyroid.: Off. J. Am. Thyroid. Assoc. 23(9), 1099–1105 (2013). https://doi.org/10.1089/thy.2013.0027
Y. Ito, A. Miyauchi, H. Masuoka, T. Higashiyama, M. Kihara, A. Miya, Prognostic value of extranodal tumor extension in papillary thyroid carcinoma: proposal for upstaging of cases with extranodal tumor extension. World J. Surg. 44(2), 638–643 (2020). https://doi.org/10.1007/s00268-019-05232-3
A.K. Leite, M.A. Kulcsar, B. de Godoi Cavalheiro, E.S. de Mello, V.A. Alves, C.R. Cernea, L.L. Matos, Death related to pulmonary metastasis in patients with differentiated thyroid cancer. Endocr. Pract.: Off. J. Am. Coll. Endocrinol. Am. Assoc. Clin. Endocrinol. 23(1), 72–78 (2017). https://doi.org/10.4158/ep161431.or
M. Kim, W.G. Kim, S. Park, H. Kwon, M.J. Jeon, J.J. Lee, J.S. Ryu, T.Y. Kim, Y.K. Shong, W.B. Kim, Initial size of metastatic lesions is best prognostic factor in patients with metastatic differentiated thyroid carcinoma confined to the lung. Thyroid.: Off. J. Am. Thyroid. Assoc. 27(1), 49–58 (2017). https://doi.org/10.1089/thy.2016.0347
Y.M. Lee, T.Y. Sung, W.B. Kim, K.W. Chung, J.H. Yoon, S.J. Hong, Risk factors for recurrence in patients with papillary thyroid carcinoma undergoing modified radical neck dissection. Br. J. Surg. 103(8), 1020–1025 (2016). https://doi.org/10.1002/bjs.10144
M.J. Jeon, W.G. Kim, Y.M. Choi, H. Kwon, Y.M. Lee, T.Y. Sung, J.H. Yoon, K.W. Chung, S.J. Hong, T.Y. Kim, Y.K. Shong, D.E. Song, W.B. Kim, Features predictive of distant metastasis in papillary thyroid microcarcinomas. Thyroid.: Off. J. Am. Thyroid. Assoc. 26(1), 161–168 (2016). https://doi.org/10.1089/thy.2015.0375
Funding
This study was funded by Henan Health Commission (Grant No. 2018020490).
Author information
Authors and Affiliations
Contributions
H.H. and J.W.Q. designed research; H.H., W.B.G., and C.Z. conducted research; H.H. and B.Z. analyzed data; H.H. wrote the paper; J.W.Q. had primary responsibility for final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval and consent to participate
The study was reviewed and approved by Institutional Review Board of the Affiliated Cancer Hospital of Zhengzhou University. This study was conducted in accordance with the Declaration of Helsinki.
Consent for publication
All authors have reviewed the final version of the manuscript and are in agreement its content and submission.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hei, H., Gong, W., Zheng, C. et al. Macroscopic extranodal extension is an independent predictor of lung metastasis in papillary thyroid cancer. Endocrine 77, 73–79 (2022). https://doi.org/10.1007/s12020-022-03045-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-022-03045-4