Abstract
Purpose
Antibiotics prescription in early life can cause dysbiosis, an imbalance of gut microbiota. We aimed to reveal the relationship between antibiotics exposure during the first 2 years after birth and type 1 diabetes risk in children under 8 years of age using a nationally representative data from South Korea.
Methods
The final study population consisted of 63,434 children from the National Health Insurance Service (NHIS) database from 2008 to 2015. The primary exposure of interest was antibiotics prescription in first 2 years after birth. The analysis was conducted with cumulative defined daily dose (cDDD; 0–29, 30–59, ≥ 60 cDDD), the number of antibiotics classes (0–3, 4, ≥5 classes), and age at first antibiotics prescription (0–119, 120–239, ≥ 240 days). Age, sex, household income, and overweight were considered as potential confounding covariates.
Results
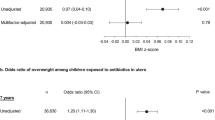
Compared to those within the less than 30 cDDD, other groups that were prescribed more antibiotics did not have a significant difference in diabetes risk (aHR 0.86, 95% CI 0.37–2.02 in ≥ 60 cDDD). The number of antibiotics classes and age at first antibiotics prescriptions were also not associated with the risk of type 1 diabetes. The development of diabetes was not related to the cDDD, the number of antibiotics classes, and age at first antibiotics prescription according to subgroup analysis which was stratified by overweight.
Conclusions
Antibiotics exposure within the first 2 years of life was not associated with subsequent diabetes risk. Future studies using a larger number of long-term follow-up data are needed.

Similar content being viewed by others
Data availability
This study used the NHIS database (NHIS-2020-2-072).
Code availability
SAS Enterprise Guide 7.1 (SAS Institute, Cary, NC, USA) was used to conduct all statistical analyzes.
References
C.C. Patterson, G.G. Dahlquist, E. Gyürüs, A. Green, G. Soltész, Incidence trends for childhood type 1 diabetes in Europe during 1989–2003 and predicted new cases 2005–20: a multicentre prospective registration study. Lancet 373(9680), 2027–2033 (2009). https://doi.org/10.1016/s0140-6736(09)60568-7
D. Dabelea, E.J. Mayer-Davis, S. Saydah, G. Imperatore, B. Linder, J. Divers, R. Bell, A. Badaru, J.W. Talton, T. Crume, A.D. Liese, A.T. Merchant, J.M. Lawrence, K. Reynolds, L. Dolan, L.L. Liu, R.F. Hamman; Study, S.f.D.i.Y., Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA 311(17), 1778–1786 (2014). https://doi.org/10.1001/jama.2014.3201
K. Hummel, K.K. McFann, J. Realsen, L.H. Messer, G.J. Klingensmith, H.P. Chase, The increasing onset of type 1 diabetes in children. J. Pediatr. 161(4), 652–657.e651 (2012). https://doi.org/10.1016/j.jpeds.2012.03.061
P.J. Carter, W.S. Cutfield, P.L. Hofman, A.J. Gunn, D.A. Wilson, P.W. Reed, C. Jefferies, Ethnicity and social deprivation independently influence metabolic control in children with type 1 diabetes. Diabetologia 51(10), 1835–1842 (2008). https://doi.org/10.1007/s00125-008-1106-9
H. Zhang, W. Xia, Q. Yu, B. Wang, S. Chen, Z. Wang, E.J. Love, Increasing incidence of type 1 diabetes in children aged 0-14 years in Harbin, China (1990–2000). Prim Care. Diabetes 2(3), 121–126 (2008). https://doi.org/10.1016/j.pcd.2008.06.001
M.E. Craig, A. Hattersley, K.C. Donaghue, Definition, epidemiology and classification of diabetes in children and adolescents. Pediatr. Diabetes 10(Suppl 12), 3–12 (2009). https://doi.org/10.1111/j.1399-5448.2009.00568.x
D.P., Group, Incidence and trends of childhood Type 1 diabetes worldwide 1990-1999. Diabet. Med 23(8), 857–866 (2006). https://doi.org/10.1111/j.1464-5491.2006.01925.x
D.J. Kim, The epidemiology of diabetes in Korea. Diabetes Metab. J. 35(4), 303–308 (2011). https://doi.org/10.4093/dmj.2011.35.4.303
D. Dabelea, J.M. Stafford, E.J. Mayer-Davis, R. D’Agostino Jr., L. Dolan, G. Imperatore, B. Linder, J.M. Lawrence, S.M. Marcovina, A.K. Mottl, M.H. Black, R. Pop-Busui, S. Saydah, R.F. Hamman, C. Pihoker; Group, S.f.D.i.Y.R., Association of type 1 diabetes vs type 2 diabetes diagnosed during childhood and adolescence with complications during teenage years and young adulthood. JAMA 317(8), 825–835 (2017). https://doi.org/10.1001/jama.2017.0686
K.T. Coppieters, F. Dotta, N. Amirian, P.D. Campbell, T.W. Kay, M.A. Atkinson, B.O. Roep, M.G. von Herrath, Demonstration of islet-autoreactive CD8 T cells in insulitic lesions from recent onset and long-term type 1 diabetes patients. J. Exp. Med. 209(1), 51–60 (2012). https://doi.org/10.1084/jem.20111187
C.F. Verge, R. Gianani, E. Kawasaki, L. Yu, M. Pietropaolo, H.P. Chase, G.S. Eisenbarth, R.A. Jackson, Prediction of type i diabetes in first-degree relatives using a combination of Insulin, GAD, and ICA512bdc/IA-2 autoantibodies. Diabetes 45(7), 926–933 (1996). https://doi.org/10.2337/diab.45.7.926
J.S. Skyler, J.P. Krischer, J. Wolfsdorf, C. Cowie, J.P. Palmer, C. Greenbaum, D. Cuthbertson, L.E. Rafkin-Mervis, H.P. Chase, E. Leschek, Effects of oral insulin in relatives of patients with type 1 diabetes: the diabetes prevention trial–type 1. Diabetes Care 28(5), 1068–1076 (2005). https://doi.org/10.2337/diacare.28.5.1068
S. Candon, A. Perez-Arroyo, C. Marquet, F. Valette, A.P. Foray, B. Pelletier, C. Milani, M. Ventura, J.F. Bach, L. Chatenoud, Antibiotics in early life alter the gut microbiome and increase disease incidence in a spontaneous mouse model of autoimmune insulin-dependent diabetes. PLoS One 10(5), e0125448 (2015). https://doi.org/10.1371/journal.pone.0125448
G. Tapia, K. Stordal, K. Marild, C.R. Kahrs, T. Skrivarhaug, P.R. Njolstad, G. Joner, L.C. Stene, Antibiotics, acetaminophen and infections during prenatal and early life in relation to type 1 diabetes. Int J. Epidemiol. 47(5), 1538–1548 (2018). https://doi.org/10.1093/ije/dyy092
L.C. Bailey, C.B. Forrest, P. Zhang, T.M. Richards, A. Livshits, P.A. DeRusso, Association of antibiotics in infancy with early childhood obesity. JAMA Pediatr. 168(11), 1063–1069 (2014). https://doi.org/10.1001/jamapediatrics.2014.1539
F.I. Scott, D.B. Horton, R. Mamtani, K. Haynes, D.S. Goldberg, D.Y. Lee, J.D. Lewis, Administration of antibiotics to children before age 2 years increases risk for childhood obesity. Gastroenterology 151(1), 120–129.e125 (2016). https://doi.org/10.1053/j.gastro.2016.03.006
Y.J. Park, J. Chang, G. Lee, J.S. Son, S.M. Park, Association of class number, cumulative exposure, and earlier initiation of antibiotics during the first two-years of life with subsequent childhood obesity. Metabolism 112, 154348 (2020). https://doi.org/10.1016/j.metabol.2020.154348
K.D. Corbin, K.A. Driscoll, R.E. Pratley, S.R. Smith, D.M. Maahs, E.J. Mayer-Davis, Advancing care for type, D., Obesity, N.: obesity in type 1 diabetes: pathophysiology, clinical impact, and mechanisms. Endocr. Rev. 39(5), 629–663 (2018). https://doi.org/10.1210/er.2017-00191
K.C. Verbeeten, C.E. Elks, D. Daneman, K.K. Ong, Association between childhood obesity and subsequent Type 1 diabetes: a systematic review and meta-analysis. Diabet. Med 28(1), 10–18 (2011). https://doi.org/10.1111/j.1464-5491.2010.03160.x
N. Vilarrasa, P. San Jose, M.Á. Rubio, A. Lecube, Obesity in patients with type 1 diabetes: links, risks and management challenges. Diabetes Metab. Syndr. Obes.: Targets Ther. ume 14, 2807–2827 (2021). https://doi.org/10.2147/dmso.s223618
T.J. Wilkin, The convergence of type 1 and type 2 diabetes in childhood: the accelerator hypothesis. Pediatr. Diabetes 13(4), 334–339 (2012). https://doi.org/10.1111/j.1399-5448.2011.00831.x
A. Kilkkinen, S.M. Virtanen, T. Klaukka, M.G. Kenward, M. Salkinoja-Salonen, M. Gissler, M. Kaila, A. Reunanen, Use of antimicrobials and risk of type 1 diabetes in a population-based mother–child cohort. Diabetologia 49(1), 66–70 (2006). https://doi.org/10.1007/s00125-005-0078-2
T.D. Clausen, T. Bergholt, O. Bouaziz, M. Arpi, F. Eriksson, S. Rasmussen, N. Keiding, E.C. Lokkegaard, Broad-spectrum antibiotic treatment and subsequent childhood type 1 diabetes: a nationwide danish cohort study. PLoS One 11(8), e0161654 (2016). https://doi.org/10.1371/journal.pone.0161654
S. Cheol Seong, Y.Y. Kim, Y.H. Khang, J. Heon Park, H.J. Kang, H. Lee, C.H. Do, J.S. Song, J. Hyon Bang, S. Ha, E.J. Lee, S. Ae Shin, Data resource profile: the national health information database of the National Health Insurance Service in South Korea. Int J. Epidemiol. 46(3), 799–800 (2017). https://doi.org/10.1093/ije/dyw253
J.H. Lee, Y.M. Kim, M.J. Kwak, S.Y. Kim, H.J. Kim, C.K. Cheon, W.Y. Chung, I.J. Choi, S.Y. Hong, H.W. Chueh, J.H. Yoo, Incidence trends and associated factors of diabetes mellitus in Korean children and adolescents: a retrospective cohort study in Busan and Gyeongnam. Ann. Pediatr. Endocrinol. Metab. 20(4), 206–212 (2015). https://doi.org/10.6065/apem.2015.20.4.206
T. Yatsunenko, F.E. Rey, M.J. Manary, I. Trehan, M.G. Dominguez-Bello, M. Contreras, M. Magris, G. Hidalgo, R.N. Baldassano, A.P. Anokhin, A.C. Heath, B. Warner, J. Reeder, J. Kuczynski, J.G. Caporaso, C.A. Lozupone, C. Lauber, J.C. Clemente, D. Knights, R. Knight, J.I. Gordon, Human gut microbiome viewed across age and geography. Nature 486(7402), 222–227 (2012). https://doi.org/10.1038/nature11053
WHO Collaborating Centre for Drug Statistics Methodology, Guidelines for ATC classification and DDD assignment, 2020. Oslo (2019).
S.R. Daniels, S.G. Hassink, Committee On, N.: the role of the pediatrician in primary prevention of obesity. Pediatrics 136(1), e275–e292 (2015). https://doi.org/10.1542/peds.2015-1558
J.H. Kim, S. Yun, S.S. Hwang, J.O. Shim, H.W. Chae, Y.J. Lee, J.H. Lee, S.C. Kim, D. Lim, S.W. Yang, K. Oh, J.S. Moon, Committee for the Development of Growth Standards for Korean, C., Adolescents, Committee for School, H., Public Health Statistics, t.K.P.S., Division of, H., Nutrition Survey, K.C.f.D.C., Prevention: The 2017 Korean National Growth Charts for children and adolescents: development, improvement, and prospects. Korean J. Pediatr. 61(5), 135–149 (2018). https://doi.org/10.3345/kjp.2018.61.5.135
G. Chai, L. Governale, A.W. McMahon, J.P. Trinidad, J. Staffa, D. Murphy, Trends of outpatient prescription drug utilization in US children, 2002-2010. Pediatrics 130(1), 23–31 (2012). https://doi.org/10.1542/peds.2011-2879
P. Vangay, T. Ward, J.S. Gerber, D. Knights, Antibiotics, pediatric dysbiosis, and disease. Cell Host Microbe 17(5), 553–564 (2015). https://doi.org/10.1016/j.chom.2015.04.006
S. Sharma, P. Tripathi, Gut microbiome and type 2 diabetes: where we are and where to go? J. Nutr. Biochem. 63, 101–108 (2019). https://doi.org/10.1016/j.jnutbio.2018.10.003
K.S.W. Leong, J.G.B. Derraik, P.L. Hofman, W.S. Cutfield, Antibiotics, gut microbiome and obesity. Clin. Endocrinol. (Oxf.) 88(2), 185–200 (2018). https://doi.org/10.1111/cen.13495
A. Paun, J.S. Danska, Modulation of type 1 and type 2 diabetes risk by the intestinal microbiome. Pediatr. Diabetes 17(7), 469–477 (2016). https://doi.org/10.1111/pedi.12424
G.L.V. de Oliveira, A.Z. Leite, B.S. Higuchi, M.I. Gonzaga, V.S. Mariano, Intestinal dysbiosis and probiotic applications in autoimmune diseases. Immunology 152(1), 1–12 (2017). https://doi.org/10.1111/imm.12765
A.M. Abdellatif, N.E. Sarvetnick, Current understanding of the role of gut dysbiosis in type 1 diabetes. J. Diabetes 11(8), 632–644 (2019). https://doi.org/10.1111/1753-0407.12915
T.M. Davis, Ethnic diversity in type 2 diabetes. Diabet. Med 25(Suppl 2), 52–56 (2008). https://doi.org/10.1111/j.1464-5491.2008.02499.x
J.H. Kim, C.G. Lee, Y.A. Lee, S.W. Yang, C.H. Shin, Increasing incidence of type 1 diabetes among Korean children and adolescents: analysis of data from a nationwide registry in Korea. Pediatr. Diabetes 17(7), 519–524 (2016). https://doi.org/10.1111/pedi.12324
E.J. Mayer-Davis, J.M. Lawrence, D. Dabelea, J. Divers, S. Isom, L. Dolan, G. Imperatore, B. Linder, S. Marcovina, D.J. Pettitt, C. Pihoker, S. Saydah, L. Wagenknecht; Study, S.f.D.i.Y., Incidence trends of type 1 and type 2 diabetes among youths, 2002-2012. N. Engl. J. Med 376(15), 1419–1429 (2017). https://doi.org/10.1056/NEJMoa1610187
M.E. Falagas, M. Kompoti, Obesity and infection. Lancet Infect. Dis. 6(7), 438–446 (2006). https://doi.org/10.1016/s1473-3099(06)70523-0
J. Dobner, S. Kaser, Body mass index and the risk of infection–from underweight to obesity. Clin. Microbiol. Infect. 24(1), 24–28 (2018). https://doi.org/10.1016/j.cmi.2017.02.013
Y.J. Choe, J.-Y. Shin, Trends in the use of antibiotics among Korean children. Korean J. Pediatr. 62(4), 113–118 (2019). https://doi.org/10.3345/kjp.2018.07290
I. Youngster, J. Avorn, V. Belleudi, A. Cantarutti, J. Diez-Domingo, U. Kirchmayer, B.J. Park, S. Peiro, G. Sanfelix-Gimeno, H. Schroder, K. Schussel, J.Y. Shin, S.M. Shin, G.S. Simonsen, H.S. Blix, A. Tong, G. Trifiro, T. Ziv-Baran, S.C. Kim, Antibiotic use in children - a cross-national analysis of 6 countries. J. Pediatr.-Us 182, 239–244 (2017). https://doi.org/10.1016/j.jpeds.2016.11.027
Author contributions
S.M.P. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: D.H.L., S.G.C., S.M.P. Acquisition of data: D.H.L., J.Y.C., S.M.P. Analysis and interpretation of data: D.H.L., S.G.C., J.Y.C., Y.J.P., S.M.P. Drafting of the manuscript: D.H.L., S.G.C., S.M.P. Critical revision of the manuscript: J.H.K., S.M.P. Statistical analysis: D.H.L., S.G.C., J.Y.C., Y.J.P. Administrative, technical, or material support: J.Y.C., S.G.C., S.M.P.
Funding
This research was supported by the Basic Science Research Program by the National Research Foundation of Korea (grant number: 2017R1D1A1B03033721).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Consent for publication
The Ministry of Health and Welfare and National Research Foundation of Korea had no role in the design and conduct of the study, the collection, management, analysis, and interpretation of the data, or the preparation, review, or approval of the manuscript, and decision to submit for publication.
Consent to participate
The requirement for informed consent was waived as the NHIS data is anonymized according to strict confidentiality guidelines prior to distribution.
Ethics approval
This study was approved by the Seoul National University Hospital Institutional Review Board (IRB number: E-1904-003-1021).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Lee, D., Choi, S., Chang, J. et al. Association of antibiotics exposure within the first 2 years after birth with subsequent childhood type 1 diabetes. Endocrine 77, 21–29 (2022). https://doi.org/10.1007/s12020-022-03042-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-022-03042-7