Abstract
Objective
To analyze the evolution of the cardiometabolic profile of patients with primary hyperaldosteronism (PA) after the treatment with surgery and with mineralocorticoid receptor antagonists (MRA).
Design
Retrospective multicentric study of patients with PA on follow-up in twelve Spanish centers between 2018 and 2020.
Results
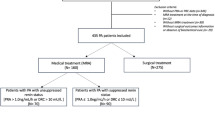
268 patients with PA treated by surgery (n = 100) or with MRA (n = 168) were included. At baseline, patients treated with surgery were more commonly women (54.6% vs 41.7%, P = 0.042), had a higher prevalence of hypokalemia (72.2% vs 58%, P = 0.022) and lower prevalence of obesity (37.4% vs 51.3%, P = 0.034) than patients treated with MRA. Adrenalectomy resulted in complete biochemical cure in 94.0% and clinical response in 83.0% (complete response in 41.0% and partial response in 42.0%). After a median follow-up of 23.6 (IQR 9.7–53.8) months, the reduction in blood pressure (BP) after treatment was similar between the group of surgery and MRA, but patients surgically treated reduced the number of antihypertensive pills for BP control more than those medically treated (∆antihypertensives: −1.3 ± 1.3 vs 0.0 ± 1.4, P < 0.0001) and experienced a higher increased in serum potassium levels (∆serum potassium: 0.9 ± 0.7 vs 0.6 ± 0.8mEq/ml, P = 0.003). However, no differences in the risk of the onset of new renal and cardiometabolic comorbidities was observed between the group of surgery and MRA (HR = 0.9 [0.5–1.5], P = 0.659).
Conclusion
In patients with PA, MRA and surgery offer a similar short-term cardiovascular protection, but surgery improves biochemical control and reduces pill burden more commonly than MRA, and lead to hypertension cure or improvement in up to 83% of the patients.


Similar content being viewed by others
References
G.P. Rossi, G. Bernini, C. Caliumi, G. Desideri, B. Fabris, C. Ferri et al. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J. Am. Coll. Cardiol. 48, 2293–2300 (2006) https://doi.org/10.1016/j.jacc.2006.07.059
P. Milliez, X. Girerd, P.F. Plouin, J. Blacher, M.E. Safar, J.J. Mourad et al. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J. Am. Coll. Cardiol. 45, 1243–1248 (2005) https://doi.org/10.1016/j.jacc.2005.01.015
G.P. Rossi, G. Bernini, G. Desideri, B. Fabris, C. Ferri, G. Giacchetti et al. Renal damage in primary aldosteronism: results of the PAPY study. Hypertension 48, 232–238 (2006) https://doi.org/10.1161/01.HYP.0000230444.01215.6a
C. Catena, G. Colussi, R. Lapenna, E. Nadalini, A. Chiuch, P. Gianfagna et al. Long-term cardiac effects of adrenalectomy or mineralocorticoid antagonists in patients with primary aldosteronism. Hypertension 50, 911–918 (2007). https://doi.org/10.1161/HYPERTENSIONAHA.107.095448
M. Fernández-Argüeso, E. Pascual-Corrales, N. Bengoa Rojano, A. García Cano, L. Jiménez Mendiguchía, M. Araujo-Castro, Higher risk of chronic kidney disease and progressive kidney function impairment in primary aldosteronism than in essential hypertension. Case-control study. Endocrine 73, 439–446 (2021). https://doi.org/10.1007/s12020-021-02704-2
S. Monticone, F. D’Ascenzo, C. Moretti, T.A. Williams, F. Veglio, F. Gaita et al. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 6, 41–50 (2018). https://doi.org/10.1016/S2213-8587(17)30319-4
G.L. Hundemer, G.C. Curhan, N. Yozamp, M. Wang, A. Vaidya, Incidence of atrial fibrillation and mineralocorticoid receptor activity in patients with medically and surgically treated primary aldosteronism. JAMA Cardiol. 3, 768–774 (2018). https://doi.org/10.1001/jamacardio.2018.2003
C.T. Pan, C.W. Liao, C.H.T sai, Z.W. Chen, L. Chen, C.S. Hung et al. Influence of different treatment strategies on new-onset atrial fibrillation among patients with primary aldosteronism: a nationwide longitudinal cohort-based study. J. Am. Heart Assoc. 9 (2020). https://doi.org/10.1161/JAHA.119.013699
G.P. Rossi, G. Maiolino, A. Flego, A. Belfiore, G. Bernini, B. Fabris et al. Adrenalectomy lowers incident atrial fibrillation in primary aldosteronism patients at long term. Hypertension 71, 585–591 (2018). https://doi.org/10.1161/hypertensionaha.117.10596
A.H. Ahmed, R.D. Gordon, N. Sukor, E. Pimenta, M. Stowasser, Quality of life in patients with bilateral primary aldosteronism before and during treatment with spironolactone and/or amiloride, including a comparison with our previously published results in those with unilateral disease treated surgically. J. Clin. Endocrinol. Metab. 96, 2904–2911 (2011). https://doi.org/10.1210/jc.2011-0138
G.L. Hundemer, G.C. Curhan, N. Yozamp, M. Wang, A. Vaidya, H. GL et al. Renal outcomes in medically and surgically treated primary aldosteronism. Hypertension 72, 658–666 (2018). https://doi.org/10.1161/HYPERTENSIONAHA.118.11568
Y. Jing, K. Liao, R. Li, S. Yang, Y. Song, W. He et al. Cardiovascular events and all-cause mortality in surgically or medically treated primary aldosteronism: a Meta-analysis. J Renin-Angiotensin-Aldosterone Syst. 22, (2021). https://doi.org/10.1177/14703203211003781
C. Catena, G.L. Colussi, E. Nadalini, A. Chiuch, S. Baroselli, R. Lapenna et al. Cardiovascular outcomes in patients with primary aldosteronism after treatment. Arch. Intern. Med. 168, 80–85 (2008). https://doi.org/10.1001/archinternmed.2007.33
T.H. Puar, L.M. Loh, W.J. Loh, D.S.T. Lim, M. Zhang, P.T. Tan et al. Outcomes in unilateral primary aldosteronism after surgical or medical therapy. Clin. Endocrinol. 94, 158–167 (2021). https://doi.org/10.1111/cen.14351
C. Catena, R. Lapenna, S. Baroselli, E. Nadalini, G.L. Colussi, M. Novello et al. Insulin sensitivity in patients with primary aldosteronism: a follow-up study. J. Clin. Endocrinol. Metab. (2006). https://doi.org/10.1210/jc.2006-0736
L.A. Sechi, A.D.I. Fabio, M. Bazzocchi, A. Uzzau, C. Catena, Intrarenal hemodynamics in primary aldosteronism before and after treatment. J. Clin. Endocrinol. Metab. 94, 1191–1197 (2009). https://doi.org/10.1210/jc.2008-2245
B. Williams, G. Mancia, W. Spiering, E.A. Rosei, M. Azizi, M. Burnier et al. 2018 ESC/ESHGuidelines for themanagement of arterial hypertension. J. Hypertens. 36, 1956–2041 (2018). https://doi.org/10.1097/HJH.0000000000001940
A.S. Levey, J. Coresh, K. Bolton, B. Culleton, K.S. Harvey, T.A. Ikizler et al. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am. J. Kidney Dis. 39, 3–10 (2002).
J.W. Funder, R.M. Carey, F. Mantero, M.H. Murad, M. Reincke, H. Shibata et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 101, 1889–1916 (2016). https://doi.org/10.1210/jc.2015-4061
P. Mulatero, S. Monticone, J. Deinum, L. Amar, A. Prejbisz, M.C. Zennaro et al. Genetics, prevalence, screening and confirmation of primary aldosteronism: a position statement and consensus of the Working Group on Endocrine Hypertension of The European Society of Hypertension. J. Hypertens. 38, 1919–1928 (2020). https://doi.org/10.1097/HJH.0000000000002510
T.A. Williams, J.W.M. Lenders, P. Mulatero, J. Burrello, M. Rottenkolber, C. Adolf et al. Outcomes after adrenalectomy for unilateral primary aldosteronism: an international consensus on outcome measures and analysis of remission rates in an international cohort. Lancet Diabetes Endocrinol. 5, 689–699 (2017). https://doi.org/10.1016/S2213-8587(17)30135-3
O. Picado, B.W. Whitfield, Z.F. Khan, M. Jeraq, J.C. Farrá, J.I. Lew, Long-term outcome success after operative treatment for primary aldosteronism. Surgery 169, 528–532 (2021). https://doi.org/10.1016/j.surg.2020.07.046
A.M. Sawka, J. Young, G.B. Thompson, C.S. Grant, D.R. Farley, C. Leibson et al. Primary aldosteronism: factors associated with normalization of blood pressure after surgery. Ann. Intern. Med. 135, 258–261 (2001). https://doi.org/10.7326/0003-4819-135-4-200108210-00010
E. Letavernier, S. Peyrard, L. Amar, F. Zinzindohoué, B. Fiquet, P.F. Plouin, Blood pressure outcome of adrenalectomy in patients with primary hyperaldosteronism with or without unilateral adenoma. J. Hypertens. 26, 1816–1823 (2008). https://doi.org/10.1097/HJH.0b013e3283060f0c
V.C. Wu, K.H. Huang, K.Y. Peng, Y.C.T. sai, C.H. Wu, S.M. Wang et al. Prevalence and clinical correlates of somatic mutation in aldosterone producing adenoma-Taiwanese population. Sci. Rep. 15 (2015). https://doi.org/10.1038/srep11396
J.L. Benham, M. Eldoma, B. Khokhar, D.J. Roberts, D.M. Rabi, G.A. Kline, Proportion of patients with hypertension resolution following adrenalectomy for primary aldosteronism: a systematic review and meta-analysis. J. Clin. Hypertens. 18, 1205–1212 (2016). https://doi.org/10.1111/jch.12916
L. Marzano, G. Colussi, L.A. Sechi, C. Catena, Adrenalectomy is comparable with medical treatment for reduction of left ventricular mass in primary aldosteronism: meta-analysis of long-term studies. Am. J. Hypertens. (2015). https://doi.org/10.1093/ajh/hpu154
G.P. Rossi, M. Cesari, C. Cuspidi, G. Maiolino, M.V. Cicala, V. Bisogni et al. Long-term control of arterial hypertension and regression of left ventricular hypertrophy with treatment of primary aldosteronism. Hypertension 62, 62–69 (2013). https://doi.org/10.1161/HYPERTENSIONAHA.113.01316
M. Satoh, T. Maruhashi, Y. Yoshida, H. Shibata, Systematic review of the clinical outcomes of mineralocorticoid receptor antagonist treatment versus adrenalectomy in patients with primary aldosteronism. Hypertens. Res. 42, 817–824 (2019). https://doi.org/10.1038/s41440-019-0244-4
B. Lechner, K. Lechner, D. Heinrich, C. Adolf, F. Holler, H. Schneider et al. Medical treatment of primary aldosteronism. Eur. J. Endocrinol. 181, R147–R153 (2019). https://doi.org/10.1530/EJE-19-0215
G.L. Hundemer, G.C. Curhan, N. Yozamp, M. Wang, A. Vaidya, Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: a retrospective cohort study. Lancet Diabetes Endocrinol. 6, 51–59 (2018). https://doi.org/10.1016/S2213-8587(17)30367-4
A. Köhler, A.L. Sarkis, D.A. Heinrich, L. Müller, L. Handgriff, S. Deniz et al. Renin, a marker for left ventricular hypertrophy, in primary aldosteronism: a cohort study. Eur. J. Endocrinol. 185, 663–672 (2021). https://doi.org/10.1530/EJE-21-0018
Y. Tezuka, A.F. Turcu, Mineralocorticoid receptor antagonists decrease the rates of positive screening for primary aldosteronism. Endocr. Pract. 26, 1416–1424 (2020). https://doi.org/10.4158/EP-2020-0277
M. Velema, T. Dekkers, A. Hermus, H. Timmers, J. Lenders, H. Groenewoud, et al. Quality of life in primary aldosteronism: a comparative effectiveness study of adrenalectomy and medical treatment. J. Clin. Endocrinol. Metab. 103, 16–24 (2018). https://doi.org/10.1210/jc.2017-01442
G. Bernini, A. Bacca, V. Carli, D. Carrara, G. Materazzi, P. Berti et al. Cardiovascular changes in patients with primary aldosteronism after surgical or medical treatment. J. Endocrinol. Investig. 35, 274–280 (2012). https://doi.org/10.3275/7611
J.W. Funder, M. Reincke, Aldosterone: a cardiovascular risk factor? Biochim. Biophys. Acta—Mol. Basis Dis. 1802, 1188–1192 (2010). https://doi.org/10.1016/j.bbadis.2010.08.005
N.K. Hollenberg, Aldosterone in the development and progression of renal injury. Kidney Int. 66, 1–9 (2004). https://doi.org/10.1111/j.1523-1755.2004.00701.x
B. Pitt, N. Reichek, R. Willenbrock, F. Zannad, R.A. Phillips, B. Roniker et al. Effects of eplerenone, enalapril, and eplerenone/enalapril in patients with essential hypertension and left ventricular hypertrophy: the 4e-left ventricular hypertrophy study. Circulation 108, 1831–1838 (2003). https://doi.org/10.1161/01.CIR.0000091405.00772.6E
H. Fukuta, T. Goto, K. Wakami, T. Kamiya, N. Ohte, Effects of mineralocorticoid receptor antagonists on left ventricular diastolic function, exercise capacity, and quality of life in heart failure with preserved ejection fraction: a meta-analysis of randomized controlled trials. Heart Vessels 34, 597–606 (2019). https://doi.org/10.1007/s00380-018-1279-1
W. Arlt, K. Lang, A.J. Sitch, A.S. Dietz, Y. Rhayem, I. Bancos et al. Steroid metabolome analysis reveals prevalent glucocorticoid excess in primary aldosteronism. JCI Insight 2, (2017). https://doi.org/10.1172/JCI.INSIGHT.93136
Y. Tezuka, A.F. Turcu, Real-world effectiveness of mineralocorticoid receptor antagonists in primary aldosteronism. Front. Endocrinol 21, (2021). https://doi.org/10.3389/FENDO.2021.625457
M.J.E. Kempers, J.W.M. Lenders, L. Van Outheusden, G.J. Van Der Wilt, L.J.S. Kool, A.R.M.M. Hermus et al. Systematic review: diagnostic procedures to differentiate unilateral from bilateral adrenal abnormality in primary aldosteronism. Ann. Intern. Med. 151, (2009). https://doi.org/10.7326/0003-4819-151-5-200909010-00007
M.H. Wu, F.H. Liu, K.J. Lin, J.H. Sun, S.T. Chen, Diagnostic value of adrenal iodine-131 6-beta-iodomethyl-19-norcholesterol scintigraphy for primary aldosteronism: a retrospective study at a medical center in North Taiwan. Nucl. Med. Commun. 40, 568–575 (2019). https://doi.org/10.1097/MNM.0000000000000987
Funding
This research was funded by Sociedad Española de Endocrinología y Nutrición (SEEN) https://www.seen.es/portal.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Informed consent statement
Patient consent was waived due to the retrospective nature of the study. Only for patients who continued follow-up or prospectively included the informed consent was requested.
Institutional review board statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the Hospital Universitario Ramón y Cajal. Madrid. Spain (approval date: 10th November 2020, code: ACTA 401).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Araujo-Castro, M., Paja Fano, M., González Boillos, M. et al. Evolution of the cardiometabolic profile of primary hyperaldosteronism patients treated with adrenalectomy and with mineralocorticoid receptor antagonists: results from the SPAIN-ALDO Registry. Endocrine 76, 687–696 (2022). https://doi.org/10.1007/s12020-022-03029-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-022-03029-4