Abstract
Context
Spinal Epidural Lipomatosis (SEL) is a rare and frequently unrecognized complication of Cushing syndrome (CS). Only nine previous cases of SEL have been described in CS. Here, we present a case of severe SEL and review the literature.
Case report
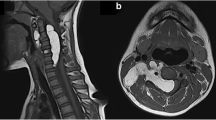
A 29-year-old man who had severe CS secondary to an ACTH-secreting pituitary macroadenoma. He presented with progressive lower limb weakness over a 2-year period leading to complete paraplegia in the last 4 months. In addition, he had classic symptoms and signs of severe CS. His evaluation confirmed the diagnosis of CS with a 4-fold increase in his daily free urinary cortisol (1190 mg/day), a positive 1-mg dexamethasone suppression test (AM cortisol 729 nmol/l) and an elevated ACTH of 196 ng/dl (10–65). Magnetic resonance imaging (MRI) revealed a 20-mm pituitary adenoma and extensive fat accumulation in the spinal canal extending from C7 to S5 with significant spinal cord compression from T2-T10. The patient underwent an urgent spinal cord decompression surgery. He showed an immediate improvement and was able to walk with crutches 3 weeks later and independently 3 months later. About 13 days after the spinal surgery, he underwent a trans-sphenoidal surgery resulting in eucortisolemia.
Conclusion
SEL is a rare and serious complication of CS. It should be considered in any patient with CS, especially when there is neurological symptoms or disproportionate weakness of the lower limbs. Its management should be individualized but prompt surgical decompression should be considered even in patients with relatively long history of paraparesis.



Similar content being viewed by others
References
R. Pivonello, A.M. Isidori, M.C. De Martino, J. Newell-Price, B.M. Biller, A. Colao, Complications of Cushing’s syndrome: state of the art. Lancet Diabetes Endocrinol. 4(7), 611–629 (2016). https://doi.org/10.1016/s2213-8587(16)00086-3
S.M. Webb, E. Valassi, Morbidity of Cushing’s syndrome and impact of treatment. Endocrinol. Metab. Clin. North Am. 47(2), 299–311 (2018). https://doi.org/10.1016/j.ecl.2018.01.001
H. Cushing, The basophil adenomas of the pituitary body and their clinical manifestations (pituitary basophilism). J. Neurosurg. 21(4), 318–347 (1964)
G. Ntali, A. Grossman, N. Karavitaki, Clinical and biochemical manifestations of Cushing’s. Pituitary 18(2), 181–187 (2015). https://doi.org/10.1007/s11102-014-0631-4
E.B. Geer, W. Shen, D. Gallagher, M. Punyanitya, H.C. Looker, K.D. Post et al. MRI assessment of lean and adipose tissue distribution in female patients with Cushing’s disease. Clin. Endocrinol. 73(4), 469–475 (2010). https://doi.org/10.1111/j.1365-2265.2010.03829.x
E.B. Geer, W. Shen, E. Strohmayer, K.D. Post, P.U. Freda, Body composition and cardiovascular risk markers after remission of Cushing’s disease: a prospective study using whole-body MRI. J. Clin. Endocrinol. Metab. 97(5), 1702–1711 (2012). https://doi.org/10.1210/jc.2011-3123
P.B. Walker, C. Sark, G. Brennan, T. Smith, W.F. Sherman, A.D. Kaye, Spinal epidural lipomatosis: a comprehensive review. Orthop. Rev. 13(2), 25571 (2021). https://doi.org/10.52965/001c.25571
K. Kim, J. Mendelis, W. Cho, Spinal epidural lipomatosis: a review of pathogenesis, characteristics, clinical presentation, and management. Glob. Spine J. 9(6), 658–665 (2019). https://doi.org/10.1177/2192568218793617
D. Al-Khawaja, K. Seex, G.D. Eslick, Spinal epidural lipomatosis–a brief review. J. Clin. Neurosci. 15(12), 1323–1326 (2008). https://doi.org/10.1016/j.jocn.2008.03.001
K. Chaudhary, D. Chandy, V. Agrawal, A. Dhawale, S. Nagaonkar, Spinal epidural lipomatosis with osteoporotic vertebral fractures presenting as acute thoracic myelopathy in a 33-year-old man with Cushing disease. World Neurosurg. 142, 136–141 (2020). https://doi.org/10.1016/j.wneu.2020.06.212
P. Noël, T. Pepersack, A. Vanbinst, J.-L. Allé, Spinal epidural lipomatosis in Cushing’s syndrome secondary to an adrenal tumor. Neurology 42(6), 1250 (1992). https://doi.org/10.1212/wnl.42.6.1250
K. Sivakumar, K. Sheinart, M. Lidov, B. Cohen, Symptomatic spinal epidural lipomatosis in a patient with Cushing’s disease. Neurology 45(12), 2281–2283 (1995). https://doi.org/10.1212/wnl.45.12.2281
D. Dumont-Fischer, A.C. Rat, N. Saidenberg-Kermanac’h, S. Laurent, R. Cohen, M.C. Boissier, Spinal epidural lipomatosis revealing endogenous Cushing’s syndrome. Jt. Bone Spine 69(2), 222–225 (2002). https://doi.org/10.1016/s1297-319x(02)00382-2
C.A. Koch, J.L. Doppman, N.J. Patronas, L.K. Nieman, G.P. Chrousos, Do glucocorticoids cause spinal epidural lipomatosis? When endocrinology and spinal surgery meet. Trends Endocrinol. Metab. 11, 86–90 (2000)
A.G. Bodelier, W. Groeneveld, A.N. van der Linden, H.R. Haak, Symptomatic epidural lipomatosis in ectopic Cushing’s syndrome. Eur. J. Endocrinol. 151(6), 765–769 (2004). https://doi.org/10.1530/eje.0.1510765
K. Bhatia, E. Frydenberg, T. Steel, M. Ow-Yang, K. Ho, E. Grainger, Spinal epidural lipomatosis due to a bronchial ACTH-secreting carcinoid tumour. J. Clin. Neurosci. 17(11), 1461–1462 (2010). https://doi.org/10.1016/j.jocn.2010.04.008
S., Ahmad T., Best A., Lansdown C., Hayhurst F., Smeeton S., Davies et al. Spinal epidural lipomatosis: a rare association of Cushing’s disease. Endocrinol Diabetes Metab Case Rep. 2020;2020. https://doi.org/10.1530/edm-20-0111.
N.C. Theyskens, N.R. Paulino Pereira, S.J. Janssen, C.M. Bono, J.H. Schwab, T.D. Cha, The prevalence of spinal epidural lipomatosis on magnetic resonance imaging. Spine J. 17(7), 969–976 (2017). https://doi.org/10.1016/j.spinee.2017.02.010
J.B. Malone, P.J. Bevan, T.J. Lewis, A.D. Nelson, D.E. Blaty, M.E. Kahan, Incidence of spinal epidural lipomatosis in patients with spinal stenosis. J. Orthop. 15(1), 36–39 (2018). https://doi.org/10.1016/j.jor.2017.11.001
G.R. Fogel, P.Y. Cunningham 3rd, S.I. Esses, Spinal epidural lipomatosis: case reports, literature review and meta-analysis. Spine J. 5(2), 202–211 (2005). https://doi.org/10.1016/j.spinee.2004.05.252
P.K. Toshniwal, R.P. Glick, Spinal epidural lipomatosis: report of a case secondary to hypothyroidism and review of literature. J. Neurol. 234(3), 172–176 (1987). https://doi.org/10.1007/bf00314138
H. Fujisawa, M. Hasegawa, O. Tachibana, J. Yamashita, Spinal epidural lipomatosis associated with pituitary macroprolactinoma. Acta Neurochir. 144(2), 213–214 (2002). https://doi.org/10.1007/s007010200028
A.I. Okunlola, T.O. Orewole, C.K. Okunlola, O.F. Babalola, A. Akinmade, Epidural lipomatosis in elderly patient: a rare cause of cauda equina compression. Surg. Neurol. Int 12, 7 (2021). https://doi.org/10.25259/sni_840_2020
P.H. Benamou, P. Hilliquin, N. Chemla, A. Chevrot, C. Cormier, C.J. Menkès, Epidural lipomatosis not induced by corticosteroid therapy. Three cases including one in a patient with primary Cushing’s disease (review of the literature). Rev. Rhum. Engl. Ed. 63(3), 207–212 (1996)
Acknowledgements
The authors would like to thank Dr. Hindi Al-Hindi for preparing the pathology images.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mukhtar, N., Alzahrani, A.S. Spinal epidural lipomatosis: a rare and frequently unrecognized complication of Cushing syndrome. Endocrine 76, 218–223 (2022). https://doi.org/10.1007/s12020-022-03026-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-022-03026-7