Abstract
Purpose
Primary aldosteronism (PA) is the most frequent form of secondary hypertension. Hypertension is a risk factor for cognitive decline and dementia. White matter lesions (WMLs) are linked to vascular risk factors, which increase the risk of dementia. We aimed to analyze the association of PA-related parameters and WMLs in patients with PA.
Methods
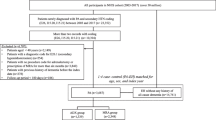
We conducted a retrospective analysis of all patients with PA in the Hypertension Center of the People’s Hospital of Xinjiang Uygur Autonomous Region from January 1, 2011 to April 1, 2021. We analyzed the relationship between plasma aldosterone concentration (PAC), plasma renin activity (PRA), aldosterone–renin ratio (ARR), serum potassium, and WMLs.
Results
We enrolled 138 patients with WMLs and matched these to controls without WMLs at a 1:4 ratio. Among the analytic sample (N = 711) with ages ranging from 30 to 64 years, 69% were male. In the logistic regression analysis, PAC, PRA and serum potassium were treated as continuous variables. The results showed that PAC (OR 1.04, 95% CI 1.01, 1.06, P = 0.008) was positively associated with the risk of WMLs, and serum potassium (OR 0.26, 95% CI 0.16, 0.44, P < 0.001) was inversely associated with the risk of WMLs. PRA (OR 0.86, 95% CI 0.68, 1.08, P = 0.384) was not associated with the risk of WMLs after adjusting for confounders. The results of restricted cubic splines showed the dose-response association between increasing PAC, ARR, decreasing serum potassium, and the risk of WMLs. We also divided PAC, ARR and serum potassium into two groups according to the result of restricted cubic splines. After adjusting for confounders, patients who were in Q2 (≥23.12 ng/dl) of PAC (OR 2.07, 95% CI 1.36, 3.15), Q2 (≥56.81 (ng/dl per ng/ml*h) of ARR (OR 1.82, 95% CI 1.22, 2.72) and Q2 (≤3.58 mmol/l) of serum potassium (OR 2.99, 95% CI 1.95, 4.50) had a significantly higher risk of WMLs than their counterparts. In stratified analyses, there was no evidence of subgroup heterogeneity regarding the change in the risk of WMLs (P > 0.05 for interaction for all).
Conclusion
Our results suggested that the PAC and serum potassium were related to the risk of WMLs in patients with PA. In particular, PAC ≥23.12 ng/dl significantly increased the risk of WMLs in patients with PA.




Similar content being viewed by others
Data availability
We can provide data by e-mail at any time.
References
S. Monticone, J. Burrello, D. Tizzani, C. Bertello, A. Viola, F. Buffolo, L. Gabetti, G. Mengozzi, Prevalence and clinical manifestations of primary aldosteronism encountered in primary care practice. J. Am. Coll. Cardiol. 69(14), 1811–1820 (2017). https://doi.org/10.1016/j.jacc.2017.01.052
J.W. Funder, Primary aldosteronism: present and future. Vitam. Horm. 109, 285–302 (2019). https://doi.org/10.1016/bs.vh.2018.10.006
J.W. Funder, R.M. Carey, F. Mantero, M.H. Murad, M. Reincke, H. Shibata, M. Stowasser, W.F. Young Jr., The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J. Clin. Endocrinol Metab. 101(5), 1889–1916 (2016). https://doi.org/10.1210/jc.2015-4061
M. Parasiliti-Caprino, C. Lopez, N. Prencipe, B. Lucatello, F. Settanni, G. Giraudo, D. Rossato, Prevalence of primary aldosteronism and association with cardiovascular complications in patients with resistant and refractory hypertension. J. Hypertens. 38(9), 1841–1848 (2020). https://doi.org/10.1097/HJH.0000000000002441
M. Reincke, Primary aldosteronism and cardiovascular events: it is time to take guideline recommendations seriously. Hypertension 71(3), 413–414 (2018). https://doi.org/10.1161/HYPERTENSIONAHA.117.10405
V.C. Wu, S.M. Wang, C.H. Chang, Y.H. Hu, L.Y. Lin, Y.H. Lin, S.C. Chueh, L. Chen, K.D. Wu, Long term outcome of aldosteronism after target treatments. Sci. Rep. 6, 32103 (2016). https://doi.org/10.1038/srep32103
S. Monticone, F. D’Ascenzo, C. Moretti, T.A. Williams, F. Veglio, F. Gaita, P. Mulatero, Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 6, 41–50 (2018). https://doi.org/10.1016/S2213-8587(17)30319-4
G.L. Hundemer, G.C. Curhan, N. Yozamp, M. Wang, A. Vaidya, Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: a retrospective cohort study. Lancet Diabetes Endocrinol. 6, 51–59 (2018). https://doi.org/10.1016/S2213-8587(17)30367-4
P.J. Fuller, M.J. Young, Mechanisms of mineralocorticoid action. Hypertension. 46(6), 1227–1235 (2005). https://doi.org/10.1161/01.HYP.0000193502.77417.17
C.A. Northcott, G.D. Fink, H. Garver, J.R. Haywood, E.L. Laimon-Thomson, J.L. McClain, P.W. Pires, W.E. Rainey, C.S. Rigsby, A.M. Dorrance, The development of hypertension and hyperaldosteronism in a rodent model of life-long obesity. Endocrinology. 153(4), 1764–1773 (2012). https://doi.org/10.1210/en.2011-1176
P.W. Pires, J.L. Mclain, S.F. Hayoz, A.M. Dorrance, Mineralocorticoid receptor antagonism prevents obesity-induced cerebral artery remodeling and reduces white matter injury in rats. Microcirculation. 25(5), e12460 (2018). https://doi.org/10.1111/micc.12460
Q.N. Dinh, M.J. Young, M.A. Evans, G.R. Drummond, C.G. Sobey, S. Chrissobolis, Aldosterone-induced oxidative stress and inflammation in the brain are mediated by the endothelial cell mineralocorticoid receptor. Brain Res. 1637, 146–153 (2016). https://doi.org/10.1016/j.brainres.2016.02.034
J.M. Wardlaw, E.E. Smith, G.J. Biessels, C. Cordonnier, F. Fazekas, R. Frayne, R.I. Lindley, J.T. O’Brien et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 12(8), 822–838 (2013). https://doi.org/10.1016/S1474-4422(13)70124-8
M.E. Cahgiuri, P. Peotta, A. Augimeri, F. Rocca, A. Quattrone, A. Cherubini, Automatic detection of white matter hyperintensities in healthy aging and pathology using magnetic resollauce knagmg: a review. Neuromformatics 13(31), 261–276 (2015). https://doi.org/10.1007/s1202l-015.9260-v
A.H. Hainsworth, J. Miner T’Andoh, G. Forster, I. Bhide, T.R. Barrick, K. Elderfield, J. Jeevahan, H.S. Markus, L.R. Bridges, Neuropathology of white matter lesions, blood-brain barrier dysfunction, and dementia. Stroke 48(10), 2799–2804 (2017). https://doi.org/10.1161/STROKEAHA.117.018101
Y.P. Coutu, A. Goldblatt, I.-I.D. Rosas, D.H. Rosas, Alzheimer’s Disease Neuroimaging Initiative (ADNI), White matter changes are associated with ventricular expansion in aging, mild cognitive impairment, and Alzheimer’s disease. J. AIzheimers Dis. 49(2), 329–342 (2016). 10.3233HAD-150306.
L. Wang, C.O. Leonards, P. Sterzer, M. Ebinger, White matter lesions and depression: a systematic review and meta-analysis. J. Psychiatr. Res. 56, 56–64 (2014). https://doi.org/10.1016/j.jpsychires.2014.05.005
L.H. Kuller, W.T. Longstreth, A.M. Arnold, C. Bernick, R.N. Bryan, N.J. Beauchamp, White matter hyperintensity on cranial magnetic resonance imaging: a predictor of stroke. Stroke 35, 1821–1825 (2004). https://doi.org/10.1161/01.STR.0000132193.35955.69
L. Pantoni, Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 9(7), 689–701 (2010). https://doi.org/10.1016/S1474-4422(10)70104-6
L. Wolfson, D.B. Wakefield, N. Moscufo, R.F. Kaplan, C.B. Hall, J.A. Schmidt, C.R. Guttmann, W.B. White, Rapid buildup of brain white matter hyperintensities over 4 years linked toambulatory blood pressure, mobility, cognition, and depression in old persons. J. Gerontol. A Biol. Sci. Med. Sci. 68(11), 1387–1394 (2013). https://doi.org/10.1093/gerona/glt072
C.J. McNeil, P.K. Myint, A.L. Sandu, J.F. Potter, R. Staff, L.J. Whalley, A.D. Murray, Increased diastolic blood pressure is associated with MRI biomarkers of dementia-related brain pathology in normative ageing. Age Ageing 47, 95–100 (2018). https://doi.org/10.1093/ageing/afx102
B.S. Aribisala, Z. Morris, E. Eadie, A. Thomas, A. Gow, M.C. V aldés Hernández, N.A. Royle, M.E. Bastin, Blood pressure, internal carotid artery flow parameters, and age-related white matter hyperintensities. Hypertension 63, 1011–1018 (2014). https://doi.org/10.1161/HYPERTENSIONAHA.113.02735
M. Shokouhi, D. Qiu, A. Samman Tahhan, A.A. Quyyumi, I. Hajjar, Differential associations of diastolic and systolic pressures with cerebral measures in older individuals with mild cognitive impairment. Am. J. Hypertens. 31, 1268–1277 (2018). https://doi.org/10.1093/ajh/hpy104
J.F. Meschia, C.D. Bushnell, B. Boden-Albala, L.Y. Braun, D.M. Bravata, S. Chaturvedi, J.F. Meschia, C. Bushnell, B. Boden-Albala, L.T. Braun, D.M. Bravata, S. Chaturvedi, M.A. Creager, R.H. Eckel, M.S. Elkind, M. Fornage, L.B. Goldstein, S.M. Greenberg, S.E. Horvath, C. Iadecola, E.C. Jauch, W.S. Moore, J.A. Wilson; American Heart Association Stroke Council; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Functional Genomics and Translational Biology; Council on Hypertension, Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 45, 3754–3832 (2014). https://doi.org/10.1161/STR.0000000000000046
K.A. Walker, A.R. Sharrett, A. Wu, A.L.C. Schneider, M. Albert, P.L. Lutsey, K. Bandeen-Roche, J. Coresh, A.L. Gross, B.G. Windham, D.S. Knopman, M.C. Power, A.M. Rawlings, T.H. Mosley, R.F. Gottesman, Association of midlife to late-life blood pressure patterns with incident dementia. JAMA 322, 535–545 (2019). https://doi.org/10.1001/jama.2019.10575
J.W. Funder, R.M. Carey, F. Mantero, M.H. Murad, M. Reincke, H. Shibata, M. Stowasser, W.F. Young Jr., The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 101(5), 1889–1916 (2016). https://doi.org/10.1210/jc.2015-4061
X. Wang, Q. Luo, M. Wang, J. Hu, D. Zhang, W. Zhang, G. Wang, N. Li, Long-term impact of spironolactone compliance on microalbuminuria in patients with primary aldosteronism. Hypertens Res. 44(4), 426–434 (2021). https://doi.org/10.1038/s41440-020-00589-8
Q. Luo, N. Li, M. Wang, X. Yao, M. Heizhati, D. Zhang, K. Zhou, G. Wang, J. Hu, B. Zhu, Mild primary aldosteronism (PA) followed by overt PA are possibly the most common forms of low renin hypertension: a single-center retrospective study. J. Hum. Hypertens. 34(9), 633–640 (2020). https://doi.org/10.1038/s41371-019-0291-y
Q. Luo, N.F. Li, X.G. Yao, D.L. Zhang, S.F. Abulikemu, G.J. Chang, K.M. Zhou, G.L. Wang, M.H. Wang, W.J. Ouyang, Q.Y. Cheng, Y. Jia, Potential effects of age on screening for primary aldosteronism. J. Hum. Hypertens. 30(1), 53–61 (2016). https://doi.org/10.1038/jhh.2015.21
F. Beygui, G. Montalescot, E. Vicaut, S. Rouanet, E. Van Belle, C. Baulac, A. Degrandsart, J. Dallongeville; OPERA Investigator, Aldosterone and long-term outcome after myocardial infarction: a substudy of the French nationwide observatoire sur la prise en charge hospitalière, l’Evolution à un an et les caRactéristiques de patients présentant un infArctus du myocarde avec ou sans onde Q (OPERA) study. Am. Heart J. 157, 680–687 (2009). https://doi.org/10.1016/j.ahj.2008.12.013
F. Ivanes, S. Susen, F. Mouquet, P. Pigny, F. Cuilleret, K. Sautière, J.P. Collet, F. Beygui, B. Hennache, P.V. Ennezat et al. Aldosterone, mortality, and acute ischaemic events in coronary artery disease patients outside the setting of acute myocardial infarction or heart failure. Eur. Heart J. 33, 191–202 (2012). https://doi.org/10.1093/eurheartj/ehr176
S. Monticone, F. D’Ascenzo, C. Moretti, T.A. Williams, F. Veglio, F. Gaita, P. Mulatero, Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 6, 41–50 (2018). https://doi.org/10.1016/S2213-8587(17)30319-4
S. Keidar, M. Kaplan, E. Pavlotzky, R. Coleman, T. Hayek, S. Hamoud, M. Aviram, Aldosterone administration to mice stimulates macrophage NADPH oxidase and increases atherosclerosis development. Circulation. 109, 2213–2220 (2004). https://doi.org/10.1161/01.CIR.0000127949.05756.9D
A.P. McGraw, J. Bagley, W.S. Chen, C. Galayda, H. Nickerson, A. Armani, M. Caprio, P. Carmeliet, I.Z. Jaffe, Aldosterone increases early atherosclerosis and promotes plaque inflammation through a placental growth factor-dependent mechanism. J. Am. Heart Assoc. 2, e000018 (2013). https://doi.org/10.1161/JAHA.112.000018
P.W. Pires, W.F. Jackson, A.M. Dorrance, Regulation of myogenic tone and structure of parenchymal arterioles by hypertension and the mineralocorticoid receptor. Am. J. Physiol. Heart Circ. Physiol. 309(1), H127–H136 (2015). https://doi.org/10.1152/ajpheart.00168.2015
A.M. Dorrance, N.C. Rupp, E.F. Nogueira, Mineralocorticoid receptor activation causes cerebral vessel remodeling and exacerbates the damage caused by cerebral ischemia. Hypertension. 47(3), 590–595 (2006). https://doi.org/10.1161/01.HYP.0000196945.73586.0d
P. Verpillat, A. Alpérovitch, F. Cambien, V. Besançon, H. Desal, C. Tzourio, Aldosterone synthase (CYP11B2) gene polymorphism and cerebral white matter hyperintensities. Neurology 56(5), 673–675 (2001). https://doi.org/10.1212/wnl.56.5.673
P.J. Fuller, K. Verity, Mineralocorticoid receptor gene expression in the gastrointestinal tract: distribution and ontogeny. J. Steroid. Biochem. 36(4), 263–267 (1990). https://doi.org/10.1016/0022-4731(90)90215-e
P.J. Fuller, J. Yang, M.J. Young, Mechanisms of mineralocorticoid receptor signaling. Vitam. Horm. 109, 37–68 (2019). https://doi.org/10.1016/bs.vh.2018.09.004
T.M. De Silva, M.L. Modrick, J.L. Grobe, F.M. Faraci, Activation of the central renin-angiotensin system causes local cerebrovascular dysfunction. Stroke. 52(7), 2404–2413 (2021). https://doi.org/10.1161/STROKEAHA.121.034984
J.M. Diaz-Otero, C. Fisher, K. Downs, M.E. Moss, I.Z. Jaffe, W.F. Jackson, A.M. Dorrance, Endothelial mineralocorticoid receptor mediates parenchymal arteriole and posterior cerebral artery remodeling during angiotensin II-induced hypertension. Hypertension. 70(6), 1113–1121 (2017). https://doi.org/10.1161/HYPERTENSIONAHA.117.09598
P.W. Pires, J.L. McClain, S.F. Hayoz, A.M. Dorrance, Mineralocorticoid receptor antagonism prevents obesity-induced cerebral artery remodeling and reduces white matter injury in rats. Microcirculation 25(5), e12460 (2018). https://doi.org/10.1111/micc.12460
L.S. Johnson, N. Mattsson, A. Sajadieh, P. Wollmer, M. Söderholm, Serum potassium is positively associated with stroke and mortality in the large, population-based malmö preventive project cohort. Stroke 48(11), 2973–2978 (2017). https://doi.org/10.1161/STROKEAHA.117.018148
F. Matano, Y. Fujiki, T. Mizunari, K. Koketsu, T. Tamaki, Y. Murai, H. Yokota, A. Morita, Serum glucose and potassium ratio as risk factors for cerebral vasospasm after aneurysmal subarachnoid hemorrhage. J. Stroke Cerebrovasc. Dis. 28(7), 1951–1957 (2019). https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.03.041
B.E. Grueter, U.G. Schulz, Age-related cerebral white matter disease (leukoaraiosis): a review. Postgrad. Med. J. 88(1036), 79–87 (2012). https://doi.org/10.1136/postgradmedj-2011-130307
D. Fuhrmann, D. Nesbitt, M. Shafto, J.B. Rowe, D. Price, A. Gadie, C. CAN, R.A. Kievit, Strong and specifific associations between cardiovascular risk factors and white matter micro- and macrostructure in healthy aging. Neurobiol. Aging 74, 46–55 (2019). https://doi.org/10.1016/j.neurobiolaging.2018.10.005
C. Annweiler, T. Annweiler, R. Bartha, F.R. Herrmann, R. Camicioli, O. Beauchet, Vitamin D and white matter abnormalities in older adults: a cross-sectional neuroimaging study. Eur. J. Neurol. 21(12), 1436–e95 (2014). https://doi.org/10.1111/ene.12511
O. Godin, C. Tzourio, P. Maillard, B. Mazoyer, C. Dufouil, Antihypertensive treatment and change in blood pressure are associated with the progression of white matter lesion volumes: the Three-City (3C)-Dijon Magnetic Resonance Imaging Study. Circulation 123(3), 266–273 (2011). https://doi.org/10.1161/CIRCULATIONAHA.110.961052
M.R. Caunca, M. Simonetto, Y.K. Cheung, N. Alperin, S.H. Lee, M.S.V. Elkind, R.L. Sacco, T. Rundek, Diastolic blood pressure is associated with regional white matter lesion load: the Northern Manhattan Study. Stroke. 51(2), 372–378 (2020). https://doi.org/10.1161/STROKEAHA.119.025139
Funding
National Health Committee Key Laboratory of Hypertension Clinical Research.
Author information
Authors and Affiliations
Contributions
Y.Y. carried out statistical analysis, prepared original manuscript, and revised the submission. N.L. conceived and designed the present study. Y.L., M.W., M.H., Q.Z., X.Y., and Q.L. participated in controlling the quality of cases. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Consent for publication
Yes
Ethics approval
The study was approved by the Ethics Committee of People’s Hospital of Xinjiang Uygur Autonomous Region. Due to retrospective nature of the study and use of anonymized data, we waived need for informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yuan, Y., Li, N., Liu, Y. et al. Plasma aldosterone concentration is associated with white matter lesions in patients with primary aldosteronism. Endocrine 75, 889–898 (2022). https://doi.org/10.1007/s12020-021-02920-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-021-02920-w